Abstract
The objective of this clinical case study is to illustrate the caries management four-step structured process, leading to personalised interventions specific for each individual patient's risks and needs, according to CariesCare International, derived from the International Caries Classification and Management System (ICCMS) for clinical practice. An 18-year-old female was diagnosed with higher caries risk at the individual level, and with several caries lesions at different severity stages, some likely active and others likely inactive. A care plan was co-created with the patient and delivered to obtain optimal health outcomes. Several issues pertinent to patient-centred care are discussed, including caries management at the individual and the tooth surface level, the preservation of tooth structure, patient's caries risk management, and prevention and control of caries lesions. The patient's perspective is taken into account and the health outcome focus of the system is highlighted.
Similar content being viewed by others
Key points
-
Provides an example for dentists to help them deliver optimal caries care and outcomes for their patients with the CariesCare International 4D-cycle as a practice-building format.
-
Demonstrates how the system can prevent and control caries.
-
Shows an example of how the system can engage patients as long term health partners with their practice.
Introduction
CariesCare International (CCI™) is a charity promoting a patient-centred, risk-based approach to caries management designed for dental practice.1 This comprises a health outcomes-focused system that aims to maintain oral health and preserve tooth structure in the long-term by sharing the same goals as the International Caries Classification and Management System (ICCMS).2,3,4,5
The CariesCare International guide takes the dental team through a four-step structured process (Fig. 1), leading to personalised interventions specific for each individual patient's risks and needs. The four interlinked steps in the cycle (4D's) are: 1st D: Determine caries-risk; 2nd D: Detect lesions, stage their severity and assess their activity status; 3rd D: Decide on the most appropriate care plan for the specific patient at that time; and then 4th D: Do the preventive and tooth-preserving care which is needed (including risk-appropriate preventive care; control of initial non-cavitated lesions; and conservative restorative treatment of deep dentinal and cavitated caries lesions). Full details of the consensus guide are available in the first BDJ article in this series.1
Case report
An 18-year-old female patient presented complaining of sensitivity in a molar tooth at the level of the lower right quadrant when eating sugar. These signs and symptoms had been present intermittently for the previous three months.
1st D: DETERMINE: Caries risk
At the caries risk assessment, after gathering information from interview and clinical assessment with the patient, each of the caries protective factors which were failing and caries risk factors present that she presented with were clearly explained to her (Fig. 2).
2nd D: DETECT & ASSESS: Caries staging and activity
At the detection and staging of caries lesions and assessment of activity, the patient was shown the following findings from the visual and radiographic assessments:
ICDAS-merged radiographic caries stages
The patient showed on the bitewing x-rays initial enamel radiolucency (IER), initial dentine radiolucency (IDR), and moderate radiolucency (MR) in her posterior teeth (Fig. 3).
ICDAS-merged visual coronal caries stages and activity status
In the visual exam the patient presented initial, moderate and extensive lesions, some active and some inactive, caries lesions. The patient also showed a moderate dental fluorosis (according to TFI) and calculus in M of first upper molars.2
3rd D: DECIDE: Personalised care plan; patient and tooth levels
At the patient level, after analysing caries protective and risk factors from the '1st D', with the aid of the patient's caries risk level flowchart, her caries risk level was classified as 'At higher risk', due to the presence of a red-marked risk factor (presence of active caries lesions) and in addition a combination of other risk factors (high-amount/frequency free sugars intake, poor oral hygiene and access barriers) and protective factors failing (previous lack of dental care). At the tooth level, after analysing information from the '2nd D', and with the aid of the coronal caries diagnosis flowchart combining visual and radiographic caries severity stage with lesion activity (Fig. 4), the patient presented as: 'likely active: 2 extensive, 2 moderate (1 underlying dentinal shadow, 1 enamel breakdown/microcavity), 4 initial, and as likely inactive: 3 moderate and 15 initial caries lesions'. A shared personalised plan of care was discussed with her, focusing on identifying the elements and making them explicit (Fig. 5).
4th D: DO: Appropriate tooth-preserving and patient-level prevention and control
The personalised comprehensive caries care plan (Fig. 6) was built with the patient on the outcomes of the first three Ds and was further delivered by the dentist with the contribution of the dental hygienist. The management of the patient's higher caries risk was tailored at the individual level, with actions to improve the risk status taking into account the patient's needs, opportunities and preferences. Emphasis was given to the use of topical fluoride (toothpaste and varnish application), informative and one-to-one dietary advice focusing on free sugars, and toothbrushing. The management of the individual caries lesions was conducted according to their severity and activity. Extensive likely active caries lesions received tooth-preserving operative care (composite restorations), while moderate and initial likely active caries lesions located in the fossae/fissure system were sealed and those in free smooth surfaces received fluoride varnish application plus instructions on localised mechanical biofilm removal. It was decided to seal moderate likely inactive caries lesions and initial likely inactive lesions were assigned active monitoring and reassessment. The patient is now keen on maintaining dental visits every three months.
Discussion and summary
By using this patient-centred CariesCare systematic approach and being guided through a comprehensive 4D-cycle of caries management in practice, the dentist perceived that she was able to deliver optimal caries care and achieve positive health outcomes for the patient through preventing and controlling caries and engaging the patient as a health partner with her practice. The patient perceived that the process was not mechanistic and that her needs, opportunities and preferences were being taken into account during the process. She now understood her personal higher level of caries risk and recognised, with the help of the practitioner, that she had a series of active and inactive caries lesions at various severity stages. Taken together, these realisations helped both the patient and the practitioner to identify ways of modifying behaviours to control the disease process and to create together a shared, personalised, plan of care. During the process, it became clear that the patient now wants to avoid fillings whenever possible.
References
Martignon S, Pitts N B, Goffin G et al. CariesCare practice guide: consensus on evidence into practice. Br Dent J 2019; 227: 353-362.
Pitts N B, Ekstrand K R, ICDAS Foundation. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS) - methods for staging of the caries process and enabling dentists to manage caries. Community Dent Oral Epidemiol 2013; 41: e41-e52.
Pitts N B, Ismail A I, Martignon S, Ekstrand K, Douglas G V A, Longbottom C. ICCMS™ Guide for Practitioners and Educators. 2014. Available at: http://doi.org/10.5281/zenodo.853106 (accessed May 2019).
Ismail A I, Pitts N B, Tellez M et al. The International Caries Classification and Management System (ICCMS) An Example of a Caries Management Pathway. BMC Oral Health 2015; 15 (Spec Iss): S9.
International Caries Classification and Management System (ICCMS™). Available at https://www.iccms-web.com/ (accessed May 2019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beltrán, E., Guiu, L., Zarta, O. et al. Caries classification and management in the context of the CariesCare International (CCI™) consensus: a clinical case study. Br Dent J 227, 363–366 (2019). https://doi.org/10.1038/s41415-019-0680-1
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0680-1
This article is cited by
-
Knowledge of undergraduate dental students regarding management of caries lesions
BDJ Open (2022)
-
New UK Chapter of the Alliance for a Cavity-Free Future
British Dental Journal (2021)
-
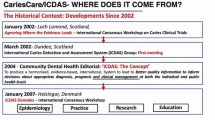
From 'ICDAS' to 'CariesCare International': the 20-year journey building international consensus to take caries evidence into clinical practice
British Dental Journal (2021)
-
Caries and collaborations in context
British Dental Journal (2021)
-
When least is most
British Dental Journal (2019)