Abstract
Introduction Upon completion of dental foundation training (DFT), a number of dental graduates apply for further training known as dental core training (DCT). Alternatively, there are two-year integrated training pathways within both primary and secondary care; known as longitudinal dental foundation training (LDFT). There is a lack of evidence supporting LDFT and how this compares to DFT and DCT.
Aim To explore perceptions and experiences of three post-qualification dental training pathways (DFT, DFT+DCT1, LDFT) and understand how this training prepares trainees for independent clinical practice and their future career.
Method A qualitative study, employing a 'grounded theory' approach. Theoretical sampling was carried out until data saturation was achieved; 36 individual in-depth semi-structured interviews of trainees and supervisors were conducted. Data analysis was iterative and inductive. The development of codes and generation of sub-themes resulted in major themes grounded within the data of participants.
Results Seven major themes were generated: training pathway choice, skill development, career development, identity, team, setting and training programme.
Conclusion The first part of this short series provides an understanding of perceptions of the different training pathways and factors considered when choosing a training pathway; in particular the impact of the recruitment process, peer opinion and service pressures.
Similar content being viewed by others
Key points
-
Identifies current perceptions of dental foundation training, dental core training and longitudinal dental foundation training.
-
Reports the expectations of trainees and considerations when applying for post-qualification dental training.
-
Identifies aspects that can influence trainee choice when applying for post-qualification dental training such as recruitment process, peer opinion and service pressures.
Introduction
Upon completion of undergraduate dental training, dental foundation training (DFT) is a mandatory one-year training programme based within primary dental care for all graduates of British dental schools who wish to practise dentistry within the NHS. With successful completion of DFT allowing entry to the NHS Dental Performers List,1 many dentists then go on to work independently as a general dental practitioner (GDP). However, a number of dental graduates opt for a longer training period post qualification as a full-time trainee. On completion of one-year DFT, some apply to 12 months (or longer) of dental core training (DCT) with the majority of these posts based within secondary care. Alternatively, there are two-year integrated training programmes based within both primary care and secondary care; known as longitudinal dental foundation training (LDFT) in Yorkshire & Humber. Health Education England across Yorkshire and Humber (HEEYH) provide opportunity for the recently qualified dental graduate to complete one of three training pathways which are summarised in Figure 1.
Dental foundation training
The primary purpose of DFT is development of 'competent, caring, reflective practitioners who can consistently provide safe and effective care for patients in a primary care setting'.2 This one-year period of training combines experiential learning within primary dental care, with a minimum of 30 study days, targeting specific areas of the DFT curriculum.2 The majority of DFT training posts are based within one dental practice, with the trainee providing NHS General Dental Services (GDS) under the supervision of one educational supervisor. Historically, the term 'trainer' was used in DFT until the recent change in term to 'educational supervisor'. Therefore, the terms 'supervisor' and 'trainer' may be used interchangeably within part 1 and part 2 of this paper. Funding of DFT is now part of the overall budget for Health Education England (HEE)1 and HEE spends £88.7 million on 848 DFT commissions per year, an average of £104,599 per trainee.3 There have been a number of studies looking at experiences of DFT.4,5,6,7,8,9,10 In 2007, it was reported that no trainee would have wanted to enter practice without this training year.7 In 2014, over 90% of trainees felt that their experience of DFT was either excellent or good, however 40% felt there were gaps in their clinical experience.5 DFT plays an increasingly important role in the development of a safe, independent practitioner,3 particularly with the suggestion that there may be some areas of weakness in the clinical skills of new dental graduates compared with previous years.11
Dental core training
There is no mandatory requirement for any dental graduate to undertake DCT. For many years, DCT was known as a senior house officer (SHO) post based mainly in oral & maxillofacial surgery (OMFS) departments. It has been renamed several times in recent years until its current term, DCT. Currently, there are approximately 600 DCT posts in England.3 The majority of DCT posts offer training linked to only one speciality area, usually OMFS, but there are some posts based in other dental specialties in dental hospitals and a few in the salaried/public dental service.12 Until 2016, there was no formal curriculum for DCT and the design of training posts was ad hoc dependent on the type of post and setting.12 DCT now has an educational programme with study days, assessment, portfolio and dedicated supervisors. The DCT curriculum sets out a number of objectives for DCT, some of which include learning from different supervisors in different settings, becoming part of a multidisciplinary team and developing preference of career choice.12 DCT has significant scope for flexible career opportunities3 with multiple endpoints and varied duration from one to three years.12 Dental trainees normally choose to pursue DCT immediately following completion of DFT, applying through the national recruitment process. They can choose to complete 1, 2 or 3 years in DCT posts but have to re-apply each year through national recruitment.
National surveys of SHOs in OMFS have been completed in the past.13,14,15 In 2012, approximately 50% of trainees chose the post in order to improve their oral surgery skills and just under a quarter were interested in OMFS as a speciality or wanted to specialise in the future.15 Only 3% felt that the post was not relevant to their career and trainees reported that the best aspects included improving skills in dentoalveolar surgery and increased confidence managing patients with medical conditions.15 However, lack of medical knowledge, being on-call at night and ward duties were the worst aspects of the post.15 In a regional survey of SHOs within various dental specialities16 'understanding the role of the hospital dental service' and 'learning from experienced clinicians' were common perceived benefits.
Longitudinal dental foundation training
A two-year integrated programme within different clinical settings was first introduced in England and Scotland in 1996. By extending the supported and supervised environment for a second year, this two-year programme aimed to broaden trainee experience in both primary and secondary care, thereby improving standards of patient care and enabling trainees to make an informed career choice.17,18 An independent evaluation17 of this two-year programme in Scotland was found to offer an improved understanding of primary and secondary care with suggestion that trainees gained more advanced clinical skills, greater adaptability and helped to inform career decisions.17 However, concerns included lack of continuity of patient care within the six-month blocks of hospital/community settings and organisational and infrastructural issues.17
Twenty-three years on from this initial pilot programme,17 2-year integrated training programmes are still available to the new dental graduate but are now only within England and there are only 24 places each year in two regions: Yorkshire & Humber and the North East.3 Previously known as longitudinal dental foundation training (LDFT), DFTDCT (Longitudinal) is now the term used for the two-year integrated training pathway provided by HEEYH. The change in terminology was to improve recognition and understanding of the training pathway and occurred while this research was being conducted, therefore for the purposes of this study, the term LDFT will continue to be used throughout this paper. A similar two-year scheme run by Health Education England across the North East (HEENE) is referred to as general professional training (GPT). These integrated two-year training programmes vary with regards to the speciality, duration and timing of rotations19 but combine the elements of both DFT and DCT year 1, with trainees working in both primary and secondary care environments over the two years.20
The LDFT scheme introduced in 2010 by HEEYH, offers an integrated programme with trainees working in both primary and secondary settings over a split- or alternate-week rotation throughout the two years. There is a dedicated training programme director (TPD) and study programme. Six dental practices each year are paired to a secondary care placement based within various settings; hospitals and community dental clinics. Trainee experience varies dependent on placement including opportunities for experience in OMFS, oral surgery, restorative, orthodontics, paediatric and special care dentistry.
Rationale for research
With post-qualification training playing an increasingly important role in the development of a safe, independent practitioner,3 standardised, high quality training is essential for the newly qualified dental graduate. To practise dentistry within the NHS, the newly qualified dental graduate must complete a one-year DFT training programme based within one primary dental care setting under the supervision of one educational supervisor. In contrast to this, medical graduates complete a two-year foundation programme across different specialties, different healthcare settings, with a number of supervisors.21 This two-year medical foundation programme was identified to be broadly comparable to the integrated two-year LDFT programme within dentistry.22,23 The need to fully scope and evaluate the LDFT training model has been identified.3 With the exception of a study exploring a pilot two-year integrated programme in Scotland over twenty years ago,17 there appears to have been no further research into an integrated two-year post-qualification dental training programme and a lack of evidence comparing the three different post-qualification dental training pathways: DFT, LDFT and DFT+DCT1.
Aim and objectives
The aim of this qualitative study was to explore perceptions and experiences of the three post-qualification dental training pathways provided by HEEYH and to understand how this training prepares trainees for independent clinical practice and their future career.
The objectives were:
To understand perceptions of the three different training pathways; LDFT, DFT, DFT+DCT1 within HEEYH
To examine the reasons for choice of training pathway from a trainee perspective
To discover how well the training pathway prepares trainees for independent clinical practice and future career prospects
To explore any recurring themes or differences in perceptions of the three different training pathways.
Method
This inductive study used a 'grounded theory' approach, as described by Glaser and Strauss.24 Grounded theory enables detailed exploration, with theoretical sensitivity, to construct theory grounded in data.25 By exploring the views of participants through semi-structured interviews, theories were generated and 'grounded' within the data of participants. Ethical approval was granted by The Hull York Medical School.
Recruitment & sample
Purposeful sampling was employed, intentionally selecting individuals and sites to understand the central phenomenon of post-qualification dental training pathways.26 HEEYH provides these dental training pathways and therefore trainees of HEEYH are suitable candidates to understand the central phenomenon of post-qualification dental training pathways. Theoretical sampling was carried out; the sample was intentional, based on the codes and concepts identified from iterative data analysis and further sampling focused on further development and generation of theory.24,26,27 Emergent data analysis confirmed that collecting data from other sources such as supervisors and subsequently TPDs of the HEEYH post-qualification dental training pathways would be beneficial. This also provided triangulation of evidence as trainee perception of successful training may have been different to that of their supervisors.
Recruitment was advertised via correspondence by HEEYH personnel to DCT, LDFT, DFT trainees and supervisors and TPDs of these training programmes. Trainees and supervisors approached the researcher via email if interested in the project, a participant information sheet and a minimum of one week was given to consider participation in the study. If they wished to take part, a consent form was given and subsequently signed. On enrolment to the study, all participants were given a unique participant identifier number in order to maintain anonymity. Participants were informed that any identifiable data would be stored securely and only accessible to members of the research team and all data that were analysed and published would be anonymous with confidentiality maintained.
Data collection & analysis
Individual, face-to-face, in-depth interviews were carried out in order to obtain a detailed personal focus from participants, exploring perceptions and experiences. Interviews were carried out by the primary researcher (AJ Coleman) at a time and location convenient to the participant and where confidentiality could be maintained. A semi-structured interview schedule was used to ensure areas of interest were covered with the flexibility to react, clarify or probe further to gain a deeper understanding.28 The interview schedules were based on guidance by Cresswell,26 with open-ended questions written in order to address the objectives of the study. A group of trainees and supervisors were asked to comment and assist with the development of the interview schedule, participant information sheet and consent form. Data derived from interviews were collected by audio recordings and then transcribed verbatim. As the primary researcher had prior knowledge and experience of DFT and DCT, reflexivity was essential. A research journal was kept by the researcher which allowed identification and reflection upon any biases, values and personal background that may have shaped interpretations of this study.29 The second researcher (G M Finn) had no prior knowledge or experience of dental training pathways and both researchers discussed reflexivity in order to identify potential biases. Transcripts, interview notes and research journal notes were used when analysing data. In line with grounded theory,24 open, axial and selective coding occurred. Iterative data analysis allowed reflection upon findings to inform and modify data collection accordingly and identify when data saturation was achieved. Data collection was ongoing until data (theoretical) saturation was achieved.24,26,30 Ultimately, the theory generated was grounded within the data of participants.
Data validation
A number of strategies were employed to validate data to determine accuracy and credibility of findings.26 Triangulation was achieved by carrying out interviews of trainees, supervisors and TPDs of the three different training pathways. During data analysis, the transcripts, interview notes and the use of a research journal were used. To minimise the impact of single-researcher bias, independent coding was carried out by both researchers and themes agreed upon through a process of negotiation. Peer review was completed in order to cross-check transcription and coding.29 Data analysis was further validated by member-validation,31 all participants were emailed a summary of the themes derived from data analysis and feedback invited as to whether interpretations were fair and representative.
Results
A total of 36 individual semi-structured interviews were conducted. These included:
LDFT trainees - majority training within at least two different dental specialties in addition to primary dental care. Dental specialties included OMFS, paediatric dentistry, orthodontics, restorative dentistry and special care dentistry. Settings included dental practices, hospitals and community clinics
DCT1 trainees - all based within OMFS but in different training locations. (representative as majority of DCT1 posts are in OMFS)
Previous DFT trainees now working as a GDP, with no experience of DCT/LDFT. This group was 14-23 months post-qualification, so a similar stage to LDFT & DCT1 participants. The term 'DFT trainee, now GDP' shall be used for quotations by this group of participants.
Supervisors and TPDs of the three different training pathways. The majority had experience of more than one training pathway. For anonymity purposes, the broad term 'supervisor' shall be used for quotations by supervisors and TPDs.
Major themes generated
Iterative data analysis resulted in seven major themes (demonstrated in Fig. 2): training pathway choice, skill development, career development, identity, team, setting and training programme.
It is not possible to discuss each major theme in detail within this publication. Upon agreement by the research team, five themes were chosen for discussion due to their recurring prevalence within the data and relevance to the research question. The theme 'training pathway choice' will be discussed in detail in this paper (Part 1) to address the first two research objectives:
To understand perceptions of the three different training pathways; LDFT, DFT, DFT+DCT1 within HEEYH
To examine the reasons for choice of training pathway from a trainee perspective.
Part 2 of this two-part series will discuss: skill development, career development, identity and team to address the final two research objectives:
To discover how well the training pathway prepares trainees for independent clinical practice and future career prospects
To explore any recurring themes or differences in perceptions of the three different training pathways.
Major theme: training pathway choice
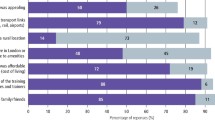
Figure 3 provides a diagrammatic representation of the seven sub-themes of the major theme: 'training pathway choice'.
Expectations of training pathway
Generally, DFT was viewed as an opportunity to consolidate general dentistry skills learnt during undergraduate training before independent clinical practice.
'…a transition year where you're making decisions for yourself, treating things on your own…I just don't think it would be safe, after you've left dental school, to be completely left on your own, so I think it's a transition year between dental school and then being an associate.' DFT trainee, now GDP.
Trainees often applied for DCT with the hope of improving surgical extraction skills, understanding secondary care and the management of medically compromised patients.
'I wanted to…get more experience with surgical extractions…being able to recognise ill patients and knowing how to manage them and when to refer to hospital for care.' DCT trainee
Whereas some applied for DCT with a clear purpose of wanting to specialise in the future.
'I wanted to specialise eventually…I knew that it [DCT] was something I needed to do…. see things from a different aspect in terms of how to manage medically compromised patients…and…be able to develop academically in terms of…posters, presentations, publications...' DCT trainee.
LDFT was perceived to provide more of a broad experience to help inform career decisions. 'I could then have both general practice and hospital training at the same time and then decide by the end of two years which I liked better and which environments suit me best…' LDFT trainee.
'…(LDFT) you're getting the best of both worlds…speak to…different professions, get their experience, have a feel first hand at what happens in a hospital and primary care setting…you might get an affiliation for a particular skill, you might absolutely hate one, love the other….' Supervisor based in primary care.
Perceptions of different training pathways
OMFS-only posts appeared to put some trainees off pursuing DCT, whereas training posts within other areas of dentistry could be more appealing.
'… you can get put in some very medical posts… we're not trained to do that at all, so if I'd have been landed with that, I'd have just felt very uncomfortable and I'm sure I would have been very unhappy…if I could have landed like a very dental specific like year, then I think I would have liked to have done that…' DFT trainee, now GDP
Peer opinions seemed to influence decisions as to whether to pursue DCT.
'It [DCT] crossed my mind but the only reason it did so was because of sort of peer pressure and…being a sheep. All of my friends were doing it so I thought am I making the right decision by staying in practice?… I thought I'd actually rather just get stuck in and be good at doing good dentistry,…' DFT trainee, now GDP.
Some preferred the option of being immersed fully within one speciality (DFT+DCT1) and highlighted concerns about splitting time across different clinical settings (LDFT).
'I was just apprehensive that I wouldn't get the full benefit of either if I did a longitudinal…scheme. I thought it would be better to, you know, throw yourself…a hundred percent into practice for a year and then a hundred percent into working in a hospital for a year… I just felt like you wouldn't gain the true experience if you were sort of chopping and changing between the two…' DCT trainee.
However, in contrast, working simultaneously in different settings was perceived to be an advantage.
'…if I had have done say DFT then (DCT1)… maybe slightly deskilled, whereas I thought, if I'm doing both simultaneously I'll not have the opportunity to deskill.' LDFT trainee.
'I think they're probably…too early in their career… to focus on one (monospeciality)… if you could experience, you know, oral surgery or paediatrics or ortho, or restorative, all within that time I think it will help them in their career pathway…' Supervisor based in secondary care.
The advantages of experience in different aspects of dentistry was identified in LDFT.
'…having a parallel mix of everything's good, especially if you're more focused on the dental side of it like… advanced restorative or paeds because I probably won't use the maxfax stuff…' LDFT Trainee.
However, there did appear to be a lack of awareness among trainees of what LDFT was and what it involved.
'…because I was trained at Newcastle, I knew roughly what the scheme involved on the two-year course there but I didn't know what the Yorkshire scheme involved and I don't think anyone really knew until they were told what job they'd got…' DFT trainee, now GDP.
Service pressures
OMFS as a speciality and the hours of work appeared to put some trainees off applying for DCT.
'…a year doing maxillofacial surgery, which is the most common one really isn't it?.doing that on-call and night shifts, just sounds horrific and terrifying for people and I think it really puts them off.' DFT trainee, now GDP.
The perception of a hospital hierarchy was also a concern among some.
'…a few of my friends had told me…there's quite a hierarchy, so not necessarily being spoken to as I would like…I would get walked all over…getting all the rubbishy jobs even off like colleagues in the same position as me…' DFT trainee, now GDP.
'…some people like the order of secondary care, they like to see that kind of almost that hierarchy and they fit into that culture really well, whereas other people hate that culture…' Supervisor based in primary care.
In contrast to this, a DFT trainee reflected upon some choosing DCT to avoid pressures of working under an NHS contract in general dental practice.
'…can only speak from what my friends have said….(they) don't want to work under the UDA system (NHS GDS contract) and they want to be salaried… we know how much we're getting, we can do the best for the patient…therefore I'm going to stay in hospital for as long as humanly possible.' DFT trainee, now GDP.
Recruitment process
Generally, LDFT was viewed as a competitive post and only provided in certain areas which may have put some trainees off applying for this post.
'I think the longitudinal schemes you're a lot more limited as to where you can live… as far as I'm aware there's two places in the whole of Leeds, so, you know, it's going to be quite competitive to get in there, quite unlikely that I might get that position, so … I played it safe…went for the other one (DFT)…' DFT trainee, now GDP.
The introduction of national recruitment was perceived by some as a barrier to applying for DCT.
'I think it (national recruitment) deters people from wanting to progress because sometimes it's just not feasible, to apply to somewhere like Cornwall or somewhere so far when you've got family or kids or partners.' DCT trainee.
Trainees focused on the benefits of a 2-year programme (LDFT) versus having to apply to national recruitment for DCT after DFT.
'… (LDFT) would make it extremely desirable…I think the idea of having to go through national recruitment which frankly is not the nicest thing in the world to do that for your FD and then have to do it again for your DCT can put a lot of people off.' DFT trainee, now GDP.
LDFT trainees did however describe issues when applying for DCT2 posts through national recruitment.
'…when I applied for national recruitment this year, they were baffled by my post…that was a bit of a disaster…had an email saying can you explain to us what you do?' LDFT trainee.
Finance
Potential earnings did influence trainee decision on training pathways.
'I am glad that I did the FD, because now it means that I can be an associate and I know this sounds horrendous but the wages are a lot better…, whereas on LDFT you are on the same salary I believe or very similar…and now I've just bought a house, it's important that I can pay the mortgage…' DFT trainee, now GDP.
However, the job security of a two-year programme in LDFT was highlighted as an advantage.
'…you don't have to faff around after six months looking for another job … you know you're going to be there for two years, you know you're going to be working, not going to be moving around, finding a flat, so yeah, the job security is pretty good.' LDFT trainee.
Location
Location appeared to be an important consideration when trainees were choosing their training pathways.
'…these DCT jobs are only for a year… is it worth it moving up and down the country every few years for different jobs?' LDFT trainee.
A number of DFT trainees reflected that they would have considered LDFT if offered in more areas.
'Location is quite important to me… it's a bit difficult, now I'm married I'm a bit more tied down…if there wasn't one (LDFT) where I live… even though…it sounds like a really good experience, I probably wouldn't go for it.' DFT trainee, now GDP.
In contrast to this, some trainees were clear that they would prioritise training programme over location.
'I went to university at Leeds so I wanted to stay local to the Yorkshire area but… if I'd got the longitudinal scheme in Newcastle I would have moved for the job.' LDFT trainee.
Personal
Personal circumstances could affect decisions to apply for further training (DCT).
'I probably would have applied to national recruitment for DCT Training but I'm getting married next year so that's kind of also played a role in things…' DFT trainee, now GDP.
'…buying a house, choosing an area to live in, wanting that sort of thing, whereas I think hospital… you have to apply to different areas and you don't necessarily know where you're going to end up…' Supervisor based in primary care.
Other trainees reflected on the work/life balance of senior colleagues when considering whether to pursue further training.
'… she's (dental speciality trainee) already moved a few times, had to move, her husband around.' LDFT trainee.
'I sent my references off and the consultants… one of them had done it that (Saturday) evening, one had done it on a Sunday morning, you just think, you're obviously having to answer emails and stuff at the weekends and is that something that you want to be doing long term?' LDFT trainee.
Discussion
Within this study, DFT was generally viewed as a useful transition period for a newly qualified dental graduate before independent general dental practice. Participants identified DFT as a period of training to consolidate and develop skills within general dentistry, building upon that taught in dental school. Frequently reported reasons to pursue DCT upon completion of DFT were to specialise in the future, to improve surgical skills, to understand secondary care and the management of medically compromised patients. These findings are similar to those from previous studies with 'improvement in oral surgery skills' being the most common reason to undertake an SHO role in OMFS in 2012.15 In 2010, there was over 70% agreement that experience in surgical extractions, management of medically compromised patients and to enter the specialist training pathway were motivational factors to apply for an SHO post.16 However, DCT roles based in OMFS settings was perceived by some to be daunting, with concern around working in a medical environment and concern that the trainee may deskill, having just recently consolidated general dentistry skills within DFT. Peer opinion seemed to influence trainee choice when considering training pathways and therefore may contribute to some of these negative perceptions of DCT within an OMFS setting with lack of medical knowledge, being on-call at night and ward duties found to be the worst aspects of an OMFS SHO post.15 Some participants explained they would prefer to go straight into GDP following DFT to continue to maintain and consolidate their general dentistry skills, alternatively some explained that they would prefer to pursue a more dental specific DCT post and that ideally there should be more DCT posts based in other dental specialties. Therefore, the broad experience of LDFT was appealing to some in that this involved training within different specialties and settings throughout the programme and therefore less risk of de-skilling. It was also felt that this would help inform career decisions by experiencing multiple specialties rather than focusing on only one speciality or setting. However, there were differing opinions as to whether training simultaneously within different settings (LDFT) or being fully immersed within one setting and speciality at a time (DFT+DCT1) would be better. Within a broad-based medical training programme in different specialties, it was identified that trainees could 'struggle to fit in' compared with those on more traditional pathways who gained more of a 'sense of community'.32 Within our study, there was the perception that LDFT trainees may take longer to settle in to a role within multiple settings; however, once settled there were perceived advantages in particular the application of transferrable skills and lack of concern arou,nd deskilling. Finally, the LDFT training pathway was appealing to many in that it offered a two-year period of job security, without the need to apply for a new job or DCT1, 6 months into DFT. The national recruitment process for DCT, did appear to discourage some from applying to DCT1 with concern around potential change in location, with many not liking the idea that they may have to potentially move every 12 months should they opt for DCT after DFT. Generally, there were mixed views regarding whether location or programme was most important when choosing a training pathway, however many reported personal factors they needed to consider such as location, family and finance.
Conclusion
The first part of this two-part series explores current perceptions of different post-qualification dental training pathways and the considerations trainees take into account when deciding on further training. The perceived advantage of the traditional DFT, DFT+DCT1 training pathways has been identified in terms of being immersed within one clinical setting for one year. However, the potential advantage of exploring different dental specialties over a two-year integrated period has been identified in terms of informing career decisions. Peer opinion seems to influence trainee decisions for training and that trainees can be 'put off' traditional OMFS DCT posts due to the medical nature of the role and the working hours. The recruitment process and location of posts appears to influence training pathway choice particularly when this has an impact on personal factors such as finance, family commitments and location. The second part of this paper will explore the themes of skill development, career development, identity and team to understand how well the training pathways prepare trainees for clinical practice and their future careers. A detailed discussion and conclusion will be covered in part 2 to explore recurring themes or differences in the three different training pathways and how this fits with current literature.
References
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). Dental Foundation Training Handbook. 2016. Available online at http://www.copdend.org/DFTHandbook/index.html (accessed 18 August 2018).
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). Dental Foundation Training Curriculum 2015. Available online at http://www.copdend.org//data/files/Foundation/Curriculum%202016%20Printable%20%20reverse%20colourway.pdf (accessed 18 August 2018).
National Health Service Health Education England. Advancing dental care: education and training review. final report. May 2018. Available online at https://www.hee.nhs.uk/sites/default/files/documents/advancing_dental_care_final.pdf (accessed 18 August 2018).
Ralph J P, Mercer P E, Bailey H. A comparison of the experiences of newly qualified dentists and vocational dental practitioners during their first year of general dental practice. Br Dent J 2000; 189: 101-106.
Palmer N O A, Kirton J A, Speechley D. An investigation of the clinical experiences of dentists within the national dental foundation training programme in the North West of England. Br Dent J 2016; 221: 323-328.
Clow R, Mehra S. Evaluation of vocational training of dentists in three different regions. Br Dent J 2006; 201: 774-778.
Cabott L B, Patel H M. Aspects of the dental vocational training experience in the South East of England. Br Dent J 2007; 202: 1-6.
Barlett D W, Coward P Y, Wilson R, Goodsman D, Darby J. Experiences and perceptions of vocational training reported by the 1999 cohort of vocational dental practitioners and their trainers in England and Wales. Br Dent J 2001; 191: 265-270.
McKenna G, Burke F, O'Sullivan K. Attitudes of Irish dental graduates to vocational training. Eur J Dent Educ 2010: 14; 118-123.
Gilmour J, Stewardson D A. Morale of vocational dental practitioners in the United Kingdom. Br Dent J 2008; 204: E18.
Oxley C J, Dennick R, Batchelor P. The standard of newly qualified dental graduates - foundation trainer perceptions. Br Dent J 2017; 222: 391-395.
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). UK Dental Core Training Curriculum. December 2016. Available online at https://www.copdend.org/wp-content/uploads/2018/09/2016-12-14-UK-DCT-Curriculum-December-2016.pdf (accessed 31 October 2019)..
Keith D J W, Durham J. Senior house officer training in oral and maxillofacial surgery: a national survey. Br Dent J 2003; (Suppl) 23-28.
Stancliffe H, Little R, Keith D. An evaluation of senior house officer training in oral and maxillofacial surgery. Br Dent J 2011; 211: 75-80.
Wildan T, Amin J, Bowe D, Gerber B, Saeed N R. Dental foundation year 2 training in oral and maxillofacial surgery units - the trainees' perspective. Br J Oral Maxillofac Surg 2013; 51: e155-e64.
Gallagher J E, Bates T J, Kalsi H, Shah A, Wang Y J, Newton J T. What is the role of senior house officer or dental foundation year two posts within professional careers? Prim Dent Care 2010; 17: 115-122.
Plowman L, Musselbrook K. An evaluation of general professional training for dentistry in Scotland. Br Dent J 2000; 188: 154-159.
Prescott L E, McKinlay P, Rennie J S. The development of an assessment system for dental vocational training and general professional training: a Scottish approach. Br Dent J 2001; 190: 41-44.
Karsondas N, Karsondas N, Blaylock P. The two-year longitudinal dental foundation training programme: an option worth revisiting. Br Dent J 2019; 226: 224-227.
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). A reference guide for dental foundation training in England, Wales and Northern Ireland. The DENTAL BLUE GUIDE. Available online at https://www.copdend.org/wp-content/uploads/2018/03/BlueGuide2016.pdf (accessed February 2019).
UK Foundation Programme Office. UK Foundation Programme. 2003. Available online at http://www.foundationprogramme.nhs.uk/content/about (accessed 19 August 2018).
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). A curriculum for UK dental foundation programme training. 2006. Available online at http://www.copdend.org/data/files/Foundation/Dental%20Foundation%20Programme%20Curriculum.pdf (19 August 2018).
UK Committee of Postgraduate Dental Deans and Directors (COPDEND). Dental Foundation Training Policy Statement. Available online at http://www.copdend.org/content.aspx?Group=foundation&Page=foundation_policystatement (19 August 2018).
Glaser B G, Strauss A L. The discovery of grounded theory: strategies for qualitative research. New York, USA: Aldine de Gruyter, 1967.
Morse J, Richards L. Read me first for a user's guide to qualitative methods. California, USA: SAGE Publications, 2002.
Cresswell J W. Educational research: Planning, conducting and evaluating quantitative and qualitative research. 2nd ed. New Jersey: Pearson Education Inc, 2005.
Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory. 3rd ed. California, USA: SAGE Publications, 2008.
Roller M R, Lavrakas P J. Applied qualitative research design: a total quality framework approach. New York: The Guilford Press, 2015.
Cresswell J W. Research design: Qualitative, quantitative and mixed methods approaches. 3rd ed. California: SAGE Publications Inc, 2009.
Spencer L, Ritchie J, O'Connor W. Analysis: practices, principles and processes. In Ritchie J, Lewis J (eds) Qualitative research practice: a guide for social science students and researchers. pp. 199-218. London: SAGE Publications Ltd, 2003.
Lewis J, Ritchie J. Generalising from Qualitative Research. In Ritchie J, Lewis J (eds) Qualitative research practice a guide for social science students and researchers. pp. 263-286. London: SAGE Publications Inc, 2003.
Bullock A, Webb K L, Muddiman E, McDonald J, Allery L, Pugsley L. Enhancing the quality and safety of care through training generalist doctors: a longitudinal, mixed-methods study of a UK broad-based training programme. BMJ Open 2018; 8: e021388.
Acknowledgements
The authors wish to thank all participants who contributed towards this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was funded by Health Education England.
Rights and permissions
About this article
Cite this article
J. Coleman, A., M. Finn, G. Post-qualification dental training. Part 1: perceptions of different dental foundation and dental core training pathways. Br Dent J 227, 915–921 (2019). https://doi.org/10.1038/s41415-019-0909-z
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0909-z
This article is cited by
-
Dental core training - a five-year review of career intentions and outcomes of trainees working at a large teaching hospital
British Dental Journal (2021)
-
The dental core training experience: the views of trainees and their postgraduate training leads
British Dental Journal (2020)
-
Dental core training: the trainee perspective
British Dental Journal (2020)