Abstract
Introduction Patient worry and concern of cancer adds to the latent distress associated with referral on the two-week suspected pathway (2WW). For oral cancer, as the conversion rate is in the region of 5-10%, the majority of people will have needless cause for concern.
Aim This study aims to report how worried/concerned patients were that the reason for referral might mean that they had cancer and to relate to referral characteristics.
Materials/methods All patients referred on the 2WW to two oral and maxillofacial departments in the three months from January to March 2021 were sent a one-off anonymised study-specific post-consultation survey.
Results In total, 107 of 353 patients responded to the survey (30%). The response rate increased notably in the older group (p <0.001). The cancer conversion rate overall was 5.4% (19/353), stratified as 2.4% (4/167) for general dental practitioner and 8.1% (15/186) for general medical practitioner (p = 0.02). When asked how worried/concerned they were that the reason for referral might have been for cancer, the response was 'very much' (34%, 33/98), and 'somewhat' (24%, 24/98). Concerns tended to be higher in women and those under 40.
Conclusions In recognition of the proportion of patients on the 2WW pathway without cancer who have 'very much worry and concern', it is appropriate to explore ways to alleviate this anxiety, and the best means to achieve this needs careful consideration.
Key points
-
Most patients referred on the two-week suspected pathway do not have cancer and should be given reassuring information around the reason for referral.
-
There is the potential for high levels of worry and concern for those on the two-week suspected pathway.
-
Patients should be seen without undue delay in order to reduce the delay to cancer diagnosis and also minimise the time of anxiety in the worried.
Similar content being viewed by others
Introduction
The two-week suspected cancer pathway (2WW) is a well-established mechanism for the referral of patients suspected of having possible malignancy. It was introduced in 2000, with the aim of promoting early referral and minimising delay in those patients with signs and symptoms that could denote an underlying neoplasia.1,2 The National Institute for Health and Care Excellence (NICE) published national guidelines for primary healthcare professionals in 2005 and an update in 2015, outlining guidance on the signs and symptoms of head and neck cancers.3 For suspected head and neck cancer, the conversion rate is in the region of 5-10%; hence, most patients assessed do not have cancer.4
Departments in secondary care are performance managed against the proportion of patients seen within the two weeks. From a clinical perspective, in the context of the 62-day treatment pathway, the capability to deliver a first consultation within two weeks places a considerable burden on clinic capacity and might appear extremely short. However, from the patient's perspective, two weeks might be viewed as a wait, especially those worrying about the potential diagnosis and the consequences if diagnosed with cancer. It has been recognised for many years that women referred with possible breast cancer do experience considerable anxiety in the period between noting a breast symptom and diagnosis.5 Cornford and co-workers reported that patients experienced significant distress while waiting to be seen within the 'two-week rule' for suspected breast carcinoma.6 For those referred on the two-week rule for suspected colorectal cancer, participants reported anxiety, fear and vulnerability.7 As part of this pathway, general practitioners are advised to inform their patients that they are being referred on the 2WW. How this is explained and framed could potentially enhance levels of anxiety. There is a paucity of evaluation in those referred for suspected head and neck cancer and a better understanding could help inform guidelines, training and future research.3 Hence, the aims of this study were to report how worried/concerned patients were that the reason for referral might mean that they had cancer and to relate this to referral characteristics.
Methods
All patients referred to Aintree University Hospital and Arrowe Park Hospital in North West England during the three months from January to March 2021 were sent a post-consultation survey. The letters were sent in April 2021. The mailing also included a covering letter explaining the reason for the survey, saying that it was to help give insight into the referral process from the doctor or dentist and that the aim was to improve services and provide better care for patients. The letter stressed that the survey was anonymous and voluntary and a pre-paid return envelope was also included. Participants consented to participate in the study and to have their data used as part of the research. The audit department approved an anonymous postal survey with no reminders to be sent. Audit approval was received from Aintree (10144) and Arrowe Park (CA0014).
The survey was adapted from one used in primary medical practice and was modified after an informal pilot in a few patients attending clinic.8Personal questions were kept to a minimum and most of the questionnaire comprised of tick-box response options. There were questions about the reason for the referral, such as where their problem was located and what their symptoms were. There were separate similar sections relating to doctor (general medical practitioner [GMP]) and dentist (general dental practitioner [GDP]) with questions asking about how many times they had spoken with this health professional before being referred, what advice or prescribing they were given before referral, whether the referral had been 'just in case' cancer might be suspected and how worried/concerned they were that the reason for referral might have been because of cancer. Patients were also asked what the professionals involved could have done differently to improve their experience. A series of five-point Likert scale questions were included.
Clinical and demographic data comprised hospital location, sex, age, the source of referral (GDP, GMP), referral date and the result of the referral (cancer, no cancer). Data obtained from hospital sources and from the returned paper questionnaires were manually transcribed into an Excel database which was then imported into IBM SPSS Statistics v25. Fishers exact test was used to compare between distinct subgroups of referred patients/survey respondents in regard to the clinical and demographic data collected, with statistical significance at the 5% level. SPSS v25 and STATA v13 were used for data management and statistical analysis. A small number of responders did not answer all questions and hence denominators vary slightly from question to question.
Results
The response rate was 30% (107/353). Characteristics of all patients and of responders are shown in Table 1. The response rate increased notably with age (p <0.001). The head and neck cancer conversion rate overall was 5.4% (19/353), stratified as 2.4% (4/167) for GDP and 8.1% (15/186) for GMP (p = 0.02). For patients aged under 40 years, the conversion rate was 0% (0/76), while for those aged 40-59 it was 7.2% (9/125) and for those aged 60 and over it was 6.4% (10/156). The median (interquartile rage) age of referred patients was 58 (45-71) for GDP referrals and 55 (41-67) for GMP referrals. Descriptive results from survey respondents are shown in Table 2.
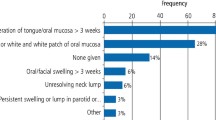
There was a tendency (Table 3) before referral for general practitioner (GP)-referred patients to speak more than once to a GP (18/40) than dentist-referred patients to speak more than once to a dentist (11/44). There was no dominant form of advice or treatment offered to the patient before referral in either referral group. There was no 'nothing' option offered to patients on the survey and many within the 'not known' category who left this question blank might possibly have answered 'nothing' if that category had existed. Overall, when asked if the referral had been made 'just in case' the reason for referral might have been for cancer, 58% (62/107) said 'yes', 9% (10/107) said 'no', while this was not known for 33% (35/107), When asked how worried/concerned they were that the reason for referral might have been for cancer, the response was 'very much' (34%, 33/98), 'somewhat' (24%, 24/98), 'undecided' (12%, 12/98), 'not really (15%, 15/98) or 'not at all' (14%, 14/98). It was observed (Table 4) that the percentage of patients who were very much or somewhat worried/concerned was higher in women (vs men) and in those aged under 40, but was somewhat lower in those aged 80 years and over. The only statistically significant difference noted (p = 0.02) was the percentage to be higher in those who felt the referral was made was because of cancer (67%) and lower in those who felt this was not the reason (22%).
The final survey free-text question asked patients to say what the professionals could have done differently to improve their experience. There were 86 responses to this question, of which the majority (83%, 71) were simply positive and largely thankful in their tone and they did not make any suggestions as to how things might have been done differently. There were 15 responses that were either neutral or negative in tone and these are listed in Box 1.
Discussion
The two-week pathway is embedded into patient care and is an important link between primary and secondary care to help facilitate the timely diagnosis of cancer. Primary dental care has a critical role in the pathways. Departments are configured to be able to assess most referrals within the two-week time frame. This enables minimal delay from referral to the request of appropriate investigations and treatment. There is evidence in other cancers that suggests high levels of anxiety and distress for those suspected of cancers.5,6,7 Thus, in terms of patient experience, as the majority referred don't have cancer, the sooner they can be reassured the better. This current study is novel in oral cancer referrals and provides evidence regarding the referral characteristics and levels of worry and concern. Although it is necessary to be circumspect regarding the findings of this survey given the low response rate, the study does serve to raise awareness of this important issue. The study was undertaken as an 'audit' and the constraint was for an anonymous survey with no reminders to non-responders. Although the survey was piloted in an attempt to reduce patient questionnaire burden and interpretability, it might have been somewhat complicated and hard to follow. It would be speculative to consider if those more anxious were less or more likely to respond. It is notable that younger patients were less likely to respond and these were also most likely to have lower risk of having head and neck cancer. Another limitation is the small sample size collected from these two departments in the North West. The proportion of those worried/concerned might be different in other geographical locations. Also, as the survey was undertaken during the ongoing COVID-19 pandemic, this could add to patients' anxiety for a hospital visit. In addition, the referral base was to oral and maxillofacial and thus the majority of sites pertained to the oral cavity. It might be that levels of worry and concern are slightly different in other sites, such as oropharynx and larynx and on the head and neck 2WW, such patients are triaged to be seen in the ear, nose and throat (ENT) department. As a limited 'audit', it was not possible to add additional questionnaires such as to measure anxiety using the Hospital Anxiety and Depression Scale.
The overall conversion rate was just over 5% and emphasises that the majority on the pathway do not have cancer and for a short time are the 'worried well'. It is not unreasonable to expect patients to be anxious when told that they are being referred on an urgent suspected cancer pathway. A level of worry and concern can be protective as there is evidence that patients with early cancers are more anxious and seek consultation sooner.9 In terms of referral, it is notable that although many symptoms were related to the mouth and the majority of responders said they were regular attenders at a GDP, around half of the referrals came from the GP. This could hint at the possible merit of expeditious review by the patient's own GDP as a way to reduce the number of referrals and ally concerns without missing any cancers or causing undue delay. About half were referred after one appointment and over half recognised that they were being referred 'just in case' it was cancer. In spite of this, 58% reported 'very much' or 'somewhat worried/concerned'. Even on those groups where the rate of oral cancer is very low, such as women and those under 40, the study reveals the potential for high levels of worry. In those giving feedback about what the professionals could have done differently to improve patient experience, some mentioned improved communication and although small numbers, it might be more of an issue to patients' experience in secondary care. Unfortunately, in this current study, it was not possible to explore the way the patient was informed about the nature of the referral, the context and the advice given. Perhaps those with low-risk signs and symptoms ('red flags') could be reassured by early telephone triage, thus attempting to reduce the distress in those referred 'just in case'. Communications have been highlighted as an issue in suspected breast cancer and colorectal cancer.6,7 The UK NICE referral guidelines emphasise that the patient should be involved in the decision-making process and be informed of the reasons for referral.10
Conclusion
In conclusion, in the context of possible cancer, it is a challenge to provide the optimum patient experience. There are relatively high levels of worry and concern in a group where cancer conversion rates are low. There is an imperative to streamline the service and explore ways to reduce two-week suspected cancer pathway anxiety.
References
UK Government. The new NHS: modern, dependable. 1997. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/266003/newnhs.pdf (accessed June 2022).
Department of Health. The NHS Cancer Plan: A plan for investment, a plan for reform. 2000. Available at https://www.thh.nhs.uk/documents/_Departments/Cancer/NHSCancerPlan.pdf (accessed June 2022).
National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. 2015. Available at https://www.nice.org.uk/guidance/ng12/resources/suspected-cancer-recognition-and-referral-pdf-1837268071621 (accessed June 2022).
Metcalfe C, Dailey Y, Lowe D, Rogers S N. Introduction of a referral pathway guide for general dental practitioners in Cheshire & Merseyside: the effect on two-week suspected cancer referrals. Br Dent J 2019; 227: 1058-1062.
Northouse L L, Jeffs M, Cracchiolo-Caraway A, Lampman L, Dorris G. Emotional distress reported by women and husbands prior to a breast biopsy. Nurs Res 1995; 44: 196-201.
Cornford C, Oswald N. The 2-week rule for patients with suspected breast cancer: what can be learnt by analysing policy documents? Health Policy 2004; 68: 263-266.
Ndukwe N, Borowski D W, Lee A, Orr A, Dexter-Smith S, Agarwal A K. The two-week rule for suspected colorectal cancer. Int J Health Care Qual Assur 2012; 25: 75-85.
Talwar C, McClune A, Kelly D, Lowe D, Rogers S N. Two-week rule: suspected head and neck cancer referrals from a general medical practice perspective. Br J Oral Maxillofac Surg 2020; 58: 981-985.
Rozniatowski O, Reich M, Mallet Y, Penel N, Fournier C, Lefebvre J-L. Psychosocial factors involved in delayed consultation by patients with head and neck cancer. Head Neck 2005; 27: 274-280.
Banks J, Walter F, Hall N, Mills K, Hamilton W, Turner K. Decision making and referral from primary care for possible lung and colorectal cancer: a qualitative study of patients' experiences. Br J Gen Pract 2014; DOI: 10.3399/bjgp14X682849.
Acknowledgements
We acknowledge with thanks the patients who completed the survey.
Author information
Authors and Affiliations
Contributions
Catherine E. P. Rowlands: conception and design of study/review/case series; acquisition of data: laboratory or clinical/literature search; analysis and interpretation of data collected; drafting of article and/or critical revision. Peter James: acquisition of data: laboratory or clinical/literature search; drafting of article and/or critical revision. Derek Lowe: conception and design of study/review/case series; analysis and interpretation of data collected; drafting of article and/or critical revision. Simon N. Rogers: drafting of article and/or critical revision; final approval and guarantor of manuscript.
Corresponding author
Ethics declarations
We have no conflicts of interest. The data was collected for service evaluation and approved by the local Clinical Governance Department.
Rights and permissions
About this article
Cite this article
Rowlands, C., James, P., Lowe, D. et al. Patient worry and concern associated with referral on the two-week suspected head and neck pathway. Br Dent J (2022). https://doi.org/10.1038/s41415-022-4444-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-4444-y