Abstract
Objective To compare the clinical effectiveness and cost benefit of different frequencies of scale and polish (S&P) treatments in combination with different types of oral hygiene advice (OHA).
Design Multi-centre, multi-level cluster randomised factorial open trial with blinded outcome evaluation. UK dental practices were cluster randomised to deliver OHA as usual or personalised. In a separate randomisation, patients were allocated to receive S&P 6-monthly, 12-monthly or never.
Setting UK primary dental care.
Participants Practices providing NHS care and adults who had received regular dental check-ups.
Main outcome measures The percent of sites with bleeding on probing, patient confidence in self-care, incremental net benefits (INB) over three years.
Results Sixty-three practices and 1,877 adult patients were randomised and 1,327 analysed (clinical outcome). There was no statistically significant or clinically important difference in gingival bleeding between the three S&P groups (for example, six-monthly versus none: difference 0.87% sites, 95% CI: 1.6 to 3.3, p = 0.48) or between personalised or usual OHA groups (difference -2.5% sites, -95%CI: -8.3 to 3.3, p = 0.39), or oral hygiene self-efficacy (cognitive impact) between either group (for example, six-monthly versus none: difference -0.028, 95% CI -0.119 to 0.063, p = 0.543). The general population place a high value on, and are willing to pay for, S&P services. However, from a dental health perspective, none of the interventions were cost-effective.
Conclusion Results suggest S&P treatments and delivering brief personalised OHA provide no clinical benefit and are therefore an inefficient approach to improving dental health (38% of sites were bleeding whatever intervention was received). However, the general population value both interventions.
Key points
-
Describes the process of successfully delivering a multi-centre, cluster randomised factorial open trial in general dental practice in the NHS, for the most frequently provided dental treatment, scale and polish (S&P), and oral hygiene advice.
-
Highlights the clinical, economic and patient-centred outcomes from providing S&P at different time intervals alongside personalised or routine oral hygiene advice to over 2,000 participants for three years.
-
Evidence from IQuaD concludes that there was no difference in gingival bleeding across trial arms at three years; however, the general population are willing to pay for and place a high value on both S&P and personalised oral hygiene advice.
Similar content being viewed by others
Introduction
The authors of this publication reflect on the original report for the NIHR HTA IQuaD Trial and provide an insight into the trial and the findings, which are particularly relevant in the COVID-19 era.1
Periodontal disease is preventable, yet it remains the major cause of poor oral health worldwide, which in turn is responsible for loss of teeth and susceptibility to oral pathogen-related systemic diseases.2,3,4,5,6 In 2010, the global annual cost for the management of severe periodontal disease was estimated to be $54 billion.7 However, the spend for prevention and maintenance will likely be far higher.
The disruption or removal of the biofilm is a key component for the prevention of periodontal disease.8,9 The evidence-based way of doing so is through sustained good oral hygiene; however, the impact/contribution made by dental professionals is uncertain.10 Scale and polish (S&P), often referred to as periodontal instrumentation (PI), is the most frequently performed dental intervention in the world provided at considerable cost. In the United Kingdom (UK), S&Ps account for over a third of all the NHS dental treatments provided in primary care. During 2018/19 in Scotland alone, 2.2 million claims were made at a cost of £31 million to the NHS and patients.11,12 Patients across the UK also pay a proportion of the cost of S&P treatment. Nevertheless, there is a remarkable lack of reliable evidence to inform policymakers and dental professionals of the optimal oral hygiene advice (OHA) format and of the optimal frequency of providing the S&P treatment.13
The objectives of the IQuaD study were to compare the clinical effectiveness, the impact on oral hygiene self-confidence, and incremental net benefits of different types of OHA in combination with different frequencies of the S&P treatment.
IQuaD was a multi-centre, multi-level cluster factorial open trial with blinded outcome evaluation.14 Dental practices were cluster randomised so that all dental professionals within practices delivered OHA as they usually did (usual) or in a format tailored to the needs of their patients (personalised) within the current appointment scheduling. In a separate randomisation, participating patients, regardless of their dental practice, were scheduled to receive the S&P treatment 6-monthly or 12-monthly or not at all during three-year follow-up.
Methods
Participants
IQuaD had two types of participants: the dental teams (dentists/hygienists) providing care within dental practices and their patients. Dental teams were participants because they were allocated to receive or not receive training to deliver an oral hygiene advice intervention. Patients were participants because they were allocated to different frequencies of S&P. We included UK NHS dentists and hygienists and adults with at least one tooth who attended the dental practice in the two years before recruitment. Because one of the interventions for patients was no S&P for three years, we excluded patients with potentially more serious periodontal disease (periodontitis and, or a BPE score of 4) and those with an uncontrolled chronic medical condition (for example, diabetes, immunocompromised).
Participating NHS dental practices represented practitioners operating in Scotland and North East England (Newcastle) in a range of different circumstances (for example, urban or rural, high-, middle- or low-income communities, employing or not employing a dental hygienist).
Randomisation and blinding
We used an automated computer-generated randomisation algorithm at the Centre for Healthcare Randomised Trials (CHaRT), University of Aberdeen, UK to allocate the randomised group (personalised OHA versus usual) to practices (clusters) and we did the same for patients within practices (no S&P, 12-monthly, and 6-monthly). We randomised dental practices to give personalised OHA versus usual and not patients, due to the risk of contamination, that is, general dental practitioners (GDPs) would have to switch between giving an educational intervention or not and we considered this to be difficult; patients that go to the same practice might communicate outside the practice about the advice received. Delivering the S&P treatment entailed no such risk.
Trial outcome assessor (OA) teams, dental hygienists and nurses employed by the trial, attended recruitment sessions in participating dental practices and consented potentially eligible participants that had been screened by GDPs.
We minimised randomisation based on the following variables: for the practices, employs dental hygienist versus doesn't, has three or more dentists versus two or less; for the patients, absence of gingival bleeding on probing versus any bleeding on probing, highest BPE score 3 versus 2 or less and currently smoking versus not.
Written consent for the dental practice (cluster) to take part in the trial was provided by the principal dentists (usually the owner of the practice) before cluster randomisation. The practice allocation was concealed from GDPs until training in the trial and intervention as appropriate had been given by a member of the trial team. The participant allocation was concealed until after baseline S&P had been provided by the dental practitioner. The OA teams remained blinded throughout the trial.
Study interventions
Details of interventions and their theoretical underpinning are described in the published protocol.15 In summary, the personalised OHA intervention was framed using Social Cognitive Theory and Implementation Intention Theory.16,17 The content of this advice was personalised according to patient needs. At a minimum the content included advice and instruction in self-diagnosis and self-care (tooth brushing and interdental cleaning), as well as an agreed-on action plan for performing self-care with the patient. Training in the delivery of the personalised OHA intervention was provided to all dentists/hygienists within a dental practice randomised to this allocation by a clinical member of the trial team. The content and the delivery of the intervention was standardised as a series of steps designed to take place within an average primary care consultation, taking approximately 5 minutes in total.
This was a pragmatic trial and was focusing on interventions/treatments already being used in general practice. Usual OHA was therefore defined as the OHA currently being provided by the practices. There is no published information describing 'usual' OHA, but anecdotal evidence suggests that this is often the provision of minimal advice (for example, 'you need to brush your teeth more frequently') or no advice at all.
Similarly, the definition of S&P was as used in standard practice and could include the removal of plaque and calculus from the crown and root surfaces using manual or ultrasonic scalers and the appropriate management of plaque retention factors, but no adjunctive sub-gingival therapy, for example, local delivery antibiotics. No time limit was set on this treatment and dentists/hygienists were instructed to scale the teeth and root surfaces until they were free of all deposits and were smooth to probing.
Participating dental practices were advised that all patient participants, regardless of group, should be invited to a routine dental check-up at least every 12 months. All participants received a S&P at baseline.
Outcome measures
Clinical outcomes were recorded by blinded OAs at baseline and three years. Training was provided to ensure intra- and inter-assessor alignment.18 Participant reported outcomes were collected at baseline and annually by self-administered postal questionnaires. The primary clinical outcome was bleeding at the gingival margin measured by running a University of North Carolina probe circumferentially around each tooth just within the gingival sulcus or pocket.19 After 30 seconds, bleeding was recorded as being present or absent on the buccal and lingual surface and reported as the percentage of sites (twice the number of teeth) with bleeding.
Oral hygiene self-efficacy (cognitive impact) was the primary patient-reported outcome and was collected annually by self-administered postal questionnaires issued to patient participants and measured on a 7-point scale (1 being not at all confident to 7 being extremely confident). The primary economic outcome was incremental net benefits (INB).
Secondary outcomes were calculus and clinical probing depth, patient-reported dental quality of life,20 oral health behaviour and intention, additional private scale and polish treatments, and referral. Dental professionals' beliefs relating to providing oral hygiene advice and their perceived ability to maintain their patients' periodontal health were collected at three years. Details on the assessment of secondary outcomes are provided in the published trial monograph.1
Trial oversight
A Periodontal Advisory Group provided expert clinical advice. The trial was overseen by a Trial Steering Committee (TSC) and an independent Data and Safety Monitoring Committee. A Project Management Group took responsibility for the accuracy and completeness of the data, analyses and reporting, and for the fidelity of the study to the protocol.
Patient and public involvement
Prior to the start of the IQuaD trial, patients were involved with the trial design and provided invaluable feedback on trial recruitment and communication strategies. Patients also contributed to the content and layout of the trial invitation, trial newsletters and the design of patient participant questionnaires. Members of the public also contributed to trial oversight through membership of the TSC, including helping to interpret the trial findings and preparation of the monograph. Patient and public involvement representatives were also involved in designing a leaflet for dissemination of trial results to the participants.
Statistical analysis
We analysed the pre-specified comparisons of no S&P versus 6-monthly, 12-monthly versus 6-monthly, and personalised versus usual OHA according to an intention-to-treat framework. The primary analysis was performed when all participants had completed the three-year follow-up, conducted according to a pre-specified statistical plan (available upon request).
We used the appropriate mixed effects model depending on the outcome distribution and included a random effect for practice in outcomes collected at three years - and a random effect for practice and for patient in outcomes collected at year 1, 2 and 3. Models were adjusted for minimisation variables and, where available, for baseline measures. An interaction factor between the two interventions (S&P and OHA) was included. Subgroup analyses explored the possible modification of treatment effect by factor, by including a treatment-by-factor interaction in models with the corresponding 99% confidence interval. We conducted pre-specified subgroup analyses for the primary outcome by smoking status (yes/no), BPE score (<3 or 3), age group (<45 years old/45-64/>64), employment of a hygienist in the practice (yes/no). Post-hoc subgroup analyses were undertaken by number of sites with a deeper probing depth (four or more sites with a clinical probing depth of ≥4 mm [yes/no]) and country (Scotland/England).
We compared variables collected at baseline by missing primary outcome status (participants with and without missing data) and using t-test and chi-squared tests.
Routine treatment data were obtained from Information Services Division Scotland and the NHS Business Services Authority in England from the time periods of 2010-2016. They provided the number of treatment claims for S&P made by dentists for each participant.
The planned sample size was 1,248 patients and 50 practices (clusters) with 25 patients each and intracluster correlation of 0.05. We aimed to recruit 208 patients in each S&P group and 416 across OHA groups. This resulted in more than 95% power to detect a 7.5% difference in gingival bleeding (considered clinically meaningful) and 90% power to detect the same difference between the two OHA groups. This sample size assumes no interaction between interventions. If there was an interaction, assuming an ICC of 0.05, the trial had 80% power to detect an interaction effect of 7.5%. To account for 17% attrition at the practice level and 20% at the participant level, we aimed to recruit 60 practices and 1,860 participants. Each dentist was required to recruit on average 31 participants to ensure 25 at follow-up.
For patient-reported outcomes, a third of a standard deviation difference between groups was considered clinically meaningful.
Economic analysis: incremental net benefit
A within-trial cost-benefit analysis was conducted. The primary economic outcome, net benefits, was calculated as mean willingness to pay (WTP) - mean costs from the healthcare provider perspective. Costs were obtained through linkage of the trial dataset to NHS administrative data for primary dental care. WTP was obtained from a Discrete Choice Experiment (DCE) administered to a nationally representative online sample of the UK general population, and analysed using mixed logistical regression models. WTP tariffs from the DCE were mapped to interventions received, self-reported bleeding and aesthetics outcomes to calculate economic value (benefits). Multi-level hierarchical models accounted for clustering between costs and benefits, and adjusted for minimisation co-variates.
Results
Recruitment took place between February 2012 and May 2013 and follow-up closed on 2 September 2016. The flow of participants in the trial is shown in Figure 1. Across 63 dental practices, 2,341 patients were screened, 1,877 were recruited, 281 were eligible but declined, and 183 (8%) were ineligible. There were 112 dentists and 28 hygienists involved in delivering the interventions.
Participant practices' demographic characteristics per randomised group are shown in Table 1. Personalised OHA practices employed fewer hygienists than usual OHA practices (73% versus 80%) and most (78%) employed three or more dentists. Baseline demographic and clinical data for participant groups are shown in Table 2. There were no substantive differences for any socio-demographic factors or dental characteristics. The average age was 48 years; the majority (65%) were women. Around 60% reported receiving OHA and a S&P treatment at their last dental appointment.
Primary outcomes
Around 71% of participants attended their clinical follow-up. This percentage was similar across the randomised groups (436 out of 626 in the 6-monthly group; 447 out of 625 in the 12-monthly; 444 out of 623 in the no S&P; 615 out of 866 in the usual OHA group and 712 out of 1,008 in the personalised OHA group). Groups had similar levels of bleeding on probing at three years: no S&P 39.3 (SD 23.1), 12-monthly S&P 38.2 (SD 25.6), 6-monthly S&P 39.3 (SD 24.2). Table 3 summarises results for the primary outcomes. At 3 years there was no evidence of a difference in bleeding on probing between randomised groups, for example, 0 versus 6-monthly: mean difference 0.87%, 95% CI: -1.6 to 3.3, P = 0.48 or between patients randomised to receive usual or personalised OHA (mean difference -2.5%, 95%CI: -8.3 to 3.3, P = 0.39). The ICC at follow-up for bleeding was 0.23 (95% CI 0.16 to 0.31). The interaction between personalised OHA and 6-monthly S&P for bleeding was 1.7 (95% CI -3.8 to 7.3) (that is, neither statistically nor clinically significant). Approximately three quarters of participants completed a questionnaire at three years. Response rates were similar between the randomised groups (responders: 472 in the no S&P group; 486 in the 12-monthly yearly S&P; 494 in the 6-monthly S&P; 672 in the personalised group and 780 in the usual OHA group). Cognitive impact (self-efficacy) is presented by group and over time in Supplementary Figure 1. There was no evidence of a difference in cognitive impact (self-efficacy) between patients across groups: personalised versus usual mean difference: 0.02, 95% CI: -0.09 to 0.12; P = 0.75; 6 versus 0: difference -0.03, 95% CI: -0.12 to 0.06; P = 0.54; 12 versus 0: mean difference -0.1, 95% CI: -0.19 to -0.01; P = 0.04.
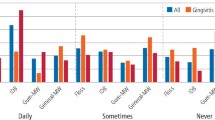
Subgroup analyses
Figures 2 and 3 display the means and 99% CIs for the differences in bleeding at three years by subgroups and randomised allocation. There was no evidence that any of the subgroups were significantly different at the 1% level.
Secondary outcomes
Table 3 shows that the mean level of calculus decreased across the no, 12-monthly and 6-monthly S&P groups. Calculus was significantly higher for the no versus 6-monthly groups (8.0%, 95% CI 5.4 to 10.7, P <0.001) with no evidence of a difference between 12-monthly and 6-monthly groups or personalised versus usual OHA. No evidence was found for clinically important differences in participant reported cognitive variables, however, attitude was significantly lower in the 6-monthly group compared with the no S&P group, favouring a better attitude to oral hygiene behaviour in the group going without (-0.137-95% CI -0.273 to -0.001; P = 0.048) (Supplementary Table 1).
At follow-up, dentists/hygienists believed in the usefulness of patient self-care for preventing disease, that providing OHA was an easy thing to do, and had a positive attitude towards providing OHA and S&P. Dentists/hygienists showed similar beliefs in both OHA randomised groups (data available upon request).
Fidelity of interventions
The routine data confirmed the expected differences between the frequency of S&P groups with mean numbers of S&Ps over the three years of: no S&P mean 1.0 (SD1.2), 12-monthly S&P mean 1.8 (SD1.1), 6-monthly mean 2.8 (SD 1.5). Compliance with providing initial personalised advice was 100% as witnessed by the trial team.
Economic outcomes
Over the three years, the group randomised to receive no S&P had the lowest average total NHS costs. The DCE demonstrated that the general population place a high value on, and are willing to pay for both interventions (more for S&P than personalised OHA.) They also value the perceived clinical benefits (bleeding) and aesthetic benefits. Given the lack of demonstrable clinical benefit, it is unlikely that S&P or personalised OHA offer value for money if the goal of NHS funding is to maximise dental health. However, when broadening the valuation space to consider all sources of value (both health and non-health), 6-monthly S&P with personalised OHA had the largest incremental net benefit compared to standard care (6-monthly S&P and usual OHA) (difference £48, 95% CI £22 to £74).
Discussion
IQuaD is the first large pragmatic multi-level cluster factorial randomised controlled trial (RCT) to evaluate the effectiveness and impact of S&P treatment and OHA provision22. At three years, there was no evidence of a meaningful benefit in terms of clinical effectiveness (38% of sites were bleeding whatever intervention was received at the end of the three-year trial period) or patient's confidence in self-care in scheduling 6-monthly or 12-monthly S&P treatment over not providing this treatment. There was also no evidence that there was any benefit in providing personalised OHA or usual OHA (current practice) by itself or in combination with any of the S&P schedules. The results of the economic analyses suggest that patients valued and were willing to pay for both interventions, with greater value placed on receiving the S&P treatment.
Limitations
Being a pragmatic trial, S&P treatments were provided if patient participants requested them, regardless of group. Although this meant some participants experienced more S&P treatments than the randomisation directed, there was still a clear separation in the mean number of S&Ps between groups, in the expected directions.
Another limitation concerned the personalised OHA intervention. This was designed as a brief (around five minutes) theoretically-informed intervention appropriate to be delivered in primary dental care by dentists/hygienists. Between the time of its development and implementation in the trial, clinical guidance documents were disseminated which recommended similar advice content23. This is likely to have increased the similarity of the personalised advice intervention with current (usual) practice, accounting for the lack of any additional benefit. Furthermore, there was also a likely ceiling effect in relation to the possible cognitive impact as most patients were confident in performing their self-care at baseline (means in all groups scoring over 5 out of 7; see Supplementary Figure 1).
Conclusion
This trial compares the clinical effectiveness of frequency of different S&P treatments (including none) and comes to the controversial conclusion that there is no additional clinical benefit to these treatments. The trial was unable to find a clinical benefit for a brief personalised OHA versus usual OHA. The evidence therefore suggests that if the aim is to maximise dental health, the current scheduling of S&P treatments is an inefficient use of scarce NHS resources. One alternative approach would be to re-direct funding towards patients with clear diagnoses of unstable levels of disease as defined in the revised 2017 periodontal diseases classification.21 However, the evidence also demonstrates that the general population value and are willing to pay for these services. Changing current practice will require the cooperation of healthcare policymakers, changing NHS contracts, clinician knowledge and decision making, as well as patient input. The results also have implications for other healthcare systems supporting a similar approach to preventing this disease. The presence of COVID-19 has led to restrictions and concerns on the use of aerosol generating procedures. It may be reassuring to patients that they are not missing out on a clinical benefit by forgoing S&P treatments during the global pandemic. An editorial in the Lancet states: 'This is also a time to stop delivering unnecessary and ineffective treatments. A perfect example of this is the routine provision of scaling and polishing, a procedure that does not have an evidence base and is a costly waste of resources.'24
This study focused on patients who are regularly attending adults with BPE scores 0-3. Seventy percent had gingivitis (BPE codes 1 and 2) and 30% had probing depths of 3.5-5.5 mm (BPE code 3); therefore, further research is needed to assess the effect and cost-effectiveness of interventions to improve self-care of all patients and to treat unstable periodontitis in primary care.
References
Ramsay C R, Clarkson J E, Duncan A et al. Improving the Quality of Dentistry (IQuaD): A cluster factorial randomised controlled trial comparing the effectiveness and cost-benefit of oral hygiene advice and/or periodontal instrumentation with routine care for the prevention and management of periodontal disease in dentate adults attending dental primary care. Health Technol Assess 2018; 22: 1-144.
Azarpazhooh A, Leake J L. Systematic review of the association between respiratory diseases and oral health. J Periodontol 2006; 77: 1465-1482.
Neely A L, Holford T R, Loe H, Anerud A, Boysen H. The natural history of periodontal disease in man. Risk factors for progression of attachment loss in individuals receiving no oral health care. J Periodontol 2001; 2: 1006-1015.
Papapanou PN. Epidemiology of periodontal diseases: an update. J Int Acad Periodontol 1999; 1: 110-116.
Petersen P E, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 2000; 60: 15-39.
Kassebaum N J, Bernabe E, Dahiya M, Bhandari B, Murray C J, Marcenes W. Global burden of severe periodontitis in 1990-2010: a systematic review and meta-regression. J Dent Res 2014; 93: 1045-1053.
Listl S, Galloway J, Mossey P A, Marcenes W. Global Economic Impact of Dental Diseases. J Dent Res 2015; 94: 1355-1361.
Steele J, O'Sullivan I. Executive Summary: Adult Dental Health Survey 2009. 2011. Available at http://content.digital.nhs.uk/catalogue/PUB01086/adul-dent-heal-surv-summ-them-exec-2009-rep2.pdf (accessed January 2021).
Chapple I L, Van der Weijden F, Doerfer C et al. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol 2015; 42(Suppl 16): S71-S76.
Axelsson P, Nystrom B, Lindhe J. The long-term effect of a plaque control programme on tooth mortality, caries and periodontal disease in adults: Results after 30 years of maintenance. J Clin Periodontol 2004; 31: 749-757.
National Health Service. NHS Dental Statistics for England 2015-16. Available at https://files.digital.nhs.uk/publicationimport/pub21xxx/pub21701/nhs-dent-stat-eng-15-16-rep-v2.pdf (accessed January 2021).
NHS Information Services Division Scotland. Primary Care Dentistry in Scotland: Dental Statistics - NHS Treatment & Fees. Statistics as at March 2019. 2019. Available at (accessed January 2021).
Worthington H V, Clarkson J E, Bryan G, Beirne P. Routine scale and polish for periodontal health in adults. Cochrane Database Syst Rev 2013; DOI:10.1002/14651858.CD004625.pub5.
Goulão B, MacLennan G, Ramsay C. The split-plot design was useful for evaluating complex, multilevel interventions, but there is need for improvement in its design and report. J Clin Epidemiol 2018; 96: 120-125.
Clarkson J E, Ramsay C R, Averley P et al. IQuaD dental trial; improving the quality of dentistry: a multicentre randomised controlled trial comparing oral hygiene advice and periodontal instrumentation for the prevention and management of periodontal disease in dentate adults attending dental primary care. BMC Oral Health 2013; 13: DOI: 10.1186/1472-6831-13-58.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health 1998; 13: 623-649.
Gollwitzer P M. Implementation intentions: Strong effects of simple plans. Am Psychol 1999; 54: 493-503.
Hefti A F, Preshaw P M. Examiner alignment and assessment in clinical periodontal research. Periodontol 2012; 59: 41-60.
Loe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol 1967; 38(6 Suppl): 610-616.
Slade G D. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997; 25: 284-290.
Caton J G, Armitage G, Berglundh T et al. A new classification scheme for the periodontal and peri-implant diseases and conditions - Introduction and key chages from the 1999 classification. J Clin Periodontol 2018; 45 (suppl 20): S1-S8.
Lamont T, Worthington H V, Clarkson J E, Beirne P V. Routine scale and polish for periodontal health in adults (Review). Cochrane Database Syst Rev 2018; DOI: 10.1002/14651858.CD004625.pub5.
Scottish Dental Clinical Effectiveness Programme (SDCEP). Prevention and Treatment of Periodontal Diseases in Primary Care: Dental Clinical Guidance. Dundee: SDCEP, 2014. Available at www.sdcep.org.uk/wp-content/uploads/2015/01/SDCEP+Periodontal+Disease+Full+Guidance.pdf (accessed February 2020).
Watt R G. COVID-19 is an opportunity for reform in dentistry. Lancet 2020; 396: 462.
Acknowledgements
We would like to acknowledge the participating dental practice teams and patients without whose valuable contribution this study could not have taken place. We would also like to acknowledge the role of the IQuaD Group members from the NIHR HTA IQuaD final report for their dedication and support. In addition, we would like to thank the IQuaD Perio-Advisory Committee members for their support throughout the trial; Mary Cullinan, Mark Ide, Ian Needleman, Tim Newton, Greg Seymour. Ethical approval: a favourable ethical opinion for the trial was provided by the East of Scotland Research Ethics 24 March 2011 (REC reference number 10/S0501/65).
Funding information
This project was funded by the NIHR HTA Programme (project number 09/01/45) and was published in full in Health Technology Assessment 2018: 22(38) Current Controlled Trials number ISRCTN56465715: https://doi.org/10.3310/hta22380. The results have been reproduced as per the non-commercial Government licence: http://www.nationalarchives.gov.uk/doc/non-commercial-government-licence/version/2/. Further information available at: https://www.journalslibrary.nihr.ac.uk/HTA. The Health Services Research Unit and the Health Economics Research Unit are funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates. This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, CCF, NETSCC, the NIHR HTA programme or the Department of Health.
Author information
Authors and Affiliations
Contributions
JC, CR, HW, PH, M van der Pol, LY, GM contributed to conception and design. JC, CR, HW, PH, M van der Pol, LY, GM, TL, DB, AD, BG contributed to data acquisition, analysis and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
None to disclose.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Clarkson, J., Ramsay, C., Lamont, T. et al. Examining the impact of oral hygiene advice and/or scale and polish on periodontal disease: the IQuaD cluster factorial randomised controlled trial. Br Dent J 230, 229–235 (2021). https://doi.org/10.1038/s41415-021-2662-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-021-2662-3