Abstract
Minimally invasive (MI) concepts in restorative dentistry in the year 2020 request from the practitioner not only a scientifically supported rationale for carious tissue removal/excavation and defect-oriented, biological cavity preparation, but also a deep understanding of how to ensure a biomechanically stable and durable restoration in different clinical situations by applying different restorative options. Bio-interactive materials play an increasingly relevant role, as they not only replace diseased or lost tissue, but also optimise tissue mineral recovery (among other properties) when used in restorative and preventive dentistry. Indeed, this is of certain interest in MI restorative dentistry, especially in those cases where gap formation jeopardises the integrity of the margins along resin composite restorations, causing penetration of bacteria and eventually promoting the formation of secondary caries. Recently, the interest in whether ion-releasing materials may reduce such biofilm penetration into margin gaps and reduce such a risk for development and propagation of secondary caries is growing significantly among clinicians and scientists. The aim of this article was to explore mechanisms involved in the process that allow mineral deposition at the interface between such materials and dentine, and to describe how conventional 'bioactive' restorative materials currently available on the market may benefit treatments in MI dentistry.
Key points
-
Explores the mechanisms involved in the process that allows mineral deposition at the interface between such materials and dentine, and describes how conventional 'bioactive' restorative materials currently available on the market may be beneficial for treatments in minimally invasive (MI) dentistry.
-
Different carious tissue removal methods are currently available. However, chemo-mechanical methods reach a compromise between MI tissue removal to protect the pulp and an 'adhesion-friendly' substrate to enable successful restoration placement and interfacial longevity.
-
Contemporary 'therapeutic' bio-interactive materials should now be used for tissue replacement, as they may be able to reduce the susceptibility of tooth mineral to dissolution and/or to recover its mechanical properties via remineralisation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
He L H, Yin ZH, van Vuuren L J, Carter E A, Liang X W. A natural functionally graded biocomposite coating: Human enamel. Acta Biomater 2013; 9: 6330-6337.
Bertassoni L E. Dentin on the nanoscale: Hierarchical organisation, mechanical behaviour and bioinspired engineering. Dent Mater 2017; 33: 637-649.
Giacaman R, Perez V A, Carrera A. Mineralisation processes in hard tissues: Teeth. In Aparicio C, Ginebra M P (eds) Biomineralisation and biomaterials: Fundamentals and applications. pp 147-185. Waltham: Woodhead Publishing, 2016.
Neves A A, Coutinho E, Alves H D, Assis J T. Stress and strain distribution in demineralized enamel: A micro-CT based finite element study. Microsc Res Tech 2015; 78: 865-872.
Larsen M J, Pearce E I. Saturation of human saliva with respect to calcium salts. Arch Oral Biol 2003; 48: 317-322.
Niu L N, Zhang W, Pashley D H et al. Biomimetic remineralization of dentin. Dent Mater 2014; 30: 77-96.
Kidd E A, Fejerskov O. What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. J Dent Res 2004; DOI: 10.1177/154405910408301s07.
Fernandez-Ferrer L, Vicente-Ruiz M, Garcia-Sanz V et al. Enamel remineralization therapies for treating postorthodontic white-spot lesions: A systematic review. J Am Dent Assoc 2018; 149: 778-786.
Goldberg M, Kulkarni A B, Young M, Boskey A. Dentin: Structure, composition and mineralization. Front Biosci (Elite Ed) 2011; 3: 711-735.
Bertassoni L E, Habelitz S, Kinney J H, Marshall S J, Marshall-Jr G W. Biomechanical perspective on the remineralization of dentin. Caries Res 2009; 43: 70-77.
Sauro S, Osorio R, Watson T F, Toledano M. Influence of phosphoproteins' biomimetic analogues on remineralization of mineral-depleted resin-dentin interfaces created with ion-releasing resin-based systems. Dent Mater 2015; 31: 759-777.
Hunter G K, Poitras M S, Underhill T M, Grynpas M D, Goldberg H A. Induction of collagen mineralization by a bone sialoprotein-decorin chimeric protein. J Biomed Mater Res 2001; 55: 496-502.
Saito T, Arsenault A L, Yamauchi M, Kuboki Y, Crenshaw M A. Mineral induction by immobilized phosphoproteins. Bone 1997; 21: 305-311.
Gower L B. Biomimetic mineralization of collagen. In Aparicio C, Ginebra M P (eds) Biomineralisation and biomaterials: Fundamentals and applications. pp 187-232. Waltham: Woodhead Publishing, 2016.
Banerjee A. Minimal intervention dentistry: Part 7. Minimally invasive operative caries management: Rationale and techniques. Br Dent J 2013; 214: 107-111.
Schwendicke F, Frencken J E, Bjorndal L et al. Managing carious lesions: Consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58-67.
FDI World Dental Federation. FDI policy statement on minimal intervention dentistry (MID) for managing dental caries: Adopted by the general assembly: September 2016, Poznan, Poland. Int Dent J 2017; 67: 6-7.
Schwendicke F, Frencken J, Innes N. Clinical recommendations on carious tissue removal in cavitated lesions. Monogr Oral Sci 2018; 27: 162-166.
Sauro S, Pashley D H. Strategies to stabilise dentine-bonded interfaces through remineralising operative approaches: State of the art. Int J Adhes Adhes 2016; 69: 39-57.
Neves A, Coutinho E, Cardoso M, de Munck J, Van Meerbeek B. Micro-tensile bond strength and interfacial characterization of an adhesive bonded to dentin prepared by contemporary caries-excavation techniques. Dent Mater 2011; 27: 552-562.
Neves A A, Coutinho E, Cardoso M V, Lambrechts P, Van Meerbeek B. Current concepts and techniques for caries excavation and adhesion to residual dentin. J Adhes Dent 2011; 13: 7-22.
Banerjee A, Kidd E A M, Watson T F. Scanning electron microscopic observations of human dentine after mechanical caries excavation. J Dent 2000; 28: 179-186.
Neves A A, Coutinho E, De Munck J, Van Meerbeek B. Caries-removal effectiveness and minimal-invasiveness potential of caries-excavation techniques: A micro-CT investigation. J Dent 2011; 39: 154-162.
Banerjee A, Kidd E A M, Watson T F. In vitro evaluation of five alternative methods of carious dentine excavation. Caries Res 2000; 34: 144-510.
Neves A A, Coutinho E, Cardoso M V, de Munck J, Van Meerbeek B. Micro-tensile bond strength and interfacial characterization of an adhesive bonded to dentin prepared by contemporary caries-excavation techniques. Dent Mater 2011; 27: 552-562.
Schwendicke F, Al-Abdi A, Pascual Moscardo A, Ferrando Cascales A, Sauro S. Remineralization effects of conventional and experimental ion-releasing materials in chemically or bacterially-induced dentin caries lesions. Dent Mater 2019; 35: 772-779.
Liu Y, Mai S, Li N et al. Differences between top-down and bottom-up approaches in mineralizing thick, partially demineralized collagen scaffolds. Acta Biomater 2011; 7: 1742-1751.
Profeta A C, Mannocci F, Foxton R et al. Experimental etchandrinse adhesives doped with bioactive calcium silicate-based micro-fillers to generate therapeutic resin-dentin interfaces. Dent Mater 2013; 29: 729-741.
Tjaderhane L, Nascimento F D, Breschi L et al. Strategies to prevent hydrolytic degradation of the hybrid layer: A review. Dent Mater 2013; 29: 999-1011.
Erhardt M C G, Toledano M, Osorio R, Pimenta L A. Histomorphologic characterization and bond strength evaluation of caries-affected dentin/resin interfaces: Effects of long-term water exposure. Dent Mater 2008; 24: 786-798.
Wang Y, Spencer P, Walker M P. Chemical profile of adhesive/caries-affected dentin interfaces using raman microspectroscopy. J Biomed Mater Res A 2007; 81: 279-286.
Liu Y, Kim Y K, Dai L et al. Hierarchical and non-hierarchical mineralisation of collagen. Biomaterials 2011; 32: 1291-1300.
Tjaderhane L, Nascimento F D, Breschi L et al. Optimizing dentin bond durability: control of collagen degradation by matrix metalloproteinases and cysteine cathepsins. Dent Mater 2013; 29: 116-135.
Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res 2003; 92: 827-839.
Tezvergil-Mutluay A, Agee K A, Hoshika T et al. The requirement of zinc and calcium ions for functional MMP activity in demineralized dentin matrices. Dent Mater 2010; 26: 1059-1067.
Boelen G J, Boute L, d'Hoop J, EzEldeen M, Lambrichts I, Opdenakker G. Matrix metalloproteinases and inhibitors in dentistry. Clin Oral Investig 2019; 23:2823-2835.
Osorio R, Yamauti M, Sauro S, Watson T F, Toledano M. Experimental resin cements containing bioactive fillers reduce matrix metalloproteinase-mediated dentin collagen degradation. J Endod 2012; 38: 1227-1232.
Page-McCaw A, Ewald A J, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nat Rev Mol Cell Biol 2007; 8: 221-233.
Fu H, Rahaman M N, Day D E, Huang W. Effect of pyrophosphate ions on the conversion of calciumlithiumborate glass to hydroxyapatite in aqueous phosphate Solution. J Mater Sci Mater Med 2010; 21: 2733-2741.
Osorio R, Toledano M. Biomaterials for catalysed mineralization of dental hard tissues. In Aparicio C, Ginebra M P (eds) Biomineralisation and biomaterials: Fundamentals and applications. pp 365-376. Waltham: Woodhead Publishing, 2016.
Jones J R. Reprint of: Review of bioactive glass: From Hench to hybrids. Acta Biomater 2015; DOI: 10.1016/j.actbio.2015.07.019.
Anusavice K J, Shen C, Rawls H R. Dental cements. In Anusavice K J, Shen C, Rawls H R (eds) Phillips' science of dental materials. pp 418-473. Philadelphia: Saunders, 2012.
Hoppe A, Guldal N S, Boccaccini A R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials 2011; 32: 2757-2774.
Ma J, Wang J, Ai X, Zhang S. Biomimetic self-assembly of apatite hybrid materials: From a single molecular template to bi-/multi-molecular templates. Biotechnol Adv 2014; 32: 744-760.
Osorio R, Osorio E, Cabello I, Toledano M. Zinc induces apatite and scholzite formation during dentin remineralization. Caries Res 2014; 48: 276-290.
Qi Y P, Li N, Niu L N et al. Remineralization of artificial dentinal caries lesions by biomimetically modified mineral trioxide aggregate. Acta Biomater 2012; 8: 836-842.
Pires P M, Santos T P, Fonseca-Goncalves A, Pithon M M, Lopes R T, Neves A A. Mineral density in carious dentine after treatment with calcium silicates and polyacrylic acid based cements. Int Endod J 2018; 51: 1292-1300.
Falsafi A, Mitra S B, Oxman J D, Ton T T, Bui H T. Mechanisms of setting reactions and interfacial behaviour of a nano-filled resin-modified glass ionomer. Dent Mater 2014; 30: 632-643.
Koenraads H, Van der Kroon G, Frencken J E. Compressive strength of two newly developed glass-ionomer materials for use with the atraumatic restorative treatment (art) approach in class ii cavities. Dent Mater 2009; 25: 551-556.
Zainuddin N, Karpukhina N, Law R V, Hill R G. Characterisation of a remineralising glass carbomer ionomer cement by MAS-NMR spectroscopy. Dent Mater 2012; 28: 1051-1058.
Olegario I C, Hesse D, Mendes F M, Bonifacio C C, Raggio D P. Glass carbomer and compomer for art restorations: 3year results of a randomized clinical trial. Clin Oral Investig 2019; 23: 1761-1770.
Attin T, Vataschki M, Hellwig E. Properties of resin-modified glass-ionomer restorative materials and two polyacid-modified resin composite materials. Quintessence Int 1996; 27: 203-209.
Sidhu S K, Watson T F. Interfacial characteristics of resin-modified glass-ionomer materials: A study on fluid permeability using confocal fluorescence microscopy. J Dent Res 1998; 77: 1749-1759.
Nikolaenko S A, Lohbauer U, Roggendorf M, Petschelt A, Dasch W, Frankenberger R. Influence of cfactor and layering technique on microtensile bond strength to dentin. Dent Mater 2004; 20: 579-585.
Irie M, Suzuki K, Watts D C. Marginal gap formation of light-activated restorative materials: Effects of immediate setting shrinkage and bond strength. Dent Mater 2002; 18: 203-210.
Irie M, Suzuki K, Watts D C. Immediate performance of self-etching versus system adhesives with multiple light-activated restoratives. Dent Mater 2004; 20: 873-880.
Sampaio PC, de Almeida Junior A A, Francisconi L F et al. Effect of conventional and resin-modified glass-ionomer liner on dentin adhesive interface of class i cavity walls after thermocycling. Oper Dent 2011; 36: 403-412.
Sauro S, Faus-Matoses V, Makeeva I et al. Effects of polyacrylic acid pre-treatment on bonded-dentine interfaces created with a modern bioactive resin-modified glass ionomer cement and subjected to cycling mechanical stress. Materials (Basel) 2018; 11: 1884.
Toledano M, Cabello I, Aguilera F S, Osorio E, Osorio R. Effect of in vitro chewing and bruxism events on remineralization, at the resin-dentin interface. J Biomech 2015; 48: 14-21.
Khvostenko D, Salehi S, Naleway S E et al. Cyclic mechanical loading promotes bacterial penetration along composite restoration marginal gaps. Dent Mater 2015; 31: 702-710.
Ikemura K, Tay F R, Endo T, Pashley D H. A review of chemical-approach and ultramorphological studies on the development of fluoride-releasing dental adhesives comprising new pre-reacted glass ionomer (PRG) fillers. Dent Mater J 2008; 27: 315-339.
Gordan V V, Mondragon E, Watson R E, Garvan C, Mjor I A. A clinical evaluation of a self-etching primer and a giomer restorative material: Results at eight years. J Am Dent Assoc 2007; 138: 621-627.
Sauro S, Makeeva I, Faus-Matoses V et al. Effects of ions-releasing restorative materials on the dentine bonding longevity of modern universal adhesives after load-cycle and prolonged artificial saliva aging. Materials (Basel) 2019; 12: 722.
Hench L L. Biological applications of bioactive glasses. Life Chem Rep 1996; 13: 187-241.
Yli-Urpo H, Narhi M, Narhi T. Compound changes and tooth mineralization effects of glass ionomer cements containing bioactive glass (s53p4): An in vivo study. Biomaterials 2005; 26: 5934-5941.
Salonen J I, Arjasamaa M, Tuominen U, Behbehani M J, Zaatar E I. Bioactive glass in dentistry. J Min Inv Dent 2009; 2: 208-218.
Hench L L. Bioceramics. J Amer Ceram Soc 1998; 74: 1487-1510.
Prabhakar A R, Paul M J, Basappa N. Comparative evaluation of the remineralizing effects and surface micro hardness of glass ionomer cements containing bioactive glass (s53p4): An in vitro study. Int J Clin Paediatr Dent 2010; 3: 69-77.
Sauro S, Watson T F, Thompson I. Dentine desensitization induced by prophylactic and air-polishing procedures: An in vitro dentine permeability and confocal microscopy study. J Dent 2010; 38: 411-422.
Makowski G S, Ramsby M L. Differential effect of calcium phosphate and calcium pyrophosphate on binding of matrix metalloproteinases to fibrin: Comparison to a fibrin-binding protease from inflammatory joint fluids. Clin Exp Immunol 2004; 136: 176-187.
Hench L L, Jones J R. Bioactive glasses: Frontiers and challenges. Front Bioeng Biotechnol 2015; 3: 194.
Kremer E A, Chen Y, Suzuki K, Nagase H, Gorski J P. Hydroxyapatite induces autolytic degradation and inactivation of matrix metalloproteinase-1 and3. J Bone Miner Res 1998; 13: 1890-1902.
Tavafoghi M, Cerruti M. The role of amino acids in hydroxyapatite mineralization. J Royal Soc Interface 2016; 13: 20160462.
Torabinejad M, Hong C U, McDonald F, Pitt Ford T R. Physical and chemical properties of a new root-end filling material. J Endod 1995; 21: 349-353.
Atmeh A R, Chong E Z, Richard G, Festy F, Watson T F. Dentin-cement interfacial interaction: Calcium silicates and polyalkenoates. J Dent Res 2012; 91: 454-459.
Camilleri J, Montesin F E, Papaioannou S, McDonald F, Pitt Ford T R. Biocompatibility of two commercial forms of mineral trioxide aggregate. Int Endod J 2004; 37: 699-704.
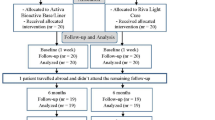
Ali A H, Koller G, Foschi F et al. Self-limiting versus conventional caries removal: A randomized clinical trial. J Dent Res 2018; 97: 1207-1213.
Tawil P Z, Duggan D J, Galicia J C. Mineral trioxide aggregate (MTA): Its history, composition, and clinical applications. Compend Contin Educ Dent 2015; 36: 247-252; quiz 254, 264.
Fransson H. On the repair of the dentine barrier. Swed Dent J 2012; 226: 9-84.
Kim S G, Malek M, Sigurdsson A, Lin L M, Kahler B. Regenerative endodontics: A comprehensive review. Int Endod J 2018; 51: 1367-1388.
Sanz J L, Rodriguez-Lozano F J, Llena C, Sauro S, Forner L. Bioactivity of bioceramic materials used in the dentin-pulp complex therapy: A systematic review. Materials (Basel) 2019; 12: 1015.
Yamaga R, Yokomizo I. Arrestment of caries of deciduous teeth with diamine silver fluoride. Dent Outlook 1969; 33: 1007-1013.
Horst J A, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc 2016; 44: 16-28.
Gao S S, Zhao I S, Hiraishi N et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res 2016; 1: 201-210.
Chen Y, Miao X. Thermal and chemical stability of fluorohydroxyapatite ceramics with different fluorine contents. Biomaterials 2005; 26: 1205-1210.
Mei M L, Nudelman F, Marzec B et al. Formation of fluorohydroxyapatite with silver diamine fluoride. J Dent Res 2017; 96: 1122-1128.
Mei M L, Ito L, Cao Y, Li Q L, Lo E C, Chu C H. Inhibitory effect of silver diamine fluoride on dentine demineralisation and collagen degradation. J Dent 2013; 41: 809-817.
Mei M L, Lo E C M, Chu C H. Arresting dentine caries with silver diamine fluoride: what's behind it? J Dent Res 2018; 97: 751-758.
Mei M L, Li Q L, Chu C H, Lo E C M, Samaranayake L P. Antibacterial effects of silver diamine fluoride on multi-species cariogenic biofilm on caries. Ann Clin Microbiol Antimicrob 2013; 12: 4.
Zhao I S, Chu S, Yu O Y, Mei M L, Chu C H, Lo E C M. Effect of silver diamine fluoride and potassium iodide on shear bond strength of glass ionomer cements to caries-affected dentine. Int Dent J 2019; 69: 341-347.
Watson T F, Atmeh A R, Sajini S, Cook R J, Festy F. Present and future of glass-ionomers and calcium-silicate cements as bioactive materials in dentistry: Biophotonics-based interfacial analyses in health and disease. Dent Mater 2014; 30: 50-61.
Wang Z, Shen Y, Haapasalo M et al. Polycarboxylated microfillers incorporated into light-curable resin-based dental adhesives evoke remineralization at the mineral-depleted dentin. J Biomater Sci Polym Ed 2014; 25: 679-697.
Acknowledgements
Dr Paula Maciel Pires was undertaking a PhD exchange programme at Cardenal Herrera University during the writing up of this manuscript and that was supported by a CAPES grant from Brazil (grant numbers 88882.424807/2018-01 and 88881.188518/2018-01). Unpublished data presented in this manuscript is part of a FAPERJ project granted to Dr Aline de Almeida Neves (E-26/203.185/2016) and micro-CT images of SDF-treated teeth were kindly provided by Dr Andréa Fonseca-Gonçalves and Gabriella Fernandes Rodrigues from the Federal University of Rio de Janeiro. Part of this work was also supported by 'Programa de Consolidación de Indicadores: Fomento Plan Estatal CEU-UCH 2018-2020' granted to Dr Salvatore Sauro.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pires, P., Neves, A., Makeeva, I. et al. Contemporary restorative ion-releasing materials: current status, interfacial properties and operative approaches. Br Dent J 229, 450–458 (2020). https://doi.org/10.1038/s41415-020-2169-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-2169-3
This article is cited by
-
Bonding performance and interfacial adaptation of modern bulk-fill restorative composites after aging in artificial saliva: an in vitro study
Clinical Oral Investigations (2024)
-
Secondary caries and marginal adaptation of ion-releasing versus resin composite restorations: a systematic review and meta-analysis of randomized clinical trials
Scientific Reports (2022)
-
Dental adhesion with resin composites: a review and clinical tips for best practice
British Dental Journal (2022)
-
Assessment of the remineralisation induced by contemporary ion-releasing materials in mineral-depleted dentine
Clinical Oral Investigations (2022)