Abstract
Complex oral surgery procedures are occurring more commonly in primary care, performed by both specialist oral surgeons and non-specialists/tier 2 providers. Practitioners in the UK are working in an increasingly litigious environment which is often at the forefront of a practitioner's mind and prevention of complaints and claims of negligence is vital in maintaining confidence in our practise. In this ever-increasing litigious environment practitioners need to be aware of the risks associated with oral surgery procedures and have to be able to assess and treatment plan patients effectively and safely. Consent is critical to all procedures, and the recent Montgomery case reinforces the importance of this process which must be individual to each patient. It is vital that as practitioners we are aware of our scope of practice and are able to fully inform patients of the risks and benefits of treatment. Practitioners must know their limits and when to refer on to secondary care. This paper discusses the essentials of risk management in oral surgery and describes key stages in the management of patients undergoing an oral surgery procedure. Initial assessment of the patient, which includes medical and dental history will be discussed followed by investigations to support the clinical diagnosis. Once diagnosis has been confirmed, the process of obtaining consent and the legal implications of this are discussed. Finally, a discussion on the appropriate evidence-based management of common complications which may arise when performing oral surgery will complete the paper.
Similar content being viewed by others
Key points
Oral surgery procedures are more commonplace in primary care and practitioners are working in a increasingly litigious environment.
Reinforces the importance of informed consent following Montgomery.
Practitioners must have an awareness of their limits and refer appropriately.
Discusses common oral surgery procedures and their risk management.
Initial assessment
Often, patients have been referred for oral surgery treatment and will have therefore already been seen by their general dental practitioner (GDP). This is a common occurrence with the tier 2 providers and specialists receiving referrals. However, irrespective of this it is vital that the operating practitioners assess the patient because such an assessment will ensure an accurate diagnosis of any presenting complaint, acting as a sense check on the accuracy of a referral. This will inform the treatment planning discussions. The detailed recording of assessments enables practitioners to have a clear outline of the clinical process leading to the operative treatment. This is important where there is more than one practitioner in the team, one carrying out the assessment and another, the surgery. It is also a vital safeguard in the event of queries, complaints, regulatory investigations or legal claims. While the absence of a record does not mean such actions were omitted, a comprehensive clinical record may prevent a complaint escalating beyond local resolution. In addition, the General Dental Council (GDC) requires registrants to keep 'contemporaneous, complete and accurate patient records'.1
The widely accepted standard in the UK for clinical examination and the recording of such is the Faculty of General Dental Practitioners's (FGDP) Guidelines on clinical examination and record keeping.2 This outlines the steps a clinician should undertake in order to perform and record an acceptable clinical assessment, as well as the precautions that should be taken in relation to the storage of electronic records, graded into 'Aspiration', 'Basic' and 'Conditions' strata. It is expected that all clinicians should record those facets within the Basic categorisation, unless they consider there to be strong reasons for not doing so, in which case the rationale for this should be recorded. One such example may be a patient with complex additional needs who is uncooperative for the assessment of periodontal tissues and the recording of a Basic Periodontal Examination (BPE). In such a situation, it is prudent to record the reasons for not carrying out a significant aspect of the assessment.
Any radiographs received from a referring practitioner should be identified within the clinical record, and the treating clinician should make a note of any relevant features of these images. Existing, relevant radiographs should be carefully examined, and consideration should be given as to whether these are sufficient in themselves for the proposed procedure, in order to prevent unnecessary radiographic exposure.2 In addition, all radiographs taken should be justified, reported and assigned an appropriate quality assurance score as required by current legislation.3
Medical history
It is imperative that all patients undergo medical screening almost invariably with a questionnaire before a consultation or treatment. We are living with an increasingly ageing population and dealing with patients who have multiple co-morbidities affecting treatment. It is mandatory that dental practitioners recognise the importance and relevance of an up-to-date medical history, and it should be noted that it is the responsibility of the dental surgeon to elicit the history, interpret and record it. Completion of pre-printed forms which are uploaded onto a computer database does not fulfil this requirement if they have not been reviewed by the dental practitioner. It is also important to remember that a small, but significant, subset of the population are not able to read and or write. A note needs to be kept on the records to explain why they did not complete a proforma themselves.
Oral surgery procedures are often more invasive and perhaps more stressful than general dental procedures,4,5 and therefore it is of paramount importance that any medical risks are identified preoperatively and discussed with the patient, and where necessary, the physician who cares for the patient.
Clinical assessment
Prior to a medical history the practitioner must enquire as to the symptoms that the patient has had or is suffering from. This should be recorded as the 'presenting complaint' and be recorded in the patient's own words.
The authors suggest adopting a systematic approach to obtaining a medical history. A combination of open and closed questions are essential to gain the full picture of the patient's medical and dental history. It is not within the remit of this paper to discuss in depth specific medical history questions, suffice to say that all systems should be covered and an example of a written questionnaire can be found in Appendix S1 (available in the online supplementary information associated with this paper).
However, it is important that patients are questioned about allergies, the commonest being to medications such as penicillin, and recent national and international press reports of allergies, although food related, have raised awareness of them being commonplace. In cases of reported allergy to medication, further information should be sought as to the reaction type for example, rash, difficulty in breathing, anaphylaxis etc. Patients commonly associate side effects such as gastro-intestinal symptoms with allergies and may self-report an allergy due to this. This information cannot be ignored, but it must be documented then tested and additional information sought, particularly if antibiotics are necessary. It is particularly important to be prepared for anaphylaxis when intravenous medications are delivered for example, antibiotics.
Local anaesthetic allergy, albeit rare, should be taken seriously and investigated further with appropriate immunological referral to confirm as this will prove a significant issue for not only oral surgery procedures but also general dental and any other surgical procedures. Local anaesthetic sensitivities have been reported in up to 30% of patients.6 Chlorhexidine allergy, again rare, but significant has been reported in the national press and literature.7 As this is frequently used in dentistry, both as a mouthwash and handwash or skin preparation, the patient should be asked directly if they have suffered any unwanted effects. There have been two reported fatalities of use of chlorhexidine for irrigation of tooth sockets in 2009 and 2011 and we must therefore be vigilant of this. Interestingly, Bonesvoll8 et al. showed that an average of 4% of the compound chlorhexidine was swallowed, despite only being used as a mouthwash, therefore if there are reports of side effects it would be suggested to avoid use as a mouthwash as well.
We are living in a society with an increasingly ageing population, and people within the UK are living longer than before, which is a major achievement of modern science and healthcare. Older people make up a growing proportion of the population and one in six of the UK population is currently aged over 65 years. It is predicted that this ratio will increase to one in four by 2050. The older population may present a challenge with regards to both surgical and non-surgical treatments in dentistry, in particular the medical aspects.
We should appreciate the increase in recognition of mental health and conditions, such as dementia, in society and the implications this has on both assessment, consent and treatment. Patients may require complex management techniques, such as conscious sedation. Such patients should be assessed appropriately for their anxiety or concerns regarding treatment, and the Intercollegiate Advisory Committee for Sedation in Dentistry standards should be referred to.9
Medications should be recognised and documented, and as discussed above with the ageing population; patients often are prescribed a cocktail of drugs which may either be prescription only or over the counter (OTC).
In recent years we have seen a shift of patients taking warfarin to direct oral anticoagulants (DOACs) such as dabigatran, apixaban and rivoraxaban. Which, although ideal for patients because no regular monitoring is required, has caused concern among the dental profession. The management of patients who are prescribed warfarin is clearly documented,10 and the SDCEP Guidelines11 have been very useful for managing patients on such medications. It is the authors' recommendation that all patients on such medications should be treated routinely with local haemostatic measures (remembering that some contain bovine products and patients should be consented for this) including suturing as routine to assist with haemostasis, irrespective of the appearance of the surgical site. This should also be applied to those on dual anti-platelet or compound medications. The use of platelet rich fibrin (PRF) as an autogenous product for use as a haemostatic agent, but also in the prophylactic management of MRONJ and alveolar ostieitis should also be considered with the appropriate training.12,13
Patients who pose a higher risk of bleeding should be warned appropriately and treated where possible early in the week and early in the day, to allow for management of post-operative bleeding, and consideration should be given to the avoidance of nerve block anaesthesia for the risk of haematoma formation. Clear written post-operative instructions, which must include instructions on how to get urgent help, are important for all patients but in particular those who are at risk of bleeding to allow them to self-manage where possible. Clear guidelines exist for patients taking other medications which may be of concern, such as bisphosphonates and patients taking long-term moderate to high dose steroids remain an area of contention.
Coupled with an increasingly ageing population is the rise in obesity, which is associated with diabetes and its multi-system effects which include, ischaemic heart disease, hypertension and renal failure.
With regards to any medical condition, direct questions should be asked in relation to the stability of the condition and its long-term management. One should be aware of those conditions that may present with an acute exacerbation and how they are managed, eg epilepsy, angina and diabetes, and probing questions should be asked with regards to these conditions. For example:
How often do you have a problem with this condition?
What exacerbates it?
When did you last see your physician regarding this?
Have you ever been admitted to hospital for this condition?
Cardiac issues often seem to be of significant concern more than any other medical issues to dental surgeons. However, there are very few reported cases of cardiac arrest in dental practice. It is important to recognise for any patient's medical condition whether or not that condition is stable or unstable. This allows preparation for any likely 'event'. Although angina features as a common emergency, the most common, unsurprisingly is a vasovagal syncope.14
Key questions for a patient concerning any cardiac condition, should include an enquiry about the precipitating factors for the condition. For example, patients who suffer from angina should be asked about what precipitates their chest pain: is it exercise or does it present when at rest? This allows the clinician to predict the likely onset of the condition. Those who have unstable cardiac conditions should be treated with caution and questioned in detail as to previous events. Often poor pain management of such patients by use of adrenaline-free local anaesthetic can precipitate cardiac events. There is little evidence for the use of adrenaline-free local anaesthetics in dentistry, providing local anaesthetics are administered appropriately and in safe quantities.15
The use of an ASA scoring system (see Table 1) is helpful to categorise patients broadly. As a general rule for invasive treatment, depending on the clinicians' experience, patients who score an ASA grade of III or higher should be considered for onward referral to either a specialist or secondary care facility.
It is a GDC requirement that all members of the dental team are trained to manage medical emergencies appropriately, many dental and oral surgeons treat patients under conscious sedation and such individuals should seek advanced training at either intermediate or advanced life support level via the Resuscitation Council UK. The General Dental Council states that it is essential that all registrants are trained in dealing with medical emergencies, including resuscitation, and possess up to date evidence of competence.16
Diagnosis
Prior to any surgery a definitive diagnosis is required, this must be confirmed with appropriate investigations. Pre-operative imaging should always be considered before surgery to allow planning of the procedure and assist in the consent process. Radiological images allow visualisation of the crown and root of the tooth, apical tissues, surrounding bone and any vital structures that may be relevant to the surgery. Clearly when considering surgery which potentially involves vital structures such as the inferior alveolar nerve, imaging is essential, and advanced imaging such as cone beam CT (CBCT) scanning may be justified. It is important to note that with the advent of CBCT clinicians should be trained to the appropriate level17 when either requesting or reporting such images. Images must be reported according to IRMER18 guidelines, with a quality assurance programme in use.
We have seen a significant shift in the National Health Service regarding the prevention of wrong site surgery, and NHS Providers are encouraged to learn from mistakes and be open and honest to ensure that staff, patients, families and carers feel supported to speak up in a constructive way.19 The WHO Surgical Safety Checklist was launched in 200920 and allows 'phases' of treatment to be checked before a procedure commencing. Within trusts it is essential that such a checklist is documented before any procedure to minimise the risk of a an adverse outcome including a never event. Although the WHO checklist hasn't been specifically developed for dental procedures, there are other recommendations such as National Safety Standards for Invasive Procedures (NatSSIPs)21 and NHS providers who have developed their own Local Safety Standards for Invasive Procedures (LocSSIPs).22 Checklists are only valid if the initial diagnosis and treatment plan is correct and the patient has given valid consent. In primary care settings systems need to be developed that utilise the checklist philosophy of error reduction.
In the authors' experience the following procedures within oral surgery are fraught with potential difficulties:
Two adjacent lone standing molars which have been charted by a colleague as second and third molars, and the patient has been listed for extraction of the first molar
Multiple supernumaries and orthodontic extractions which may contain typographical errors
Transposition of left and right on the charting or referral letter.
It is suggested that for such extractions, referrals should document the tooth/teeth for extraction in both words and charting and this should be confirmed with the patient at the start of any consultation, as per the WHO surgical checklist.23
Consent
Practitioners must obtain appropriate, valid consent before carrying out any procedure. A failure to obtain such consent may leave a clinician vulnerable to an allegation of the crime of battery. In addition, the GDC have highlighted to their decision makers that valid consent is 'a cornerstone of the public interest'24 and that a failure to obtain consent should be viewed seriously when considering allegations against a dental professional.
In obtaining consent from patients, it is essential that the discussions around any proposed intervention are clearly recorded within the clinical records. The records must reflect the treatment options given to the patient, along with material risks and benefits, including the possibility of providing no treatment at that time. Any specific concerns raised by a patient should be noted, as these must be actively considered when deciding on the most appropriate treatment plan in the circumstances. It is further recommended that any resources provided to a patient to enable them to make an informed decision are noted within the records, and that the reasons for choosing certain treatment options over other alternatives are recorded.
With the advent of the Mental Capacity Act 2005,25 and similar legislation in Scotland26 Northern Ireland27 and Ireland,28 practitioners have a duty to ensure that steps are taken to ascertain whether patients have the requisite capacity to make the decision in question at the time it needs to be made, following the two-stage test set out by the Act. The steps taken to ascertain capacity should also be recorded within the clinical records, and it may be considered good practice to note the involvement of other individuals (for example, family members, support workers or an Independent Mental Capacity Advocate or equivalent, having sight of the certificate of incapacity29) who have been involved in the consent process, should queries be raised at a later stage.
In relation to written consent, it is recommended that complex procedures should necessitate the use of a written consent form,1 although there is only a legal requirement for such paperwork in relation to procedures taking place under conscious sedation or general anaesthetic. Practitioners must be alert to the fact that the obtaining of written consent does not constitute blanket acceptance of the proposed treatment, and that consent should be revisited at every subsequent appointment within the treatment pathway, and all of these discussions are reflected in the clinical records.
GDC Standards and the law require clinicians to both ensure that patients are given relevant information about any proposed treatment (including costs) and that this information is delivered to patients in an appropriate manner so that they are able to understand what is proposed.1 Recent developments in case law, as set out in the case of Montgomery,30 have served to further clarify the nature of information provided to patients, stating that there is a duty to ensure patients are informed of the 'material risks' attached to a procedure. The test for materiality has been defined as 'whether, in the circumstances, a reasonable person in the same position as the patient would be likely to regard a particular risk as significant, or the doctor was or should reasonably be aware that the patient would be likely to attach significance to it'. While it was recognised that it is acceptable to withhold information if it was reasonably considered that such information may be 'seriously detrimental' to a patient's health, this 'therapeutic exception' is considered a limited exception to the principles outlined above. Montgomery has played a significant part in abolishing the paternalistic approach historically taken by the medical profession to consent and has highlighted the need to consider the circumstances of the individual patient as part of the process. Relevant examples in the field of oral surgery may include the impact of nerve damage on an individual patient, taking into account the implications this may have, for example, on the career of a professional musician specialising in woodwind or brass instruments.
Paperwork pertaining to consent, including copies of signed consent forms, should form part of the clinical record for a patient, and should be securely stored as per current good practice and in line with legislation.31,32
Complications and consequences
As with all surgery, appropriate warnings for all patients should include the risk of pain, swelling, bleeding, bruising and infection. In addition to this, despite risk factors documented with regard to exodontia and alveolar osteitis, it is recommended that all patients be warned about this complication irrespective of their risk factors as it is the commonest complication from exodontia.33 This also applies where the risk of a root fracture or displacement of a root is likely.
Fracture of the tooth or root should also be discussed, in particular in those patients who have unfavourable root formation. If it is felt that removal of the tooth is outside of the competency of the practitioner, then an onward appropriate referral should be offered. It is critical to have an insight into one's own ability and limitations and the GDC consider this important.
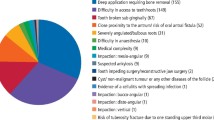
Some procedures will predispose patients to more significant complications, and this may be compounded by the patient's own risk factors. There are a variety of complications reported in the literature34 associated with oral surgery, and as with all surgery, modern methods should be used where appropriate to minimise risk, it is indefensible to use air turbine driven hand pieces (unless they have a reverse exhaust) once a flap involving the periosteum has been raised, to decoronate teeth, section roots or remove bone. Surgical emphysema35,36 albeit rare, can be a serious complication requiring hospitalisation, and is often due to the use of an air driven hand piece for both surgical and restorative procedures, and should therefore be avoided.
Maxillary surgery
Maxillary premolars and molars may cause concern for the risk of an oro-antral communication (OAC) (as shown in Fig. 1) and if not diagnosed and managed appropriately, the development of an oro-antral fistula (OAF) can follow. Plain film imaging is not an accurate predictor of likelihood of OAC post extraction (Fig. 2) and therefore patients should be warned of the risk of an OAC and the potential signs post operatively and management. CBCT is the only definitive modality of imaging to predict such a complication.37
Fractured roots which may be displaced into the antrum should be discussed including the risk of admission and further surgery. A fractured maxillary tuberosity is often the concern of many practitioners but in reality, may go unnoticed without any symptoms from the patient. A significant tuberosity fracture is more likely in the elderly patient with a lone standing posterior maxillary molar which may then lead to an OAC.
It is important to discuss this complication and its perspective, and wording such as 'fractured jaw' should be re-phrased to ensure the patient has full understanding. In a similar situation, a tear of the palatal mucosa leading to soft palate haemorrhage can be daunting especially if the palatine vessels are involved. Sinus surgery is not discussed here, suffice to say it requires specific training.
Surgery elsewhere in the maxilla such as surgical endodontics, or removal of impacted teeth can carry additional risks with regards to the antrum and the floor of nose and appropriate imaging is often required in planning and obtaining consent for such surgery.
Mandibular surgery
The removal of mandibular third molars has been discussed in the literature on many occasions, more so since the publication of the NICE guidelines for third molar removal.38 Patients should be warned about the material risks of third molar surgery which include the temporary or permanent damage to the inferior alveolar nerves, lingual nerves and chorda tympani.39 There are a variety of papers discussing percentage risk of injury; however, it is not within the remit of this paper to discuss nerve injury but radiographic signs should be taken into consideration when discussing surgery,40 as illustrated in Figure 3.
Surgical technique should be adapted to minimise the risk of nerve injury and dated methods, such as the lingual split technique and routine lingual flap, and nerve retraction should be avoided where possible.
When coronectomy is planned, the patient must understand during the consent process that the aim of the procedure 'is intended for a coronectomy to be undertaken, however, if the roots are mobilised during surgery, they will require removal, with the heightened risk of nerve injury'.41 Additionally, the risk of a failed coronectomy should be discussed, and the risk of a second procedure at a (much) later date should the roots become symptomatic.42 It is also important to note that appropriate training before carrying out a coronectomy should be sought as this is a technique sensitive procedure.
Records
The GDC's Standards,1 at 4.1.1, state that the clinical records for a patient are not restricted to the records made during an appointment, but also include consent forms, recordings, clinical photographs, referral letters, laboratory forms and other correspondence. It is therefore incumbent on a practitioner to retain copies of any referral paperwork (including both inward and outward referrals as well as discharge letters sent to referring practitioners) within the clinical records for each individual patient. The methods of storage of such correspondence will vary between practices, from storage within paper records to scanning onto an electronic record. Whatever method of storage is employed, appropriate measures should be taken to ensure all documents pertaining to a patient are securely stored and in a way that they can easily be collated and disclosed on receipt of a subject access request.31
This does not necessarily mean that generic information given to a patient, eg information leaflets, should also be scanned or a copy stored in the records. In such situations, it is good practice to simply make a record of the information given and the form in which it was given (eg post-extraction instructions leaflets, computer demonstrations, websites identified) in the contemporaneous record. However, it is important to be mindful of version control, keeping dated copies of the historical leaflets in the practice as they are updated from time to time.
Data security has long been a prominent issue in relation to confidential material, both within the medical professions and in other walks of life. The GDC requires dental professionals to take steps to keep patient data confidential and to ensure the security of patient information.1 Examples of methods that may be used to ensure data security include the use of password protection, secure backups and the use of encrypted electronic transfer methods, eg secure data sticks or nhs.net email addresses.
The Data Protection Act 2018 which brought into effect the General Data Protection Regulations (GDPR)32 in the UK has imposed further requirements on dental practices in relation to the recording and processing of personal data. Practitioners should be aware of the impact this has on the use of patient data and be mindful of this in everyday practice.
Conclusion
Thorough assessment, investigations, diagnosis and appropriate treatment planning are key to safe and appropriate treatment. The consent process must be robust enough for patients to appreciate their options, and no treatment must always be considered irrespective of the symptoms.
Where practitioners are contemplating oral surgery procedures, they should be mindful of the risks and benefits of surgery and reflect on their limitations. It is imperative to involve patients in treatment decisions, and adequate consent must be obtained.
Treatment should be completed in a safe environment with appropriate checks in place, and clear written and verbal post-operative instructions with emergency contact details should be given to patients. Post-operative calls after surgery, usually within 72 hours, are suggested to enable any advice to be given to patients to alleviate any early issues. This also gives the practitioner opportunity to re-appoint patients with concerning symptoms.
When complications occur, practitioners must appreciate the seriousness of these and refer appropriately both in a timely manner to a suitably trained colleague.
References
General Dental Council. Standards for the Dental Team. 2013.
Faculty of General Dental Practice. Clinical examination and record-keeping. 3rd ed. London: FGDP, 2016.
Faculty of General Dental Practice. Selection criteria for dental radiography standards. 3rd ed. London: FGDP, 2018.
Wong M, Lytle W R. A comparison of anxiety levels associated with root canal therapy and oral surgery treatment. J Endod 1991; 17: 461.
Stabholz A, Peretz B. Dental anxiety among patients before different dental treatments. Int Dent J 1999; 49: 90.
Assem E S, Punnia-Moorthy A. Allergy to local anaesthetics: an approach to definitive diagnosis. A review with an illustrative study. Br Dent J 1988; 164: 44-7.
Pemberton M N, Gibons J. Chlorhexidine and hypersensitivity reactions in dentistry. Br Dent J 2012; 213: 547-550.
Bonesvoll P, Lokken P, Rolla G, Paus P N. Retention of chlorhexidine in the human oral cavity after mouth rinses. Arch Oral Biol 1974; 19: 209-212.
Standards for Conscious Sedation in the Provision of Dental Care. Report of the Intercollegiate Advisory Committee for Sedation in Dentistry 2015. The Dental Faculties of the Royal College of Surgeons and the Royal College of Anaesthetists.
Perry D J, Noakes T J C, Helliwell P S. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. Br Dent J 2007; 203: 389-393.
Scottish Dental Clinical Effectiveness Programme. Management of dental patients taking anticoagulants or antiplatelet drugs. Dental Clinical Guidance. August 2015. Available online at http://www.sdcep.org.uk/wp-content/uploads/2015/09/SDCEP-Anticoagulants-Guidance.pdf (accessed February 2019).
Fernando de Almeida Barros Mourão C, Calasans-Maia M D, Del Fabbro M3et al. The use of platelet rich fibrin in the management of medication related osteonecrosis of the jaw. A case series. J Stomatol Oral Maxillofac Surg 2019; DOI: 10.1016/j.jormas.2019.02.011.
Eshghpour M, Dastmalchi P, Nekooei A H, Nejat A. Effect of platelet rich fibrin on frequency of alveolar osteitis following mandibular third molar surgery: a double blinded randomised clinical trial. J Oral Maxillofac Surg 2014; 72: 14631467.
Girdler N M, Smith D G. Prevalence of emergency events in British dental practice and emergency management skills of British dentists. Resuscitation 1999; 41: 159-167.
Niwa H, Sugimura M, Satoh Y et al. Cardiovascular response to edrenaline-containing local anaesthesia in patients with cardiovascular disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 610-616.
General Dental Council. Scope of practice. Available online at https://www.gdc-uk.org/information-standards-guidance/standards-and-guidance/scope-of-practice (accessed February 2019).
Brown J, Jacobs R, Levring Jähagen E et al. Basic training requirements for the use of dental CBCT by dentists: a position paper prepared by the European Academy of DentoMaxilloFacial Radiology. Dentomaxillofac Radiol 2014; 43: 20130291.
Ionising Radiation Regulations: requirements (IRMER). Gov.UK Available online at https://www.gov.uk/government/publications/the-ionising-radiation-medical-exposure-regulations-2000 (accessed February 2019).
The future of NHS patient safety investigation: engagement feedback. November 2018. Available online at https://improvement.nhs.uk/documents/3519/Future_of_NHS_patient_safety_investigations_engagement_feedback_FINAL.pdf (accessed online March 2019).
WHO. WHO surgical safety checklist and implementation manual. Available online at https://www.who.int/patientsafety/safesurgery/ss_checklist/en/ (accessed February 2019).
National Safety Standards for Invasive Procedures (NatSSIPs). Available online at https://www.england.nhs.uk/wp-content/uploads/2015/09/natssips-safety-standards.pdf (accessed February 2019).
NHS Improvement. Examples of local safety standards for invasive procedures. Available online at https://improvement.nhs.uk/resources/examples-local-safety-standards-invasive-procedures (accessed February 2019).
World Health Organisation. WHO Surgical Safety Checklist. Available online at https://www.who.int/patientsafety/safesurgery/checklist/en/ (accessed July 2019).
Case Examiner Indicative Outcomes Guidance. Available online at https://www.gdc-uk.org/about/who-we-are/committees/case-examiners (accessed February 2019).
Mental Capacity Act 2005 c.9. Available online at https://www.scie.org.uk/mca/introduction/mental-capacity-act-2005-at-a-glance (accessed June 2019).
Adults with Incapacity (Scotland) Act 2000 asp 4. Available online at https://www2.gov.scot/Publications/2008/03/25120154/1 (accessed June 2019).
Mental Capacity Act (Northern Ireland) 2016 c.18. Available online at http://www.legislation.gov.uk/nia/2016/18/contents/enacted (accessed June 2019).
Assisted Decision-Making (Capacity) Act 2015. Available online at http://www.irishstatutebook.ie/eli/2015/act/64/enacted/en/html (accessed June 2019).
Certificate of incapacity under section 47 of the Adults with Incapacity (Scotland) Act 2000 Available online at https://www2.gov.scot/Topics/Justice/law/awi/forms/Medical-Report-Forms/5299 (accessed June 2019).
Montgomery v Lanarkshire Health Board [2015] 2 All ER 1031.
Data Protection Act 2018 c.12.
Data Protection Act 2018 c.12 ss 6-20.
Kolokythas A, Olech E, Miloro M. Alveolar osteitis: A comprehensive review of concepts and controversies. Int J Dent 2010; 249073.
Yamashita D D R, McAndrews J P. Complications in dentoalveolar surgery. Oral Maxillofacial Surg Clin N Am 2011; 23: ix.
Aslaner M A, Kasap G N, Demir C, Akkas M, Aksu N M. Occurance of pneumomediastinum due to dental procedures. Am J of Emerg Med 2015; 33: 125. e1-3.
Ali A, Cunlifee D R, Watt-Smith S R. Surgical emphysema and pneumomediastinum complicating dental extraction. Br Dent J 2000; 188; 589-590.
Nedblaski T R, Laskin D M. Use of panoramic radiography to predict possible maxillary sinus membrane perforation during dental extraction. Quintessence Int 2008; 39: 661-664.
NICE. Guidance on the Extraction of Wisdom Teeth [Ta1]. 2000. Available online at https://www.nice.org.uk/guidance/ta1 (accessed June 2019).
Loescher A R, Smith K G, Robinson P P. Nerve damage and third molar removal. Dent Update 2003; 30: 375-382.
Umar G, Bryant C, Obisesan O, Rood J P. Correlation of the radiological predictive factor of inferior alveolar nerve injury with cone beam computed tomography findings. Oral Surg 2010; 3: 72-82.
Frafjord R, Renton T. A review of coronectomy. Oral Surg 2010; DOI: 10.1111/j.1752-248X.2010.01079.x.
Pellatt A, Bhola S, Collin J, Cobb A. A delayed and severe presentation of coronectomy complications. Oral Surg 2019; 12: 260-263.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Moore, R., Miller, R. & Henderson, S. Risk management in oral surgery. Br Dent J 227, 1035–1040 (2019). https://doi.org/10.1038/s41415-019-0989-9
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0989-9