Abstract
Aims The first aim was to describe the energy, carbohydrate and sugar contents of formula milk products in eleven countries. The second was to assess the labelling methods used. Based on the findings, approaches to facilitate the selection of infant-appropriate formula milk products were proposed.
Background Consumption of excess sugar during infancy can increase the risk of non-communicable diseases (NCDs) including obesity, diabetes and dental caries. Reduction of sugar consumption has been high on the global public health agenda. Although most infants are fed formula milk products in addition to, or instead of, breastmilk (with only 38% exclusively breastfed), the sugar content of these products is often not included in sugar reduction strategies.
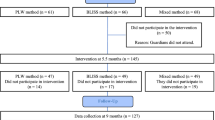
Methods An exploratory study was conducted to describe the labelling and nutritional composition of a sample of infant formula products available in 11 countries. The sample, which was collected between May and August 2019, included commercially available formula products (n = 257) targeted at infants aged <3 years of age. The products were sold in supermarkets and by other major retailers across the sample countries. Primary data were obtained from labels on the packaging of the formula products.
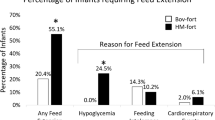
Results Findings suggest that the majority of products sampled were higher in total carbohydrate and carbohydrates of which sugar and lactose, than breastmilk, supporting previous research. The nutrition information presented on the products was often unclear and was inconsistent across the 11 counties sampled. None of the products had front-of-pack (FOP) nutritional information.
Conclusion Findings suggest that globally, infant formula products are higher in carbohydrates, sugar and lactose than breastmilk. Labelling is unclear and inconsistent across brands and between countries. Based on the findings of this study, mandatory regulation of sugar content in formula products is needed with clear FOP nutrition information to help consumers choose the healthy option for their infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
The World Bank. Repositioning nutrition as central to development: a strategy for large-scale action - overview. The World Bank. pp. 1-30. Report No.: 57489. Available online at http://documents.worldbank.org/curated/en/185651468175733998/Repositioning-nutrition-as-central-to-development-a-strategy-for-large-scale-action-overview (accessed 19 August 2019).
Akkerman R, Faas MM, de Vos P. Non-digestible carbohydrates in infant formula as substitution for human milk oligosaccharide functions: Effects on microbiota and gut maturation. Crit Rev Food Sci Nutr 2019; 59: 1486-1497.
Martin C R, Ling PR, Blackburn G L. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016; 8: 279. Available online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4882692/ (accessed 19 August 2019).
WHO. Infant and young child nutrition: Global strategy on infant and young child feeding [Internet]. World Health Organisation; 2002. Report No.: A55/15. Available online at http://apps.who.int/gb/archive/pdf_files/WHA55/ea5515.pdf (accessed 19 August 2019).
Scientific Advisory Committee on Nutrition (SACN). SACN's 'Feeding in the First Year of Life' report published - British Nutrition Foundation [Internet]. ition Foundation. 2018. Available online at https://www.nutrition.org.uk/nutritioninthenews/new-reports/feedinginthefirstyear.html (accessed 19 August 2019).
Kozhimannil K B, Jou J, Attanasio L B, Joarnt L K, McGovern P. Medically complex pregnancies and early breastfeeding behaviors: a retrospective analysis. PloS One 2014; 9: e104820.
Ogbuanu C A, Probst J, Laditka S B, Liu J, Baek J, Glover S. Reasons why women do not initiate breastfeeding. Womens Health Issues 2009; 19: 268-278.
Kakute P N, Ngum J, Mitchell P et al. Cultural Barriers to Exclusive Breastfeeding by Mothers in a Rural Area of Cameroon, Africa. J Midwifery Womens Health 2005; 50: 324-328.
Meyer R, Baker G, Reeves L. Children with cows milk allergy. BDA The Association of UK Dietitians. 2017. Available online at https://www.bda.uk.com/foodfacts/children_with_cows_milk_allergy (accessed 19 August 2019).
NHS Royal Berkshire. Could you become a breastmilk donor? NHS. 2018. Available online at https://www.royalberkshire.nhs.uk/patient-information-leaflets/maternity---could-you-become-a-breast-milk-donor.htm (access 21 August 2019).
Alencar L, Seidl E. Breast milk donation: women's donor experience. Rev Saude Publica 2009; 43: 70-77.
Stanislawski M A, Dabelea D, Wagner B D et al. Gut Microbiota in the First 2 Years of Life and the Association with Body Mass Index at Age 12 in a Norwegian Birth Cohort. mBio 2018; 9: e01751-18.
Makrides M, Neumann M A, Gibson R A. Effect of maternal docosahexaenoic acid (DHA) supplementation on breast milk composition. Eur J Clin Nutr 1996; 50: 352-357.
Dewey K G, Heinig M J, Nommsen L A, Lonnerdal B. Maternal versus infant factors related to breast milk intake and residual milk volume: The DARLING study. Pediatrics 1991; 87: 829-837.
Mitoulas L R, Kent J C, Cox D B, Owens R A, Sherriff J L, Hartmann P E. Variation in fat, lactose and protein in human milk over 24 h and throughout the first year of lactation. Br J Nutr 2002; 88: 29-37.
Jackson J G, Janszen D B, Lonnerdal B, Lien E L, Pramuk K P, Kuhlman C F. A multinational study of alpha-lactalbumin concentrations in human milk. J Nutr Biochem 2004; 15: 517-521.
Zhang Z, Adelman A S, Rai D, Boettcher J, Lőnnerdal B. Amino acid profiles in term and preterm human milk through lactation: a systematic review. Nutrients 2013; 5: 4800-4821.
Jenness R. The composition of human milk. Semin Perinatol 1979; 3: 225-239.
Stephen A, Alles M, de Graaf C et al. The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur J Clin Nutr 2012; 66: 765-779.
Walker R, Goran M. Laboratory Determined sugar content and composition of commercial infant formulas, baby foods and common grocery items targeted to children. Nutrients 2015; 7: 5850-5867.
Young B. Best Baby Formula - Carbs & Sugars. Baby Formula Expert. 2018. Available online at https://babyformulaexpert.com/babyformulacarbs/ (accessed 20 August 2019).
Skinner J D, Carruth B R, Wendy B, Ziegler P J. Children's food preferences: a longitudinal analysis. J Am Diet Assoc 2002; 102: 1638-1647.
Beauchamp G K, Mennella J A. Early flavor learning and its impact on later feeding behavior. J Pediatr Gastroenterol Nutr 2009; 48 Suppl 1: S25-30.
Park S, Pan L, Sherry B, Li R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014; 134 Suppl 1: S56-62.
Nader P R, O'Brien M, Houts R et al. Identifying risk for obesity in early childhood. Pediatrics. 2006; 118: e594-601.
Koletzko B, Brands B, Poston L, Godfrey K, Demmelmair H. Early Nutrition Project. Early nutrition programming of long-term health. Proc Nutr Soc 2012; 71: 371-378.
Tungare S, Paranjpe A G. Baby bottle syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2019; Available online at http //www.ncbi.nlm.nih.gov/books/NBK535349/ (accessed 20 August 2019).
Mandavilli A. Breast milk is teeming with bacteria — that's good for the baby. The New York Times. 2019 Available online at https://www.nytimes.com/2019/06/12/health/breastmilk-microbiome-parenting.html (accessed 20 August 2019).
Bode L. Human milk oligosaccharides: Every baby needs a sugar mama. Glycobiology 2012; 22: 1147-1162.
Doherty A M, Lodge C J, Dharmage S C, Dai X, Bode L, Lowe A J. Human milk oligosaccharides and associations with immune-mediated disease and infection in childhood: a systematic review. Front Pediatr 2018; 6: 91. Available online at https://www.frontiersin.org/articles/10.3389/fped.2018.00091/full (accessed 21 September 2019).
Duijts L, Ramadhani M K, Moll H A. Breastfeeding protects against infectious diseases during infancy in industrialized countries. A systematic review. Matern Child Nutr 2009; 5: 199-210.
Hoppu U, Kalliomäki M, Laiho K, Isolauri E. Breast milk - immunomodulatory signals against allergic diseases. Allergy 2001; 56: 23-26.
Erney R M, Malone W T, Skelding M B et al. Variability of human milk neutral oligosaccharides in a diverse population. J Pediatr Gastroenterol Nutr 2000; 30: 181.
UNICEF. The International Code of Marketing of Breastmilk Substitutes. Baby Friendly Initiative. 2018. Available online at https://www.unicef.org.uk/babyfriendly/baby-friendly-resources/international-code-marketing-breastmilk-substitutes-resources/the-code/ (accessed August 2019).
Government of Canada C F I A. Labelling Requirements for Infant Foods, Infant Formula and Human Milk. Candian Food Inspection agency. 2014. Available from: http://www.inspection.gc.ca/food/requirements-and-guidance/labelling/industry/infant-foods-infant-formula-and-human-milk/eng/1393069958870/1393070130128?chap=3 (accessed August 2019).
UN. Baby foods high in sugar, inappropriately marketed in Europe, reveal two UN studies. United Nations. 2019. Available online at https://news.un.org/en/story/2019/07/1042441 (accessed August 2019).
Legislation.gov.uk. The Infant Formula and Follow-on Formula (England) Regulations 2007. 2007. Available online at http://www.legislation.gov.uk/uksi/2007/3521/contents/made (accessed August 2019).
Baby Milk Action. Evidence that harmful baby food marketing continues. Baby milk action IBAFN UK. 2018. Available online at http://www.babymilkaction.org/monitoring-global (accessed August 2020).
Baby Milk Action. Look What They're Doing in the UK. Baby milk action IBAFN UK. 2017. Available online at http://www.babymilkaction.org/monitoringuk17 (accessed August 2019).
van Tulleken C. Overdiagnosis and industry influence: how cow's milk protein allergy is extending the reach of infant formula manufacturers. BMJ 2018; 363: k5056.
Gribble K, Berry N J. Infant formula companies are behind the guidelines on milk allergy, and their sales are soaring. The Conversation. 2018. Available online at http://theconversation.com/infant-formula-companies-are-behind-the-guidelines-on-milk-allergy-and-their-sales-are-soaring-108255 (accessed August 2019).
Fabbri A, Lai A, Grundy Q, Bero L. The Influence of Industry Sponsorship on the Research Agenda: A Scoping Review. Am J Public Health 2018; 108: DOI: 10.2105/AJPH.2018.304677.
Timsit A. Why a UK pediatricians' group cut funding ties with baby formula. Quartz. 2019. Available online at https://qz.com/1550656/why-the-uks-largest-body-of-pediatricians-will-no-longer-take-money-from-baby-formula-companies/ (accessed August 2019).
Save the Children. Don't push it: Why the formula milk industry must clean up its act. 2018. Available online at https://www.savethechildren.org.uk/content/dam/gb/reports/health/dont-push-it.pdf (accessed August 2019).
Harney A. Special Report: How Big Formula bought China - Reuters. 2013. Available online at https://www.reuters.com/article/us-china-milkpowder-specialreport/special-report-how-big-formula-bought-china-idUSBRE9A700820131108 (accessed August 2019).
WHO. Reducing consumption of sugar-sweetened beverages to reduce the risk of unhealthy weight gain in adults. 2014. Available online at https://www.who.int/elena/bbc/ssbs_adult_weight/en/ (accessed August 2019).
Sowa P M, Keller E, Stormon N, Lalloo R, Ford P J. The impact of a sugar-sweetened beverages tax on oral health and costs of dental care in Australia. Eur J Public Health 2019; 29: 173-177.
Billich N, Blake M R, Backholer K, Cobcroft M, Li V, Peeters A. The effect of sugar-sweetened beverage frontofpack labels on drink selection, health knowledge and awareness: An online randomised controlled trial. Appetite 2018; 128: 233-241.
Raine K D, Lobstein T, Landon J et al. Restricting marketing to children: consensus on policy interventions to address obesity. J Public Health Policy 2013; 34: 239-253.
European Communities. COMMISSION DIRECTIVE 2006/141/EC of 22 December 2006 on infant formulae and follow-on formulae and amending Directive 1999/21/EC. 2006. Available online at https://www.fsai.ie/uploadedFiles/Consol_Dir2006_141.pdf (accessed August 2019).
First Steps Nutrition trust. How does legislation on infant formula composition and labelling differ in the UK and US? 2018. Available online at https://static1.squarespace.com/static/59f75004f09ca48694070f3b/t/5b44e2f4758d46a2604442f5/1531241207016/Statement_on_UK_and_US_infant_formula_regulations_Jan18.pdf (accessed August 2019).
Sweet L, Pereira C, Ford R et al. Assessment of corporate compliance with guidance and regulations on labels of commercially produced complementary foods sold in Cambodia, Nepal, Senegal and Tanzania. Matern Child Nutr 2016; 12(Suppl 2): 106-125.
Associated Press. Companies pushed baby formula in Peru despite ban. Federal News Network. 2019. Available online at https://federalnewsnetwork.com/business-news/2019/06/companies-pushed-baby-formula-in-peru-despite-ban/ (accessed August 2019).
Rothstein J, Caulfield L, Broaddus-Shea E, Muschelli J, Gilman R, Winch P. "The doctor said formula would help me": Health sector influences on use of infant formula in peri-urban Lima, Peru. Soc Sci Med 2019; DOI: 10.1016/j.socscimed.2019.05.029.
Aspril J, Health JBS of P. In Peru, Baby Formula Reps Target Doctors In Low-Income Community Despite Decades-Old Ban. Johns Hopkins Bloomberg School of Public Health. 2019. Available online at https://www.jhsph.edu/news/news-releases/2019/in-peru-baby-formula-reps-target-doctors-in-low-income-community-despite-decades-old-ban.html (accessed August 2019).
Boyd C. The Nestlé infant formula controversy and a strange web of subsequent business scandals. J Bus Ethics 2012; 106: 283-293.
Koe T. Low rate of breastfeeding in China attributed to heavy marketing of infant formula. Nutra Ingredients-asia.com. 2019. Available online at https://www.nutraingredients-asia.com/Article/2019/03/19/Low-rate-of-breastfeeding-in-China-attributed-to-heavy-marketing-of-infant-formula (accessed August 2019).
Neslen A. Nestlé under fire for marketing claims on baby milk formulas. The Guardian 2018. Available online at https://www.theguardian.com/business/2018/feb/01/nestle-under-fire-for-marketing-claims-on-baby-milk-formulas (accessed August 2019).
Bagriansky J, Champa N, Pak K, Whitney S, Laillou A. The economic consequences of malnutrition in Cambodia, more than 400 million US dollar lost annually. Asia Pac J Clin Nutr 2014; 23: 524.
UNICEF. Reducing Stunting in Children Under Five Years of Age: A Comprehensive Evaluation of UNICEF'S Strategies and Programme Performance - Cambodia Country Case Study. UNICEF 2017 (EVALUATION AND LEARNING BRIEF). Report No. 6. Available online at https://www.unicef.org/cambodia/media/1146/file/Reducing%20Stunting%20Brief%20Report.pdf (accessed August 2019).
Christofides K H Nicola. Scientists are worried about the sugar levels of baby food in South Africa. Quartz Africa 2019. Available online at https://qz.com/africa/1632330/scientists-worry-about-baby-food-sugar-levels-in-south-africa/ (accessed August 2019).
Marais N C, Christofides N J, Erzse A, Hofman K J. Evidence for high sugar content of baby foods in South Africa. S Afr Med J 2019; 109: 328-332.
Murray R D. Savoring sweet: sugars in infant and toddler feeding. Ann Nutr Metab 2017; 70(Suppl. 3): 38-46.
Azad M B, Vehling L, Chan D et al. Infant feeding and weight gain: separating breast milk from breastfeeding and formula from food. Pediatrics 2018; 142: e20181092.
Maunder E, Nel J, Steyn N, Kruger S, Labadarios D. Added Sugar, Macro- and Micronutrient Intakes and Anthropometry of Children in a Developing World Context. PLoS ONE 2015; DOI: 10.1371/journal.pone.0142059.
Acton R B, Jones A C, Kirkpatrick S I, Roberto C A, Hammond D. Taxes and frontofpackage labels improve the healthiness of beverage and snack purchases: a randomized experimental marketplace. Int J Behav Nutr Phys Act 2019; 16: 46.
Baby Milk Action. Guide to UK formula marketing rules - product labelling. Baby milk action IBAFN UK, 2018. Available online at http://www.babymilkaction.org/ukrules-pt4 (accessed August 2019).
Rundall P. STOP PRESS: MEPs call for sugar levels in baby foods to be reduced. Patti Rundall's Policy Blog 2016. Available online at http://www.babymilkaction.org/archives/8192 (accessed August 2019).
Birch L L, Doub A E. Learning to eat: birth to age 2 y. Am J Clin Nutr 2014; 99: 723S-728S.
Bleich S N, Herring B J, Flagg D D, Gary-Webb T L. Reduction in purchases of sugar-sweetened beverages among low-income Black adolescents after exposure to caloric information. Am J Public Health 2012; 102: 329-335.
Roberto C A, Khandpur N. Improving the design of nutrition labels to promote healthier food choices and reasonable portion sizes. Int J Obes 2014; 38 Suppl 1: S25-S33.
Ilic D, Rowe N. What is the evidence that poster presentations are effective in promoting knowledge transfer? A state of the art review. Health Inf Libr J 2013; 30: 4-12.
Acknowledgments
The authors would like to thank the members of the WFPHA who took the photos of the infant formula milk products in their respective countries.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bridge, G., Lomazzi, M. & Bedi, R. A cross-country exploratory study to investigate the labelling, energy, carbohydrate and sugar content of formula milk products marketed for infants. Br Dent J 228, 198–212 (2020). https://doi.org/10.1038/s41415-020-1252-0
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-020-1252-0
This article is cited by
-
Digital marketing of commercial breastmilk substitutes and baby foods: strategies, and recommendations for its regulation in Mexico
Globalization and Health (2023)
-
Plant-based milks: the dental perspective
BDJ Team (2021)
-
Plant-based milks: the dental perspective
British Dental Journal (2020)