Abstract
This CariesCare practice guide is derived from the International Caries Classification and Management System (ICCMS) and provides a structured update for dentists to help them deliver optimal caries care and outcomes for their patients. This '4D cycle' is a practice-building format, which both prevents and controls caries and can engage patients as long-term health partners with their practice. CariesCare International (CCI™) promotes a patient-centred, risk-based approach to caries management designed for dental practice. This comprises a health outcomes-focused system that aims to maintain oral health and preserve tooth structure in the long-term. It guides the dental team through a four-step process (4D system), leading to personalised interventions: 1st D: Determine Caries Risk; 2nd D: Detect lesions, stage their severity and assess their activity status; 3rd D: Decide on the most appropriate care plan for the specific patient at that time; and then, finally, 4th D: Do the preventive and tooth-preserving care which is needed (including risk-appropriate preventive care; control of initial non-cavitated lesions; and conservative restorative treatment of deep dentinal and cavitated caries lesions). CariesCare International has designed this practice-friendly consensus guide to summarise best practice as informed by the best available evidence. Following the guide should also increase patient satisfaction, involvement, wellbeing and value, by being less invasive and more health-focused. For the dentist it should also provide benefits at the professional and practice levels including improved medico-legal protection.
Similar content being viewed by others
Key points
-
Provides a structured update for dentists to help them deliver optimal caries care and outcomes for their patients.
-
Suggests this 4D cycle is a practice-building format which both prevents and controls caries.
-
Proposes that CariesCare International can engage patients as long term health partners with their practice.
Introduction
What is CariesCare International (CCI™)?
CariesCare International is a charity promoting a patient-centred, risk-based approach to caries management designed for dental practice. This comprises a health outcomes-focused system that aims to maintain oral health and preserve tooth structure in the long-term.
What does CariesCare International aim to do?
It shares the same goals as the International Caries Classification and Management System (ICCMS),1,2,3,4 which are to:
Prevent new caries lesions from appearing
Prevent existing caries lesions from advancing further
Preserve tooth structure with non-operative care at more initial stages and conservative operative care at more extensive caries stages
Manage caries risk factors
Be alert to changes at both the tooth and patient levels through periodic monitoring and review
Improve health outcomes for patients.
Where does the CariesCare practice guide come from?
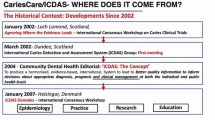
The CariesCare practice guide is derived from ICCMS, which was developed through consensus with international experts by the ICDAS Foundation charity. This journey was started in 2002, with the founding of ICDAS an international group of cariologists who, working with a wide range of other parties along the way, have systematically involved a large number of international experts in a number of high-quality, international, peer-reviewed activities.
The CariesCare practice guide is based upon best available evidence and expert opinion, and it has been specifically tailored for use in dental practice. The guide has been developed through current consensus from experts as a simpler and shorter version of the full ICCMS guide, which was itself developed using consensus agreement based on quality-ranked evidence. Methods of defining consensus vary. In these cases, large numbers of acknowledged experts in the field from many different countries have together considered systematic reviews and research evidence and agreed the final text which they viewed as best practice for the clinical care of patients in a primary care setting.
Who is the CariesCare practice guide for?
It is designed to help dentists and healthcare teams help patients of all ages to control the caries process and maintain health.
How can the CariesCare practice guide be used?
It guides the dental team through a four-step structured process, leading to personalised interventions specific for each individual patient's risks and needs. The four interlinked steps in the cycle (Figure 1) all start with 'D': 1st D: Determine caries-risk; 2nd D: Detect lesions, stage their severity and assess their activity status; 3rd D: Decide on the most appropriate care plan for the specific patient at that time; and then 4th D: Do the preventive and tooth-preserving care which is needed (including risk-appropriate preventive care; control of initial non-cavitated lesions; and conservative restorative treatment of deep dentinal and cavitated caries lesions). These are referred to in CariesCare International as the four Ds.
Why this guide and why this approach?
Multiple sources for evidence-based dentistry exist, however it can be confusing for clinicians to collect, critically analyse and implement all the relevant information into daily practice. CariesCare International has designed this practice-friendly consensus guide to summarise best practice as informed by the best available evidence. It has the objective of putting the patient's health at the centre of a risk-based personalised care plan. It will also help with international trends in practice that 'puts the mouth back in the body' and links oral health to general health. For example, routinely determining and then addressing excessive sugar consumption in dental practice may not only impact on oral health positively but also on disorders with the same risk factors such as obesity and diabetes. Following the guide should also increase patient satisfaction, involvement, wellbeing and value by being less invasive and more health-focused. For the dentist, it should also provide benefits at the professional and practice levels including improved medico-legal protection. Further references can be found at the end of this document for readers that may wish to consult the bibliography selected by the CariesCare International experts.
1st D: DETERMINE Caries Risk
The patient perspective
Understanding their personal level of risk of disease is a key determinant of a patient's motivation to engage with health care and modify their own behaviour to enhance their oral health. Patients who perceive that they are susceptible to a disease are more likely to take action to ameliorate the impact of that susceptibility.
What it is
Caries risk assessment is the first essential step in the 4D-cycle for effective and personalised care. The aim of this step is to assess the probability of whether a patient will develop carious lesions in the near future, and the likelihood that there will be a progression of lesions if already present. Caries risk assessment also helps the dental team understand why the patient has disease activity and consequently informs on adjustments that might be made to improve their risk status. Knowing a patient's caries risk will aid clinical decision-making and enable a personalised caries management plan to be developed.
How to assess the patient's caries risk
Lots of tools already exist which help clinicians to systematically assess caries risk. Common tools are Cariogram, ADA, CAMBRA and ICCMS; many of these use three or more categories of caries risk. However, in practice, it is probably quicker, easier and sufficient to focus on correctly identifying patients at the extremes of the spectrum of risk because those at 'low risk' of caries and those at 'high risk' of caries have clear management needs. Therefore, the CariesCare practice guide uses just two risk categories: 'at lower risk' and 'at higher risk', when choosing between caries management options.
Risk factors and protective factors
A patient's risk level is derived from social, medical, behavioural (oral hygiene, diet etc) and past dental histories, together with an oral examination. The clinician must weigh up the patient's risk and protective factors against each other in order to assess the likely risk of future caries. Low risk is easy to identify as the absence of both caries risk factors and active lesions. The most important information to consider is set out in Figure 2.
Good practice points
-
Patients' caries risk must be assessed regularly, since their risk category may change over time and should be documented in their health record
-
Risk assessment should inform the frequency of patient recall. Patients with higher caries risk should have a shorter recall period than patients at lower risk, for monitoring, re-evaluation, and provision of preventive interventions
-
The risk level should be clearly communicated to the patient and influence clinical decision-making regarding treatment needs and alternatives, as well as the provision of other services
-
Whichever of the many risk assessment tools available is used, it should be integrated into the oral health record and, if possible, into a digital record system
-
Sugar is an important risk factor for caries initiation and progression but it is also a common risk factor for obesity, diabetes and cardiovascular disease. Reducing sugar consumption is therefore important for both oral and general health.
Guidance references:1,2,3,4,5,6,7,8,12,13,14,15,16,17,18,19, 20,21
2nd D: DETECT AND ASSESS: Caries staging and activity
The patient perspective
Assessment is the foundation of all care planning. Practitioner and patient can work together to create a shared understanding of the patient's current health status and their priorities. Conceiving of caries severity as a series of stages helps to identify the importance of both patient and practitioner behaviours in modifying the disease process.
What it is
Caries staging and activity assessment is the second essential step in the 4D-cycle for effective and personalised care. It builds on the knowledge acquired from the 1st D. The aim is to examine the patient carefully for caries lesions, combining this clinical assessment with information from radiographs, when available. This step will involve differentiating caries lesions from other pathologies/conditions such as erosive tooth wear and developmental defects, as well as noting the stage of any caries present (initial, moderate or extensive) and the activity of lesions (likely active or likely inactive). Additionally, this step considers the patient's past caries experience (including number of restorations, state of previous restorative work, teeth extracted due to caries, and dental sepsis). Caries staging and activity assessment also helps clinical decision-making and enables the development of an individualised caries management plan.
How to conduct the caries staging and activity assessment
The caries assessment is based on a visual examination of clean teeth in combination with, where possible, a radiographic examination of posterior teeth (bite-wing x-rays). It is worth remembering that detecting smaller initial stage caries lesions may be more difficult as they develop in areas of plaque stagnation; thus removing plaque is essential (Tables 1, 2, 3, 4).
Stage the severity of caries lesions. These categories based upon surface characteristics of the lesion seen clinically are linked to the histological depth of the lesion
Where there are radiographs, the radiographic depth of a lesion is combined with its clinical appearance to determine the stage of caries
Once the severity stage of a caries lesion has been determined, its activity is assessed.
Coronal caries
Severity staging
Three key visual caries stages can be discriminated to help inform non-operative/operative care decisions.
Visual combined with radiographic
Radiographically, ICDAS classifies coronal caries into three key caries stages (initial, moderate and extensive). That, in combination with the visual staging, help to inform non-operative/operative care decisions.
Caries associated to restoration or sealant (CARS)
The same stages as coronal primary caries apply, but the caries lesion is located in association to a restoration or a sealant. Differentiation should be made from the status of the restoration or sealant: good margin; defective (plaque-retentive, can be adapted); defective (needs replacement).
Activity status
For each coronal caries lesion, assess the activity status using clinical parameters to inform either likely active or likely inactive.
Root caries
Severity staging
Characterised by colour change (light/dark brown or black). Three key root caries stages can be discriminated that will help inform the non-operative/operative care decision.
Activity status
For each root caries lesion, assess the activity status using clinical parameters to inform either likely active or likely inactive. If the lesion is located ≥1 mm from the gingival margin, hard to gentle probing, no cavitation or the surroundings of the cavity, smooth to probing, and dark brown/black, it represents a likely inactive root caries lesion. Conversely, if the lesion is located ≤1 mm from the gingival margin, leathery/soft to gentle probing, cavitation, and light brown/yellowish, it represents a likely active root caries lesion. Together, the caries severity stage along with the activity likelihood of each lesion and the patient's caries risk-status directs care.
Good practice points
-
Clinical caries severity staging is fast and easy after training, which is available through the ICDAS/ICCMS webpage
-
Sharp probing does not improve detection and it causes further damage to caries lesions
-
Clinical caries severity staging does not require any specific device
-
Remember that the radiographic images on bite-wing projections show a range of sizes of approximal lesions but are not able to reveal many occlusal lesions until they are quite extensive
-
The caries staging and activity assessment should be integrated into the oral health record and, if possible, into a digital record system.
Guidance references: ,2,3,4,5,6,7,8,9,10,22,23,24,25,26,27, 28,29,30,31,32,33,34,35,36
3rd D: DECIDE: Personalised care plan: Patient and tooth levels
The patient perspective
A core component of patient-centred care is the discussion of a shared personalised plan of care. The 'DECIDE' stage focuses on identifying that plan and making it explicit. The co-creation of a care plan with the patient enhances the patient's understanding and commitment to the plan.
What it is
Decide: the personalised care plan, at the patient and the tooth levels, is the third essential step in the 4D-cycle for effective and personalised care. The aim of this step is to synthesise all of the information gathered about the patient's caries risk (1st D) and any caries lesions (severity and activity) (2nd D) to develop an informed, risk-based, tooth-preserving care plan. This step is very important because:
It determines, at the tooth-level, what type of treatment to provide; preventive versus surgical
It helps to maintain good oral health and avoid unnecessary removal of tooth tissue
It helps allocate resources appropriately, based on risk
It involves the patient's active engagement on the importance of oral health, avoiding future caries and operative treatment
It helps clinicians to determine the recall interval for the patient.
How to develop the personalised care plan
This step involves discussion with the patient as well as synthesis and consolidation of all the information gathered about the patient's history and clinical findings, as described in this guide. There are practical synthesis guides in relation to caries lesions' stage and activity likelihood, as well as patients' risk classification (for example, ICCMS guideline and webpage). Decision trees will help to determine the personalised care plan, both at the patient and tooth levels.
Arrive at a diagnosis for each caries lesion
Caries diagnosis is the result of combining the caries severity stage, as determined from visual and radiographic examination (initial, moderate or extensive), with an accompanying lesion activity assessment into the categories below:
Initial active or inactive
Moderate active or inactive
Extensive active or inactive.
Note that, as with patient's caries risk, lesion activity can change over time and therefore so can a lesion's diagnosis. Taking into account the information gathered from the 2nd D (as described in Tables 1, 2, 3 and 4), Figure 3 shows a flowchart that outlines how the process flows from clinical assessment through radiographic assessment and lesion activity assessment to categorise coronal caries lesions as an example.
Arrive at a diagnosis of patient's caries risk
A patient's caries risk will have been determined after analysing history (1st D) and intraoral risk factors, including the presence of active caries lesions (2nd D) (Fig. 2). The influence of caries risk on deciding the appropriate care plan lies mostly at the two extremes of high and low risk. Correctly identifying patients who are particularly at lower risk and those who are at higher risk guides risk-informed appropriate care. Figure 4 shows the caries risk level classification flowchart, outlining the process flows to establish the level of caries risk.
Decide upon the personalised care plan: patient and tooth levels
Patient's risk management plan: this is tailored to the individual patient and will involve actions to protect sound tooth surfaces from developing new caries lesions, arresting currently active lesions, and maintaining inactive lesions from progressing. In addition, it aims to lower the risk status of the patient, if not already low, and to maintain low risk status. A preventive plan should address both homecare and clinical interventions/approaches informed by the caries risk status of the patient.
Tooth-level management plan: information on each caries lesion will be synthesised in terms of whether or not they are likely active and if they are of initial, moderate or extensive severity:
Initial likely active/initial likely inactive
Moderate likely active/moderate likely inactive
Extensive likely active/extensive likely inactive.
Figure 5 shows the patient's care plan flowchart, outlining the logical flow of integrating the management of individual lesions assessed for activity and the management of risk at the patient level. The three management options for surfaces at the end of this flow are keeping sound surfaces sound, controlling lesions with non-operative care, and providing tooth-preserving operative care for only those lesions that need it. The management options to control caries risk at the patient level are also outlined.
Guidance references:1,2,3,4,5,6,7,8,9,10,11,12,13,14,15, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41, 42,43,44,45
4th D: DO: Appropriate tooth-preserving & patient-level prevention & control
The patient perspective
Having finalised a mutually-agreed care plan in the 'decide' phase, the 'DO' phase involves both the planning and implementation of that care plan. Planning is good for both the practitioners and patients; making an explicit plan has repeatedly been shown to ensure adherence to health care recommendations. The do stage is not only about professional treatment but also working with the patient to ensure that they have a clear plan of action to support their own oral health (Fig. 6).
What it is
Appropriate tooth-preserving and patient-level prevention and control is the fourth essential step in the cycle that delivers the personalised comprehensive CariesCare plan built on the outcomes of the first three Ds. This fourth 'D' consists of two elements:
Managing the patient's caries risk, tailored at the individual level with actions to improve the risk status where possible
Managing individual caries lesions according to their severity and activity. Caries care options may differ between the primary and permanent dentition.
How to conduct appropriate tooth-preserving and patient-level prevention and control
Managing the patient's caries risk
-
The caries risk factor management plan can involve two levels:
-
1.
Homecare approach: activities to be conducted at home by the patient or their parent/guardian/carer, as instructed by a member of the dental team, which takes into account the patient's needs, opportunities and preferences. Activities include fluoridated toothpaste use, fluoride rinse/gel, toothbrushing, interproximal cleaning and behaviours related to oral health including diet and other oral hygiene advice
-
2.
Clinical interventions: activities conducted at the practice, including discussing personalised ways of improving oral health-related behaviour, topical fluoride application at a frequency appropriate to the patient's risk classification, sealant application, one-to-one dietary advice (with emphasis on sugars), and, if required, managing hyposalivation or other specific risk factors.
-
1.
-
There is strong evidence for the use of topical fluoride both professionally applied and for home use in the prevention of dental caries
-
Based on the available evidence, concentrate on delivering advice on brushing twice a day with a fluoridated toothpaste that is appropriate to the age of the patient and their risk factors
-
Advice should include basic details of when brushing is most effective and how to maintain the fluoridated toothpaste in contact with the teeth (spit, don't rinse)
-
Emphasis should be placed on improving oral hygiene and delivery of topical fluoride in plaque stagnation areas where caries commonly occurs
-
Given the understanding of the disease process, dietary advice should be directed at identifying sugars in the diet (including hidden sugars), reducing the amount/frequency of sugar intake and suggesting safe alternatives
-
Organise and agree with the patient or their carer a risk-based recall (re-care) interval depending on risk classification.
Managing tooth-level caries lesions
-
Care options for caries lesions include:
-
1.
Non-operative care (NOC); this is non-surgical preventive care to control caries
-
2.
Tooth-preserving operative care (TPOC); this is minimally-interventive surgical treatment.
-
1.
-
The severity status of the caries lesion will inform and dictate preventive (non-operative) or operative management, but lesion activity should also be considered:
-
1.
Initial caries lesions should be managed with non-operative care when active and when inactive should be reviewed at recall appointments for any change in status
-
2.
Moderate caries lesions (ICDAS 3 and 4) management depends on a number of factors including patient-level risk status, radiographic appearance, lesion activity, and whether or not there is surface breakdown; if the lesion radiographically extends up to the outer dentine third (mainly in ICDAS 3 or microcavity) it is feasible to manage with non-operative care if inactive, and in some cases in the absence of other risk factors and if the patient is compliant
-
3.
Extensive caries lesions (ICDAS 5 and 6) should generally be managed with tooth-preserving operative care according to lesion severity and pulp involvement.
-
1.
-
Take into account patient-level strategies for therapeutic control of initial lesions and:
-
1.
In children there is strong evidence for the use of fissure sealants for the caries management of pit and fissure caries, but there is a trend for strict indications for preventive sealants on sound teeth in high caries risk children and an increased focus on therapeutic sealants for initial caries lesions which cannot be controlled by non-operative caries measures
-
2.
Where operative intervention is required, tooth-preserving operative care should be provided according to the patient's needs (age, setting, environment). There is evidence that more conservative caries removal techniques are effective in preserving tooth tissue and avoiding pulpal complications
-
3.
In restored teeth consideration should be given to repair of a restoration rather than re-restoration, where possible, to avoid further loss of tooth tissue by unnecessary removal of sound sections of the old restoration.
-
1.
Good practice points
-
Wherever possible, caries should be managed with prevention (non-operative interventions) to avoid unnecessary surgical intervention
-
Where surgical intervention is required, tooth-preserving operative care should be considered
-
Management options are dependent on patient- and tooth-level assessment (risk, caries lesions, restorative status and patient compliance)
-
In some cases, moderate or extensive inactive caries lesions may require TPOC due to local factors such as the presence of a removable prosthesis or a clasp contacting the lesion
-
Recall interval should be based upon a combination of risk assessment and management as well as clinical procedures carried out
-
Erosive tooth wear, developmental defects of enamel and periodontal status should be considered for comprehensive care
-
Most evidence is based on children, adolescents and young adults but good clinical practice would suggest this is applicable for older adults
-
Note: local adaptations may be required, for example according to varying levels of systemic fluoride concentration
-
The intensity of the risk-based intervention is cumulative, so for patients with higher risk all preventive interventions prescribed for patients with lower caries risk should also be considered
-
Clinicians and their teams should be familiar with evidence-based prevention guidance applicable locally to them
-
Dentists should keep up to date with both changes in cavity preparation philosophy and the requirements and opportunities given by new developments in dental materials
-
Successful use of direct adhesive restorative techniques and materials that require effective moisture control and rubber dam isolation should be considered over relative isolation with cotton rolls
-
As the Minamata treaty is implemented internationally, there is both an opportunity for prevention and a need for caution when dental amalgam is replaced by more technique-sensitive materials.
Guidance references:1,2,3,4,5,6,7,8,9,10,37,38,39,40,41,42, 43,44,45,46,47,48,49,50,51,52,53,54
Concluding key points and guidance for implementation
-
CariesCare International is designed to support dentists and healthcare teams help patients of all ages control the caries process and maintain health over the life course
-
The systematic approach ensures that all the important steps involved in assessing and managing patients' caries status are completed and recorded routinely
-
It is important to deliver all four 'Ds'; they all contribute to optimal care and are required for the continuation of the cycle of care
-
It focuses attention on keeping sound surfaces sound and seeks the arrest/remineralisation of early caries lesions and encourages the use of minimally-invasive techniques when caries removal is necessary
-
It helps to clearly delineate for clinicians when preventive or surgical management of a caries lesion is most appropriate for each patient (taking into account attitudes and attendance behaviour)
-
Risk-based personalised recall and review is a key to deciding how rapidly the 4D cycle repeats
-
The '4D' approach may help stimulate discussion with patients about their risk factors and involve them in determining what can be done to reduce them. For some risk factors this may not only reduce caries risk but may also reduce the risk of other disorders such as obesity and diabetes
-
Health outcomes matter and are the purpose of this approach to care
-
4D caries management is suitable for all ages throughout the life course, but needs some change of emphasis at particular life stages
-
Dentists and the dental and healthcare teams can derive improved professional satisfaction using this patient-centred and preventive approach to caries management
-
Patients value a health-focused and personalised approach to care
-
The CariesCare aspects should integrate well with the rest of routine oral health care, including in particular erosive tooth wear, and periodontal disease assessment and management
-
CariesCare aims to integrate with the rest of health and wellbeing in a holistic way.
Implementation points
-
'Glocal' is the watchword for successful implementation. This concept has been used successfully by the Alliance for a Cavity Free Future and takes key evidence from global evidence and consensus and adapts it to the local realities and cultures in specific countries, areas and practice settings
-
Modifications to reflect local needs are acceptable, but care needs to be taken not to destroy the fundamentals of the CariesCare 4D system
-
An educational online course (a 'MOOC') will be made available in the near future and there are tools already available, like training in visual caries criteria e-learning and the CariesCare clinical case which will follow this paper
-
Collecting the required information efficiently on paper records can and is being done
-
However, moving forward, software development will ultimately help further integration into practice and help with integrated longitudinal health assessments
-
The shift in resource allocation towards prevention and 'paying for health in dentistry' are important in supporting dental teams in delivering the CariesCare International approach to caries prevention, control and management
-
In due course, CariesCare International plans to develop as a community to support implementation and development. Current examples include: 1) a consensus group of stakeholders co-creating a core Colombian oral health record; 2) a National French experiment looking at supporting the introduction of 4D caries management in general practice.
CariesCare International (Fig. 7) is working with the Alliance for a Cavity Free Future and King's College London under the umbrella of the Global Collaboratory for Caries Management to help further implementation of this guide.
Change history
13 December 2019
Author's correction note: Clinical article 2019; 353-362. When this article was initially published, one of the boxes in Figure 6 had been duplicated. The correct figure is shown below: Also, Matteo Basso's affiliation in the Acknowledgements section was incorrect. It should have read 'Matteo Bass...
References
Pitts N B, Ekstrand K R, ICDAS Foundation. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS) - methods for staging of the caries process and enabling dentists to manage caries. Community Dent Oral Epidemiol 2013; 41: e41-e52.
Pitts N B, Ismail A I, Martignon S, Ekstrand K, Douglas G V A, Longbottom C. ICCMS™ Guide for Practitioners and Educators. 2014. Available at http://doi.org/10.5281/zenodo.853106 (accessed May 2019).
Ismail A I, Pitts N B, Tellez M et al. The International Caries Classification and Management System (ICCMS™) An Example of a Caries Management Pathway. BMC Oral Health 2015; 15 (Spec Iss): S9.
International Caries Classification and Management System (ICCMS™). Available at https://www.iccms-web.com/ (accessed May 2019).
Pitts N. "ICDAS" - an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health 2004; 21: 193-198.
Ismail A I, Sohn W, Tellez M et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 2007; 35: 170-178.
Selwitz R H, Ismail A I, Pitts N B. Dental caries. Lancet 2007; 369: 51-59.
Pitts N B, Zero D T, Marsh P D et al. Dental caries. Nat Rev Dis Primers 2017; 3: 17030.
Pitts N B, Grant J, Hinrichs-Krapels S, Mazevet M E, Boulding H F, Mayne C. Towards a cavity free future: how do we accelerate a policy shift towards increased resource allocation for caries prevention and control? The Policy Institute at King's 2017. Available at: https://www.researchgate.net/publication/326776201_Towards_a_cavity-free_future_How_do_we_accelerate_a_policy_shift_towards_increased_resource_allocation_for_caries_prevention_and_control (accessed May 2019)
Pitts N B, Mazevet M E, Boulding H. Towards paying for health in dentistry How can we create and implement acceptable prevention-based dental payment systems to achieve and maintain health outcomes? The Policy Institute at King's 2019. Available at: http://www.acffglobal.org/wp-content/uploads/2019/02/Towards-paying-for-health-in-Dentistry-Policy-Lab-Report.pdf (accessed May 2019).
Beighton D. Consensus Statements. Caries Res 2017; 51: I-II.
Bratthall D, Hänsel Petersson G. Cariogram - a multifactorial risk assessment model for a multifactorial disease. Community Dent Oral Epidemiol 2005; 33: 256-264.
Twetman S, Fontana M. Patient caries risk assessment. Monogr Oral Sci 2009; 21: 91-101.
Twetman S, Fontana M, Featherstone J D. Risk assessment - can we achieve consensus? Community Dent Oral Epidemiol 2013; 41: e64-e70.
Tellez M, Gomez J, Pretty I, Ellwood R, Ismail A I. Evidence on existing caries risk assessment systems: are they predictive of future caries? Community Dent Oral Epidemiol 2013; 41: 67-78.
Baginska J, Stowska W. Pulpal involvement-roots-sepsis index: a new method for describing the clinical consequences of untreated dental caries. Med Princ Pract 2013; 22: 555-560.
Moynihan P J, Kelly S A. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res 2014; 93: 8-18.
Cagetti M G, Bontà G, Cocco F, Lingstrom P, Strohmenger L, Campus G. Are standardized caries risk assessment models effective in assessing actual caries status and future caries increment? A systematic review. BMC Oral Health 2018; 18: 123.
Featherstone J D B, Alston P, Chaffee B W, Rechmann P. Caries Management by Risk Assessment (CAMBRA): An Update for Use in Clinical Practice for Patients Aged 6 Through Adult. In CAMBRA: A Comprehensive Caries Management Guide for Dental Professionals. Sacramento: California Dental Association, 2019. Available at https://www.cdafoundation.org/Portals/0/pdfs/cambra_handbook.pdf (accessed May 2019).
Featherstone J D B, Crystal Y O, Chaffee B W, Zhan L, Ramos-Gomez F. An Updated CAMBRA Caries Risk Assessment Tool for Ages 0 to 5 Years. In CAMBRA: A Comprehensive Caries Management Guide for Dental Professionals. Sacramento: California Dental Association, 2019. Available at https://www.cdafoundation.org/Portals/0/pdfs/cambra_handbook.pdf (accessed May 2019).
INTERVAL Dental Recall Trial. Health Technology Assessment. Report in preparation for release NIHR. 2019.
Ekstrand K R, Ricketts D N, Kidd E A. Occlusal caries: pathology, diagnosis and logical management. Dent Update 2001; 28: 380-387.
Ekstrand K R, Martignon S, Ricketts D J, Qvist V. Detection and activity assessment of primary coronal caries lesions: a methodologic study. Oper Dent 2007; 32: 225-235.
Braga M M, Martignon S, Ekstrand K R, Ricketts D N, Imparato J C, Mendes F M. Parameters associated with active caries lesions assessed by two different visual scoring systems on occlusal surfaces of primary molars - a multilevel approach. Community Dent Oral Epidemiol 2010; 38: 549-558.
Braga M M, Ekstrand K R, Martignon S, Imparato J C, Ricketts D N, Mendes F M. Clinical performance of two visual scoring systems in detecting and assessing activity status of occlusal caries in primary teeth. Caries Res 2010; 44: 300-308.
Ekstrand K R, Luna L E, Promisiero L et al. The reliability and accuracy of two methods for proximal caries detection and depth on directly visible proximal surfaces: an in vitro study. Caries Res 2011; 45: 93-99.
Brocklehurst P, Ashley J, Walsh T, Tickle M. Relative performance of different dental professional groups in screening for occlusal caries. Community Dent Oral Epidemiol 2012; 40: 239-246.
Ekstrand K R, Poulsen J E, Hede B, Twetman S, Qvist V, Ellwood R P. A randomized clinical trial of the anti-caries efficacy of 5,000 compared to 1,450 ppm fluoridated toothpaste on root caries lesions in elderly disabled nursing home residents. Caries Res 2013; 47: 391-398.
Banerjee A, Watson T F. Pickard's guide to minimally invasive operative dentistry. 10th ed. Oxford: Oxford University Press, 2015.
Gimenez T, Piovesan C, Braga M M et al. Visual inspection for caries detection: a systematic review and meta-analysis. J Dent Res 2015; 94: 895-904.
Pretty I A, Ekstrand K R. Detection and monitoring of early caries lesions: a review. Eur Arch Paediatr Dent 2016; 17: 13-25.
Mattos-Silveira J, Oliveira M M, Matos R, Moura-Netto C, Mendes F M, Braga M M. Do the ball-ended probe cause less damage than sharp explorers? An ultrastructural analysis. BMC Oral Health 2016; 16: 39.
Cortes A, Ekstrand K R, Martignon S. Visual and radiographic merged-ICDAS caries progression pattern in 2-6 years old Colombian children: two-year follow-up. Int J Paediatr Dent 2019; 29: 203-212.
Ekstrand K R, Gimenez T, Ferreira F R, Mendes F M, Braga M M. The International Caries Detection and Assessment System - ICDAS: A Systematic Review. Caries Res 2018; 52: 406-419.
Martignon S, Cortes A, Gómez S I et al. How long does it take to examine young children with the caries ICDAS system and how do they respond? Braz Dent J 2018; 29: 374-380.
Drancourt N, Roger-Leroi V, Martignon S, Jablonski-Momeni A, Pitts N, Doméjean S. Carious lesion activity assessment in clinical practice: a systematic review. Clin Oral Investig 2019; 23: 1513-1524.
Hänsel Petersson G, Åkerman S, Isberg P E, Ericson D. Comparison of risk assessment based on clinical judgement and Cariogram in addition to patient perceived treatment need. BMC Oral Health 2016; 17: 13.
Schwendicke F, Frencken J E, Bjørndal L et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res 2016; 28: 58-67.
Kühnisch J, Ekstrand K R, Pretty I et al. Best clinical practice guidance for management of early caries lesions in children and young adults: an EAPD policy document. Eur Arch Paediatr Dent 2016; 17: 3-12.
Tonetti M S, Bottenberg P, Conrads G et al. Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing - Consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 2017; 44 (Spec Iss): S135-S144.
Slayton R L, Urquhart O, Araujo M W B et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions. A report from the American Dental Association. J Am Dent Assoc 2018; 149: 837-849.
Ricketts D, Innes N, Schwendicke F. Selective removal of carious tissue. Monogr Oral Sci 2018; 27: 82-91.
Fontana M, Pilcher L, Tampi M P et al. Caries management for the modern age: improving practice one guideline at a time. J Am Dent Assoc 2018; 149: 935-937.
Rechmann P, Chaffee B W, Rechmann B M T, Featherstone J D B. Caries Management by Risk Assessment: Results from a Practice-Based Research Network Study. J Calif Dent Assoc 2019; 47: 15-24.
Urquhart O, Tampi M P, Pilcher L et al. Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res 2019; 98: 14-26.
National Institute for Health and Care Excellence. Dental checks: intervals between oral health reviews. 2004. Available at https://www.nice.org.uk/guidance/CG19 (accessed May 2019).
Splieth C H, Ekstrand K R, Alkilzy M et al. Sealants in dentistry: outcomes of the ORCA Saturday Afternoon Symposium 2007. Caries Res 2010; 44: 3-13.
Ricketts D, Lamont T, Innes N P, Kidd E, Clarkson J E. Operative caries management in adults and children. Cochrane Database Syst Rev 2013; CD003808. DOI: 10.1002/14651858.CD003808.pub3.
Tellez M, Gomez J, Kaur S, Pretty I A, Ellwood R, Ismail A I. Non-surgical management methods of noncavitated carious lesions. Community Dent Oral Epidemiol 2013; 41: 79-96.
Marinho V C, Worthington H V, Walsh T, Clarkson J E. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2013; CD002279. DOI: 10.1002/14651858.CD002279.pub2.
Marinho V C, Chong L Y, Worthington H V, Walsh T. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2016; CD002284. DOI: 10.1002/14651858.CD002284.pub2.
Innes N P, Frencken J E, Bjørndal L et al. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res 2016; 28: 49-57.
Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington H V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev 2017; CD001830. DOI: 10.1002/14651858.CD001830.pub5.
Walsh T, Worthington H V, Glenny A M, Marinho V C, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev 2019; CD007868. DOI: 10.1002/14651858.CD007868.pub3.
Acknowledgements
The Authors acknowledge the research conducted by many contributors that underpinned this CariesCare International Guide and are indebted to the contributions made by all of the internationally mixed groups who attended the launch meeting of the Global Collaboratory for Caries Management at Kings College London in 2013 and the many who have helped since at meetings in Liverpool, Seattle, Philadelphia, London, Capetown, Greifswald, Dubai, Delhi and Tokyo to drive the ICCMSä initiative forward. We are also exceedingly grateful to all the individuals who have helped shape the CariesCare International initiative at meetings in Athens, Oslo, Copenhagen, Buenos Aires and London as well as to the numerous organisations and companies who have helped support this work and enabled progress to date. Acknowledgement as consensus contributors: Ninoska Abreu-Placeres, Universidad Iberoamericana, Dominican Republic; University of Copenhagen, Denmark; Ben Amaechi, University of Texas Health Science Centre at San Antonio, USA; Matteo Basso, University of Torino, Italy; Mariana Braga, University of São Paulo, Brazil; Jeroen Van den Bulcke, Ghent University, Belgium; Iain L. C. Chapple, University of Birmingham, UK; Andrea Cortes, Universidad El Bosque, Colombia; Bhupinder Dawett, Hafren House Dental Practice at Derbyshire, UK; Bernadette K. Drummond, University of Leeds, UK; Kim Ekstrand, University of Copenhagen, Denmark; Margherita Fontana, University of Michigan, USA; Thomas Lamont, University of Dundee, UK; Adrian Lussi, University of Bern, Switzerland; David Manton, University of Melbourne, Australia; Paulo Melo, University of Oporto, Portugal; Michelle Muller-Bolla, Université Côte d' Azur, France; Mike McGrady, NHS Greater Glasgow and Clyde, UK; Marcelle Nascimento, University of Florida, USA; Hien Ngo, Kuwait University, Kuwait; Francisco Ramos-Gomez, UCLA School of Dentistry, USA; Eric Rooney, NHS Central Lancashire, UK; Susie Sanderson, British Dental Association (BDA), UK; Falk Schwendicke, Charité - Universitätsmedizin Berlin, Germany; Woosung Sohn, University of Sydney School of Dentistry, Australia; Christian Splieth, Greifswald University, Germany; Seiichi Sugiyama, Sugiyama Dental Clinic Chiba-ken, Japan; Angus Walls, University of Edinburgh, UK; David Wiliams, Bart's and The London School of Medicine and Dentistry, UK; Alix Young, University of Oslo, Norway; Andrea Zandona, Tufts University, USA; Olga Lucía Zarta, Universidad El Bosque, Colombia; Dom Zero, Indiana University, USA. Finally, we are grateful to Edgar O Beltrán, Universidad El Bosque, for his contribution with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martignon, S., Pitts, N., Goffin, G. et al. CariesCare practice guide: consensus on evidence into practice. Br Dent J 227, 353–362 (2019). https://doi.org/10.1038/s41415-019-0678-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0678-8
This article is cited by
-
Oral health literacy and its association with oral health-related quality of life amongst pregnant women: a cross-sectional study
Quality of Life Research (2024)
-
ORCA-EFCD consensus report on clinical recommendation for caries diagnosis. Paper I: caries lesion detection and depth assessment
Clinical Oral Investigations (2024)
-
Clinical practice guideline adaptation for risk-based caries management in 18–55 year-old Iranian adults
BMC Oral Health (2023)
-
Knowledge and attitudes toward evidence-based cariology and restorative dentistry among Egyptian dental practitioners: a cross-sectional survey
BMC Oral Health (2023)
-
Factors perceived by health professionals to be barriers or facilitators to caries prevention in children: a systematic review
BMC Oral Health (2023)