Abstract
Introduction There are multiple ways in which treatment using dental implants is provided in a secondary care setting, not only in terms of the groups of patients treated, but also the clinicians who provide that care.
Methods An online survey was circulated to speciality registrars in restorative dentistry in all UK dental hospitals and to postgraduate students in prosthodontics in the Republic of Ireland, consisting of nine questions aimed at understanding which patient groups are treated using dental implants in a hospital setting, how cases are planned, executed and to explore the underlying reasons for each unit's method of provision.
Results Completed surveys were received from 67% of dental hospitals in Britain and Ireland. Treatment planning was undertaken by the restorative team alone in 64% of units in patients with hypodontia, 57% with trauma and 71% with an atrophic edentulous ridge and by a multi-disciplinary team in 50% of units for patients with cleft lip and palate (CLP) and 45% with head and neck (H&N) cancer. The restorative team place all or most of the implant fixtures in 50% of units in patients with CLP, 71% in trauma patients, 71% in hypodontia patients, 64% in edentulous patients and 43% in H&N oncology patients. Stents are produced and used by the restorative team in 64% of units for edentulous patients, 79% of patients with hypodontia, 79% of those suffering trauma, 58% of CLP patients and 50% of patients with H&N cancer. Twenty-one percent of responding units had stents made by the restorative team and used by the surgical team. The median percentage of implant-supported restorations that are screw retained is 90% (SD: 4.93, range: 25-95%) and the median percentage of zirconia abutments being used is 22.5% (SD: 5.24, range: 0-50%). Use of zygomatic implants varies hugely between responding units with 43% of them not placing any zygomatic implants.
Conclusions There is a wide range of protocols and team members involved in the provision of dental implant rehabilitations throughout the British Isles reflecting the lack of any single evidence-based approach. A multi-disciplinary team approach with the restorative dentist as a key member is likely to yield the most favourable long term outcomes.
Similar content being viewed by others
Key points
-
Points out that there is a great variation in the type of cases in which dental implant rehabilitations are performed, how they are planned and how they are executed.
-
Suggests that a multi-clinician, multi-speciality approach is likely to yield the best overall outcome for a complex patient's rehabilitation.
-
Outlines how a treatment plan must always be prosthetically driven using a 'tooth-down' approach and therefore the restorative dentist should have a central role.
Introduction
The use of dental implants to rehabilitate patients in a secondary/tertiary care setting is increasing, therefore it would seem logical to assume that the range of clinicians performing these procedures is also increasing.1,2 Such high volumes of treatment are likely to result in greater variability in how patients are planned and the procedures executed.
The most recent guidelines from the Royal College of Surgeons (RCS) recommends considering the use of dental implants for the management of congenital conditions (such as hypodontia, cleft lip and palate (CLP), ectopic teeth and malformed teeth such as in amelogenesis imperfecta/dentinogenesis imperfecta and dens invaginatus), traumatic loss of teeth, ablative surgery for head and neck (H&N) cancer (both intra oral and extra oral uses), for edentulous patients, those with denture intolerance (to stabilise a tolerated cut back horseshoe denture), aggressive periodontitis (once stabilised) and in the management of a malocclusion (for anchorage).3 As with any clinical guideline, uptake and implementation practices can vary significantly across different centres, therefore this warrants further investigation.
It is known that dental implants can be successfully used to rehabilitate missing single teeth,4 partially dentate patients5 and total edentulism.6,7,8 There is also a substantial body of evidence to support the use of dental implants to rehabilitate patients in the specific situations listed by the RCS above.
In patients with hypodontia, Bouchard et al.9 demonstrated that implant-supported prostheses are more successful and cost effective long term compared to conventional tooth supported prosthodontics. Similarly, Yap and Klineberg10 found high quality literature to be scarce but did report implant survival rates of 88.5-97.6% in patients with ectodermal dysplasia and 90-100% in patients with tooth agenesis. The use of implants to support obturators in the rehabilitation of patients with CLP has also been reported.11
Schwartz-Arad and Levin's retrospective case series on the use of dental implants to rehabilitate anterior maxillary teeth which had been lost due to trauma showed a high need for grafting procedures, a higher than average complication rate but an average survival rate.12 The use of dental implants to rehabilitate patients who have had treatment of a neoplasm of the H&N has been shown repeatedly13 and are invaluable in the management of a patient with extensive loss of the facial tissues offering significant benefits above tooth or mucosa borne prostheses.14,15,16
There are extensive reports of implants being used to rehabilitate edentulous patients with either fixed17,18 or removable19,20 treatment options. Patients are usually highly satisfied with the use of implants to retain complete mandibular overdentures and have a significant improvement in their oral health-related quality of life21,22,23,24 with such treatment shown to be cost effective.25 It is for these reasons that both the McGill26 and York27 Consensuses recommend the two implant mandibular overdenture as the standard treatment for all edentulous mandibles.
Given the evidence and guidance supp
orting the use of dental implants in the management of such patient groups, this cross-sectional study aims to assess the current provision and workflow of dental implant patients in dental hospitals in the UK and Ireland.
Methods
To fulfil the stated aim of this study, a cross sectional design was employed. The Senior Clinical Trials Coordinator of Clinical and Scientific Services of Manchester Universities NHS Foundation Trust deemed this project a service review and therefore exempt from ethical approval. Consent to the service review was given by the restorative department lead and Hospital Clinical Director.
A nine-question survey (see Appendix S1, in the online supplementary information) was created using online survey software (SurveyMonkey). The questions were designed to provide an overview of current practice in planning and execution of implant reconstructions in different units and which teams were involved at which stages. Questions were included regarding the use of screw- or cement-retained restorations and titanium or zirconia abutment materials. Such questions were also surrogates for assessing the use of restorative techniques for managing sub-optimally positioned fixtures, as it would generally be considered preferable to use screw-retained superstructures wherever possible. A free text comment section asking for the respondents' reasoning was made available for these questions to ensure that the figure given wasn't due to personal preference.
The composition of the survey was developed in discussion between the authors and the questions were considered factual and self-explanatory. As this was a service review, pilot testing was not deemed necessary.
The survey was distributed to Speciality Registrars in restorative dentistry via the mailing list of the Speciality Registrars in Restorative Dentistry Group (SRRDG). After the initial invitation to participate a reminder email was sent two weeks later to improve the response rate. An attempt to contact non-responding units was made by direct contact with members of that unit known to the authors.
Statistical analysis was used for descriptive purposes only.
Results
Responses were received from twelve dental hospitals. The response rate overall was 67% (12 of 18) and for each country individually was: England: 100% (10 of 10), Wales 100% (1 of 1), Scotland 0% (0 of 4), Northern Ireland 0% (0 of 1) and Republic of Ireland 50% (1 of 2).
With regards to the planning of implant rehabilitations (Table 1) the majority of patients diagnosed with hypodontia, trauma or an atrophic edentulous ridge, 64%, 57% and 71% respectively, are planned by the restorative team alone. Half of patients with a CLP are treatment planned by a joint multi-disciplinary team (MDT) with at least restorative and surgical input. Finally, patients being rehabilitated from H&N with dental implants are primarily treatment planned by an MDT (45%) but a significant portion are also planned by the restorative team alone (36%). Some respondents commented that the orthodontic team are also involved in the management of hypodontia patients and that the team members involved depends heavily on the complexity of the case and the need for specific procedures, bone grafting requiring surgical input for example.
A range of team members place fixtures in all patient groups studied (Table 2). H&N patients' implants are placed either entirely or mostly by the restorative team in 43% of respondents' units but 29% are entirely or mostly placed by the surgical team. The restorative team place all or most of the fixtures in patients with CLP (50%), trauma (71%), hypodontia (71%) and edentulism (64%). Additional comments generally stated that responses to this question were an estimate made by the responder and not based on exact figures.
The use of surgical stents varies (Table 3), in the majority of responding units stents are produced by the restorative team and used by them intraoperatively for edentulous patients, those with hypodontia, those suffering trauma and CLP, 64%, 79%, 79% and 58% respectively. The same, however, can only be said for half of patients with H&N cancer, with 21% of responding units having stents made by the restorative team and used by the surgical team, which likely reflects more fixtures being placed by the surgical team in this patient group. Interestingly, one responding unit reported that stents are made by the restorative team but not used by the surgical team for all patient groups except H&N cancer patients in whom they are sometimes used by the surgical team. Some comments indicated that the use of stents depends upon the complexity of the case and that there isn't always time for the planning and construction of a stent.
Of the responding units, the median percentage of implant-supported restorations that are screw retained is 90% (SD: 4.93, range: 25-95%). Reasons given for this high proportion of screw-retained restorations are: retrievability; ease of maintenance; availability of angled screw access systems and reduced risk of excess cement and therefore peri-implant disease. Some of the reasons given for use of cement-retained restorations includes: personal preference and positioning of the fixture due to intraoperative error or bone availability. When considering the abutment material, the median percentage of zirconia abutments being used at responding units is 22.5% (SD: 5.24, range: 0-50%).
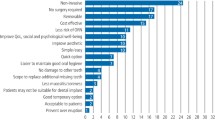
Use of zygomatic implants varies between responding units (Fig. 1) with 43% of them not placing any zygomatic implants and no units placing zygomatic implants in patients with hypodontia. Of those units placing zygomatic implants 13% are placing them in patients with trauma, 25% in patients with CLP, 63% in edentulous patients and 88% as part of rehabilitations of patients with H&N cancer.
Respondents were invited to give any general comments on how implant reconstructions were provided in their units and an emerging theme was a lack of collaboration between the restorative and surgical teams resulting in challenging restorative situations and compromised outcomes. There was a feeling that at some responding units the restorative and surgical teams work in their own silos, only work together on complex cases and more team-working through an MDT structure would yield benefits for the patient pathway.
Discussion
The results of this survey showed that planning of dental-implant-supported rehabilitations is undertaken by a range of clinicians both alone and as part of an MDT. Literature on who plans implant rehabilitations is scarce. Burns et al.28 reported that 72% of their cohort of patients with hypodontia who had been rehabilitated with dental implants had had an MDT approach to planning and this approach has been recommended by others both for hypodontia29 and for planning of complex cases in general.30
There may be many different team members undertaking the surgical placement of the implant fixtures and this survey's responses show a wide variety. Previous surveys enquiring on this area have also reported a range of different clinicians undertaking placements. Butterworth et al.31 reported 89% of responding consultant restorative dentists worked with a surgeon who placed implants for them but 35% of these also placed their own implants in some cases, and 11% placed all their own implants. Specifically for H&N cancer patients, Calvert et al.32 reported fixture placements were by restorative dentistry consultants in 39% of responders, by oral and maxillofacial surgeons in 38% of responders, by oral surgeons in 17% of responders and 3% by others. Dewan et al.33 showed that either the restorative dentist (10%) or surgeon (30%) or both (60%) placed dental implants in H&N cancer patients and Alani et al.1 reported the placement of implants for rehabilitation of following H&N cancer treatment was most commonly performed by the oral and maxillofacial surgeon (70%) or the restorative dentist (16%); however, in 24% of responses the decision depended on the type of case.
The use of surgical stents is a contentious issue with some clinicians finding them invaluable and some preferring to place their fixtures freehand. Stents may be produced via an analogue technique using waxed up casts and vacuum-formed stents34 or via a digital pathway using computed tomography and 3-dimensional printing.35 There is an absence of consensus on the optimal technique and very limited data on what is currently being done. It would generally be agreed that more complex clinical situations make the use of some sort of guide essential and so it is unsurprising that Dewan et al.33 reported 81% of their respondents used computed tomography-based technology for planning and placement.
The decision of whether to cement or screw retain restorations has been debated for almost as long as dental implants have been available. While neither approach could be universally advocated, a key determinant of the ability to screw retain a prosthesis is the angulation of the fixture.36,37 No data could be identified in the previous literature as to the proportions of restorations that are screw or cement retained; however, in this survey results there was a definite trend towards screw retention being preferred but a wide range was observed.
Zygomatic implants have been utilised successfully for many years38 and are an alternative to bone augmentation procedures in the atrophic maxilla.39 The availability of zygomatic fixtures greatly increases options for rehabilitation in patients who have had a maxillectomy.40,41 Our survey found varying degrees of use of zygomatic implants among respondents with the majority of units who place them doing so for CLP and H&N cancer patients. Calvert et al.32 found 12.9% of their responding consultant restorative dentists placed zygomatic implants and Alani et al.1 found 29% of oral and maxillofacial surgeons did. These figures aren't directly comparable to our results as they were individual to the consultant rather than asking about the unit as a whole.
Conclusions
Based on the self-reported situations at the responding units throughout the British Isles it is clear that there is great variety in the patients for whom dental implant rehabilitations are performed, how they are planned and how they are executed. This variety likely reflects the lack of high quality evidence to recommend any single protocol and the historic set up within individual units as to which team undertake which tasks.
Many of the patients groups for whom dental implant rehabilitations are provided pose complex clinical problems and may already be under the care of an MDT. This multi-clinician, multi-speciality care is likely to yield the best overall outcome for a patient's rehabilitation; however as such a plan must always be prosthetically driven using a 'tooth- down' approach then one could argue that the restorative dentist should have a central role in the provision of care for such patients.
References
Alani A, Owens J, Dewan K, Summerwill A. A national survey of oral and maxillofacial surgeons' attitudes towards the treatment and dental rehabilitation of oral cancer patients. Br Dent J 2009; 207: E21; discussion 540-541.
Ali A, Fardy M J, Patton D W. Maxillectomyto reconstruct or obturate? Results of a UK survey of oral and maxillofacial surgeons. Br J Oral Maxillofac Surg 1995; 33: 207-210.
Alani A, Bishop K, Renton T, Djemal S. Update on guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHSthe position after 15 years. Br Dent J 2014; 217: 189-190.
Schmitt A, Zarb G A. The longitudinal clinical effectiveness of osseointegrated dental implants for single-tooth replacement. Int J Prosthodont 1993; 6: 197-202.
Lindh T, Gunne J, Tillberg A, Molin M. A meta-analysis of implants in partial edentulism. Clin Oral Implants Res 1998; 9: 80-90.
Chan M F, Howell R A, Cawood J I. Prosthetic rehabilitation of the atrophic maxilla using pre-implant surgery and endosseous implants. Br Dent J 1996; 181: 51-58.
Chan M F, Johnston C, Howell R A, Cawood J I. Prosthetic management of the atrophic mandible using endosseous implants and overdentures: a six year review. Br Dent J 1995; 179: 329-337.
Zarb G A, Schmitt A. Osseointegration and the edentulous predicament. The 10yearold Toronto study. Br Dent J 1991; 170: 439-444.
Bouchard P, Renouard F, Bourgeois D, Fromentin O, Jeanneret M H, Beresniak A. Cost-effectiveness modeling of dental implant vs. bridge. Clin Oral Implants Res 2009; 20: 583-587.
Yap A K, Klineberg I. Dental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literature. Int J Prosthodont 2009; 22: 268-276.
Arcuri M R, LaVelle W E, Higuchi K W, Svec B R. Implant-supported prostheses for treatment of adults with cleft palate. J Prosthet Dent 1994; 71: 375-378.
Schwartz-Arad D, Levin L. Post-traumatic use of dental implants to rehabilitate anterior maxillary teeth. Dent Traumatol 2004; 20: 344-347.
Marx R E, Morales M J. The use of implants in the reconstruction of oral cancer patients. Dent Clin North Am 1998; 42: 177-202.
Franzen L, Rosenquist J B, Rosenquist K I, Gustafsson I. Oral implant rehabilitation of patients with oral malignancies treated with radiotherapy and surgery without adjunctive hyperbaric oxygen. Int J Oral Maxillofac Implants 1995; 10: 183-187.
Parel S M, Branemark P I, Jansson T. Osseointegration in maxillofacial prosthetics. Part I: Intraoral applications. J Prosthet Dent 1986; 55: 490-494.
Weischer T, Schettler D, Mohr C. Concept of surgical and implant-supported prostheses in the rehabilitation of patients with oral cancer. Int J Oral Maxillofac Implants 1996; 11: 775-781.
Adell R, Eriksson B, Lekholm U, Branemark P I, Jemt T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants 1990; 5: 347-359.
Arvidson K, Bystedt H, Frykholm A, von Konow L, Lothigius E. A 3year clinical study of Astra dental implants in the treatment of edentulous mandibles. Int J Oral Maxillofac Implants 1992; 7: 321-329.
Jemt T, Chai J, Harnett J et al. A 5year prospective multicentre follow-up report on overdentures supported by osseointegrated implants. Int J Oral Maxillofac Implants 1996; 11: 291-298.
Mericske-Stern R, Zarb G A. Overdentures: an alternative implant methodology for edentulous patients. Int J Prosthodont 1993; 6: 203-208.
Awad M A, Lund J P, Shapiro S H et al. Oral health status and treatment satisfaction with mandibular implant overdentures and conventional dentures: a randomized clinical trial in a senior population. Int J Prosthodont 2003; 16: 390-396.
Cune M S, de Putter C, Hoogstraten J. Treatment outcome with implant-retained overdentures: Part IIPatient satisfaction and predictability of subjective treatment outcome. J Prosthet Dent 1994; 72: 152-158.
Emami E, Heydecke G, Rompre P H, de Grandmont P, Feine J S. Impact of implant support for mandibular dentures on satisfaction, oral and general health-related quality of life: a meta-analysis of randomized-controlled trials. Clin Oral Implants Res 2009; 20: 533-544.
Hobkirk J A, Abdel-Latif H H, Howlett J, Welfare R, Moles D R. Prosthetic treatment time and satisfaction of edentulous patients treated with conventional or implant-stabilized complete mandibular dentures: a case-control study (part 2). Int J Prosthodont 2009; 22: 13-19.
Heydecke G, Penrod J R, Takanashi Y, Lund J P, Feine J S, Thomason J M. Cost-effectiveness of mandibular two-implant overdentures and conventional dentures in the edentulous elderly. J Dent Res 2005; 84: 794-799.
Feine J S, Carlsson G E, Awad M A et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25: 2002. Int J Oral Maxillofac Implants 2002; 17: 601-602.
Thomason J M, Feine J, Exley C et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patientsthe York Consensus Statement. Br Dent J 2009; 207: 185-186.
Burns B, Grieg V, Bissell V, Savarrio L. A review of implant provision for hypodontia patients within a Scottish referral centre. Br Dent J 2017; 223: 96-99.
Bergendal B, Bergendal T, Hallonsten A L, Koch G, Kurol J, Kvint S. A multidisciplinary approach to oral rehabilitation with osseointegrated implants in children and adolescents with multiple aplasia. Eur J Orthod 1996; 18: 119-129.
Epstein NE. Multidisciplinary in-hospital teams improve patient outcomes: A review. Surg Neurol Int 2014; 5(Suppl 7): S295-303.
Butterworth C J, Baxter A M, Shaw M J, Bradnock G. The provision of dental implants in the National Health Service Hospital dental servicesa national questionnaire. Br Dent J 2001; 190: 93-96.
Calvert G, Barclay S C, Owens J S, Alani A. A national survey of restorative consultants' treatment provision for head and neck oncology patients. Br Dent J 2014; 217: E21.
Dewan K, Kelly R D, Bardsley P. A national survey of consultants, specialists and specialist registrars in restorative dentistry for the assessment and treatment planning of oral cancer patients. Br Dent J 2014; 216: E27.
Becker C M, Kaiser D A. Surgical guide for dental implant placement. J Prosthet Dent 2000; 83: 248-251.
Flugge T V, Nelson K, Schmelzeisen R, Metzger M C. Three-dimensional plotting and printing of an implant drilling guide: simplifying guided implant surgery. J Oral Maxillofac Surg 2013; 71: 1340-1346.
Hebel K S, Gajjar R C. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent 1997; 77: 28-35.
Michalakis K X, Hirayama H, Garefis P D. Cement-retained versus screw-retained implant restorations: a critical review. Int J Oral Maxillofac Implants 2003; 18: 719-728.
Brånemark P. Surgery and fixture installation. Zygomaticus Fixture Clinical Procedures Göteborg, Sweden: Nobel Biocare. 1998.
Pi Urgell J, Revilla Gutierrez V, Gay Escoda C G. Rehabilitation of atrophic maxilla: a review of 101 zygomatic implants. Med Oral Patol Oral Cir Bucal 2008; 13: E363-370.
Tamura H, Sasaki K, Watahiki R. Primary insertion of implants in the zygomatic bone following subtotal maxillectomy. Bull Tokyo Dent Coll 2000; 41: 21-24.
Weischer T, Mohr C. Ten-year experience in oral implant rehabilitation of cancer patients: treatment concept and proposed criteria for success. Int J Oral Maxillofac Implants 1999; 14: 521-528.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
James, M., Taylor, C. A cross sectional study of dental implant service provision in British and Irish dental hospitals. Br Dent J 227, 735–739 (2019). https://doi.org/10.1038/s41415-019-0859-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0859-5