Abstract
Aim This research was undertaken to explore NHS general dentistry in Wales, from the perspective of both the dental practice and the general population, in order to understand patient access to NHS general dentistry. The health boards' dental budgets, and how well they have been used for primary care general dentistry, were examined. Contributory factors to patient access problems were also examined.
Background Our research shows that access for new patients has dropped to an all-time low in recent years. Causation is multifactorial. In Wales, dentists must achieve 95% of their UDA target or their practice will face 'clawback'; having to pay back monies for not achieving UDA targets. Practices may also hand back monies from their contract if they feel they will end up facing clawback at the year's end.
Methods The clawback and handback data, budgetary and contract reduction data, and practice opening and closures numbers, were acquired in the period of March 2017 to April 2018 via a series of freedom of information requests to each of the Welsh health boards. Telephone interviews with dentists and practice owners were conducted in the summer of 2017. Patient access information was gathered from the health boards and from contacting dental practices where this information was not available.
Results It was found that, on average, only 15% of all NHS practices in Wales were accepting adult NHS patients in 2017-2018 and 21% of all NHS practices had waiting lists. Cwm Taf had the best access to an NHS dentist, however, this figure was not high at 52% (15 practices). Cardiff and Vale patients were the most likely to struggle to find a dentist, with just two practices in the whole health board accepting adult NHS patients. In Wales, clawback and handback resulted in £16,322,445 of the general dental service (GDS) budget being unspent from 2014/2015 to 2016/2017. This figure increases in consideration of the monies lost from practices through contract reduction, with contracts being reduced by more than £4,000,000 from 2014/2015 to 2016/2017, making a total of £20,322,445 of the budget not being spent on NHS dentistry over a period of three years. This means that, on average, 6% of the Welsh GDS budget was unspent every year between 2014 and 2017.
Conclusion Dentists want to be able to treat more patients and see more patients with a higher need, but limitations upon patient access and the fear of clawback within the current contract make this very difficult. An increasing population and a further handback of NHS contracts mean it is likely that this problem of access will continue to worsen. The current system of clawback and handback only exacerbates the access problem because taking on new patients is a risk to dentists trying to achieve such tightly managed targets. Dentists are incentivised in the current UDA contract to treat healthy patients. A larger proportion of high needs patients can result in a practice failing to reach its targets and facing clawback, handback or contract reduction. Clawback is prevalent in all health boards, meaning that patients with poor oral health are disproportionately affected. Inverse care law is felt acutely in general dentistry.
Similar content being viewed by others
Key points
-
Presents data on access for new patients to NHS GDS in Wales and the need for ongoing review of access to NHS dentistry.
-
Highlights the inappropriate nature of the current NHS dental contract and the detrimental impact on access for high-needs patients.
-
Supports how health boards should be held accountable for underspend of the dental budget.
Introduction
Aim of the study
The aim of this study is to gain a deeper understanding of NHS general dentistry in Wales and the challenges being faced. There are many anecdotes from dentists and patients that tell a consistent story; NHS dentistry in Wales is heading towards a crisis point. However, data to verify this have been slim. The first data set that verified these anecdotes came with the responses to the handback and clawback freedom of information requests in 2017. Further data were needed to be gathered, as clawback figures were only part of the picture. The difficulties experienced trying to access an NHS dentist needed to be quantified. Furthermore, contract reduction figures would tell us what was happening to NHS dental contracts on a more permanent basis. Once the data had been obtained, it was possible to compare the clawback figures, contract reduction figures, access figures, practice closures, and anecdotal reports to gain a clearer picture of the challenges being faced by NHS Wales dentistry. The aim of the study was also to see these problems through the lens of each health board, each with different patient circumstances and challenges. The study aimed to discover how well each health board was serving NHS general dentistry in Wales.
Background
A perceived looming crisis of access to dentistry in Wales is one that has been discussed by the public and the press but has not been the subject of systematic research. Members of the public often vent their frustrations of not being able to find an NHS dentist on electronic message boards.1 Forum-based website 'Mumsnet' has hundreds of posts regarding the struggle to find an NHS dentist, many of which specify that they are in Wales.1 This has also been reported in the media.2 This begs the questions, why is there a problem of access to NHS dentistry in Wales and how can the Welsh government address this growing problem?
Alongside deteriorating patient access, dentists are still fighting the conditions that the 2006 NHS contract has caused for treating patients. Contrary to popular belief, the 2006 contract means that patients are no longer registered with a dental practice. The contract puts dental practices under intense pressure. Regardless of size, dental practices must run as businesses in providing NHS care; which means all staff wages, all technical costs and business expenses such as running the premises, must come out the monies provided via the annual contract from the respective health board. Dentists must achieve 95% of their units of dental activity (UDA) target or they will face clawback; having to pay back monies for not achieving UDA targets. In Wales, clawback is handled by the health boards which are: Betsi Cadwaladr, Powys Teaching, Hywel Dda, Cardiff and Vale, Abertawe Bro Morgannwg, Cwm Taf, and Aneurin Bevan. Each of these health boards handles clawback differently. In Cwm Taf, for example, if a dentist achieves 95% or more of their contracted UDAs they carry forward the shortfall of UDAs to the next financial year. If they achieve less than 95% then they must repay funding to the health board. Therefore, if a dentist achieves only 90% of their UDAs they must repay 10% to the health board. In Aneurin Bevan, if a dentist achieves only 90% of their UDAs they may carry forward 5% of their shortfall of UDAs to the next financial year and must repay 5% as clawback. The practice has the option to have the entire 10% clawed back if they prefer. In Hywel Dda, all matters of underperformance are discussed at the health board's dental planning performance and delivery group meetings, held among the primary care team where each case is discussed on an individual basis. Thus, this lack of uniformity in clawback policy between health boards means that dentists who have failed to hit their UDA targets can be differentially affected according to the location of their practice.
NHS general dentistry in Wales is at a time of significant change. The number of providers who are also NHS performers (providing-performers) across Wales has more than halved in the eight years from 2010 to 2018, from 418 to 155, a 63% fall.3 This means that the dental team is changing greatly, with an increasing number of NHS contract holders no longer performing NHS dentistry. The fall in providing-performers is unexplained, however, if numbers continue to decline at this rate there will be no providing-performers performing NHS dentistry in a few years' time.
The current dental contract creates an inverse care law. A dentist facing clawback could have worked longer hours and helped more patients with challenging ailments than a dentist who had completed their UDA targets. This is in part due to the banded systems in relation to UDAs. One dentist could earn 20 UDAs in five hours from 20, ten-minute examinations of healthy patients. Another dentist could earn three UDAs in five hours completing several extractions, fillings and root canals for a single patient with poor oral health. This means that patients with higher dental needs are a disadvantage to a dentist because practices are under intense pressure to hit their UDA targets, resulting in insufficient time to treat high needs patients. Over 90% of dentists say they believe that the 2006 contract has limited their capacity to treat patients with high needs.4 Nevertheless, since the inception of the 2006 general dental services (GDS) contract, many practices have struggled to hit their UDA targets; with almost half (47.6%) of dentists in England and Wales failing to achieve 96% of their UDA target in 2007.5 It should be noted that the published literature on UDA targets appears very sparse. More research must be done to provide a thorough and public examination of the current system.
Methods
The initial data of this project were gathered through freedom of information (FOI) requests to each of the Welsh health boards. The requests asked health boards for the number of practices, and their locations as specifically as possible, that had experienced clawback and handback from 2014/2015 to 2016/2017. We also asked how much money had been clawed or handed back. On analysis of these data, more questions were raised. It was clear that clawback was occurring in all health boards. This prompted a telephone survey of practices to discover the reasons for clawback. The flowchart used for this survey can be seen in Appendix 1.
Some health boards publicly display on various websites their NHS dental practices and whether they are accepting different classifications of patients. Other health boards, such as Cardiff and Vale, do not display this information. To gather this information, a practice list was obtained via Health Inspectorate Wales and the health boards' website. Practices were then contacted regarding the patient classifications they were accepting and whether they had a waiting list.
Meanwhile, one practice owner disclosed the hardship they were facing due to contract reduction. Upon hearing this, a further FOI was sent out to all health boards to discover the number of practices facing contract reduction, and by how much their contract was being reduced. This would allow a deeper understanding of how much of the GDS budget per health board was not being spent. A FOI request was also sent to the health boards to discover the GDS budgets for the last three years. During the telephone interviews, a practice disclosed that they had not faced contract reduction the previous year because of the number of practices that had closed in the surrounding area. This resulted in a FOI request to discover the openings and closures of dental practices in the last five years.
FOI requests were sent to all health boards in Wales to identify how the monies that were clawed and handed back were being invested. However, several replies were still outstanding many months later.
Results
Clawback and handback
Table1 shows the results of the FOI request into the amount of monies clawed or handed back for each of the health boards in Wales. In three years, from 2014/15 to 2016/17, a total of £16,322,445 was clawed or handed back to the health boards in Wales. It is of particular note that total clawback in Wales more than doubled between 2014/15 to 2015/16, and then remained at that level the following year 2016/17.
Some health boards, such as Aneurin Bevan, consistently experienced clawback of similar amounts. Other health boards, such as Hywel Dda, experienced spikes in clawback. Handback across Wales showed fewer trends, with health boards who had not experienced handback the previous year seeing a spike of £70,000 being handed back, as was the case for Cwm Taf. Table 2 shows the number and percentage of practices affected by clawback and handback over the three years. There were 50% and over of practices in both Betsi Cadwaladr and Powys Teaching boards that suffered clawback in each of the three years. In the other five health boards, on average, approximately a quarter of all practices were affected by clawback.
Contract reduction
Table 3 shows the amount of contract reduction and numbers of practices affected over the three-year period between 2014/2015 to 2016/2017. It can be seen that 26.5% of all NHS practices in Wales experienced contract reduction in the period. This amounts to approximately £4,323,078 removed from the GDS budget. Hywel Dda Health Board alone experienced more than half of this contract reduction.
Practices ceasing to provide NHS dental services
Table 4 shows the number of practices in Wales that have started or ceased to provide NHS dental services over the last six years. While most health boards have a similar openings/closings ratio, Betsi Cadwaladr experienced a net loss of eight practices providing NHS services. This is clearly a concern and is likely a contributory factor as to why only just 10% of practices in that health board are accepting NHS patients.
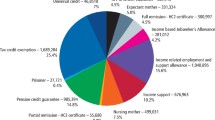
The GDS budgets of health boards
Table 5 shows the GDS budget per health board for the last three years, 2014/15 to 2016/17, and the amounts of clawback, handback and contract reduction within the GDS service in Wales, which are also expressed as a percentage of the GDS budget for each health board. It can be seen that millions of pounds of the GDS budget went unspent due to these factors. Hywel Dda and Powys Teaching had an average of 14.7% and 15.8%, respectively, of their GDS budget unspent over the last three years, not including contract reductions. These two figures are significantly higher than the average underspend of 5%. Figure 1 shows the average unspent GDS budget over three years, including contract reductions, for each health board. It can be seen that, when contract reduction is included in the calculation, nearly one fifth of the GDS budget was unspent in the Powys Teaching and Hywel Dda health boards.
Dental practices accepting new NHS patients
Table 6 shows how many practices from each health board were accepting patients in 2017 according to a variety of patient classifications. The various patient classifications were created by the health boards. The data are shown as both a percentage and the number of practices. The results for the whole of Wales are also graphically summarised in Figure 2. Figure 3 shows the percentage of practices holding an NHS contract that were accepting new NHS patients compared with accepting new private patients in 2017 in each health board.
Perceptions of practices regarding their NHS contracts
Table 7 summarises the key themes that emerged from the telephone interviews across the health boards and the perceptions regarding clawback; the impact of recruitment and retention; the difficulty of meeting UDA targets; and how well the practices felt they were serving their local communities.
Discussion
Analysis of qualitative data
The telephone survey was prompted by the results of FOI requests which had been sent to each of the Welsh health boards. The telephone interviews were conducted with practice owners or managers across Wales. The key themes of the telephone interviews were recruitment and retention of staff, the UDA system, clawback and handback, and the issue of access.
These interviews allowed for a deeper understanding of the nature of the clawback from practice to practice and health board to health board, and the key themes are summarised in Table 7. Of those practices interviewed, 57% said they were facing clawback and many disclosed that they were facing an increased level of clawback. The reasons were varied. While some practices had experienced problems with recruitment, others experienced challenges with the UDA system, not least the fact that some UDA values were below a viable value. While only one interviewee agreed with the current UDA system, many believed that several factors made working within the UDA system and achieving targets more difficult. Of the practices interviewed, 43% stated that regular check-ups for those with good oral health made UDA achievements much easier; one interviewee expressed that they felt this was a flaw in the contract as it was morally wrong. A dentist in Cardiff and Vale discussed the difficulty they were having with the size of their contract. They believed it was much too small to treat the patients living in their area and as a result they were forced to add patients to a waiting list which stood at over 300 patients long.
Of those practices interviewed, 50% stated they had experienced clawback due to recruitment and retention struggles. A practice in Cwm Taf contracted with an associate who ultimately decided not to join the practice. After experiencing an extended and difficult recruitment period the practice eventually contracted with an associate part-time. This meant the practice was unable to fulfil their UDA target. This last year, however, the staffing issues were resolved and the practice achieved their UDA target. Some 30% of practices interviewed stated they were aware of an access crisis in NHS Wales dentistry. One was in a rural setting and could not see a majority of the 7,000 patients in their area.
Analysis of quantitative data
There is a clear access problem in Wales, with only 52 out of 354 practices in Wales accepting 'new' adult NHS patients in 2017. This is just 15% of all practices. The figures for accepting children were somewhat better at 28%, but still low. Waiting lists were a further considerable obstacle, as patients could be part of a waiting list having over 300 other patients.
Each health board's data told a varying story regarding access figures. While some health boards published online whether their practices were accepting patients, others did not. The final data were gathered using a mixture of available data and telephoning the practices to ask about their patient availability. Cwm Taf had the best access to an NHS dentist, standing at 52% (15 practices). Cardiff and Vale had the worst access, with just two practices (3%) in the health board accepting new adult NHS patients and only four (6%) accepting children.
The data in Table 6 show that if the practice had a waiting list it was included in the data. As can be seen, some health boards and practices considered their practice to be accepting patients if they had a waiting list; others deemed that if they had a waiting list, they were not accepting patients. The waiting lists themselves were also something that needed close examination. The length of time patients could be waiting, as disclosed by practices, varied from weeks to over a year. However, many practices did not disclose the length of time. Therefore, practices that were accepting patients with a waiting list might not be accepting these new patients for treatment for many months.
The data in Table 1 show that clawback and handback in Wales were becoming an increasing problem, with the total monies clawed or handed back more than doubling from 2014/15 to 2015/16. Moreover, there was considerable variation between health boards and two in particular, Powys Teaching and Hywel Dda, showed a significant total underspend of circa one-fifth of their GDS budget during that three-year period, as shown in Figure 1. These figures were alarming and led us to the conclusion that clawback was likely a causative factor of the access problem.
Each health board had its own story in terms of access, clawback and handback. Health boards faced different challenges; some had a largely rural population, for example. It is important when looking at dentistry in Wales that circumstances are viewed through the lenses of the different health boards. This gives a more granular picture in terms of what dentists in Wales are facing and what patients are experiencing. The following sections consider each health board in turn.
Betsi Cadwaladr Health Board
Betsi Cadwaladr Health Board is experiencing an access crisis. Only 10% of all practices with NHS contracts in Betsi Cadwaladr in 2017 were accepting new NHS patients. This equates to just seven practices. They also had the second lowest percentage of practices accepting charge-exempt NHS patients at just 10%. Betsi Cadwaladr is home to the practice which disclosed the longest waiting time; this waiting list was three years long and yet the practice was deemed as 'accepting patients'. Of the seven practices accepting NHS patients, only one of them did not have a waiting list. Betsi Cadwaladr has experienced a population rise of 1.6% since 2009; this means that at least 11,247 patients were not included in current dental budgets.
As can be seen in Table 1, Betsi Cadwaladr had high levels of clawback with £1,045,106 being clawed back in 2016/2017 alone. While clawback and handback reflect that the dental budget was not being spent yearly, this is only part of the story. One practice owner disclosed the problems they were having with contract reduction. Betsi Cadwaladr had the highest number of permanent contract reductions, with 18 practices having their contract reduced between 2014/2015 and 2016/2017. This equates to £318,382. This meant that, with clawback and handback, over £4,000,000 had been underspent by Betsi in the last three years, which was 5% of Betsi Cadwaladr's GDS budget. During the telephone interviews, a practice in Betsi Cadwaladr explained that the only NHS patients they treated were children. They believed that the current contract only allowed prevention-focused treatment on children. They felt that if they were to take on adult patients, they would experience clawback.
Betsi Cadwaladr had experienced the closure of NHS contracts in nine practices in the last five years, with only one practice opening an NHS contract. This means that a net loss of eight practices offering NHS treatment had occurred in the last six years. Betsi Cadwaladr practices are under the intense pressure of treating a rising population with a dwindling number of practices but are nevertheless suffering high levels of clawback. This is a bad situation for patients and would-be patients.
Powys Teaching Health Board
Powys Teaching Health Board also has an access problem, with only 20% of NHS practices accepting new NHS patients in 2017. This equated to just four practices, all of which had waiting lists. Two of these practices disclosed their waiting lists as taking two months and four months. Clawback and handback created a strain on practices in this health board, with £828,786 being clawed or handed back in 2016/2017. This meant that 16.4% of Powys Teaching Health Board's general dental budget for 2016/2017 was clawed or handed back. Overall, an average of 15.8% of the GDS budget was not spent on dentistry every year for three years from 2014/2015 to 2016/2017. However, this is only part of the story. As can be seen in Table 3, 11 practices (55%) experienced contract reduction in Powys Teaching Health Board in the last three years.
Over the last three years, approximately £2,435,608.64 was clawed back, handed back or reduced from the GDS contract. If the contract reductions are included in the calculation, then 19% of the budget in the three-year period was unspent or reduced. That is to say, one-fifth of the budget was not available for patients' treatment.
During the telephone interviews, a practice in Powys revealed that they had experienced two years of clawback. While they did not experience contract reduction, they would have lost the contract if they had not met their target the following year. They believed that clawback, handback and contract reduction happened frequently in Powys due to staffing difficulties. They discussed the difficulties of recruiting and retaining dentists in more rural areas. This practice revealed that the reason they managed to achieve their target in 2016-17 was because several practices in the surrounding area had closed. This meant that this practice took on more patients who regularly saw a dentist and had a good standard of oral health.
While conducting this telephone survey, several practices listed on the health board website as open were uncontactable, leading to a question as to whether they really were still functioning practices. Powys Health Board stated that zero practices had closed their NHS contracts in the last three years, which is at odds with the intelligence from the dental practice mentioned.
Hywel Dda Health Board
Access was also problematic in Hywel Dda, with only 21% of practices accepting new adult NHS patients in 2017. This equates to nine practices, all of which had waiting lists ranging from one to nine months. These nine practices were also the only NHS practices in Hywel Dda to accept children, young people with learning disabilities, and charge-exempt patients. Hywel Dda also had high levels of clawback and handback, with £1,452,696 clawed back in 2016/2017. Hywel Dda had the highest levels of contract reduction in Wales, with over 20 practices experiencing contract reduction in the last three years, amounting to £2,233,391; this is ten times as much as the Cardiff and Vale Health Board. This has had a huge impact on the Hywel Dda GDS budget. From 2014/2015 to 2016/2017, clawback, handback and contract reduction caused an underspend of £5,447,161 in Hywel Dda's budget. This equates to an average of 14.7% of the budget every year over three years. If the contracts had not been reduced the underspend would have been a very significant 19.6% or one-fifth of the total 'budget' (Table 5). Hywel Dda was experiencing contract reduction, however, they were attempting to address it so that £1,336,214 of the £2,233,391 was meant to be a 'temporary contract reduction' for that year.
Abertawe Bro Morgannwg Health Board
Access in Abertawe Bro Morgannwg Health Board (ABMU) was complex. While only 14% of NHS practices were accepting NHS patients in 2017, there was also a postcode lottery in ABMU. One practice was only accepting patients from an SA12 or SA13 postcode. Some 20% of practices had a waiting list, and only two of these practices disclosed the length of the waiting list. Clawback, handback and contract reduction were problematic for ABMU. On average, 26 practices a year were experiencing clawback. From 2014/2015 to 2016/2017, the monies clawed back, handed back or obtained through contract reduction amounted to £3,213,441 of ABMU's GDS budget.
During the telephone interviews, one practice in ABMU discussed the concerns they had about clawback. They had experienced it for the two previous years and the practice manager felt extremely stressed. They stated that they were unable to reach their targets and did not know why. From 2009 to 2016, a 3% increase in the population of the health board occurred; this meant 16,657 more patients now lived in ABMU. ABMU was experiencing a rise in population, while simultaneously experiencing a rise in clawback, handback and GDS contract reduction.
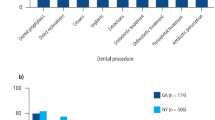
ABMU also has high levels of deprivation.6 Deprivation has been shown to have a negative effect on oral health. Children in Wales receiving free school meals aged 12 were 6% more likely to have had toothache in the last three months than those not eligible for free school meals. Among 15-year-olds this divide increases, with those eligible for school meals being more than twice as likely to have experienced toothache in the last three months.7 This means that practices within areas of higher deprivation are further deterred from treating new patients, as their poor oral health could result in clawback or even contract reduction. It is vital to remember that 'poor oral health' can range from the need for multiple fillings to the full clearance of a patient's teeth. Some dentists disclosed that they had to remove all the teeth from patients as young as 13. The 2018 report by ABMU Community Health Council (CHC), interviewed 53 homeless and 'vulnerably housed' people in Swansea, Neath Port Talbot and Bridgend, and found that few could access emergency dental treatment due to the cost of travelling and many had severe dental problems.
Aneurin Bevan Health Board
Aneurin Bevan Health Board had one of the worst access levels for Wales: In 2017, a mere six practices were accepting adult NHS patients, which equated to just 8% of all NHS practices in Aneurin Bevan. These practices all had waiting lists, as did 28% of all NHS practices in the health board. Of those disclosing the timings of their waiting lists, it ranged from one month to nine months. Aneurin Bevan's access levels meant that it had a practice that, while not accepting NHS patients, it needed to put private patients on a waiting list that was several weeks long. Twenty practices in Aneurin Bevan were consistently experiencing clawback and handback of approximately half a million pounds a year, with a further 15 practices experiencing contract reduction in the last three years. Yet Aneurin Bevan had seen a population rise of 11,615 from 2009 to 2016. Clearly the population needs were being increasingly unmet.
Cwm Taf Health Board
Cwm Taf had the best access figures in Wales, with 52% of practices accepting adult NHS patients in 2017. They also had the highest percentage of practices accepting NHS patients in the category 'children up to secondary school age' (up to 16 years of age or 18 years of age if in full-time education) with 59% accepting. The average of the other six health boards was 25%. Cwm Taf Health Board also had the lowest amount of clawback in Wales, at £1,402,929 over three years. While this is still a large sum of money, Cwm Taf was forthcoming with how they reinvested this money into dentistry. Although Cwm Taf is a smaller health board, it had one of the lowest underspends at 3%.
As previously discussed, deprivation can have a negative effect on oral health, resulting in teenagers from deprived families becoming twice as likely to experience toothache than their classmates.7 From 2007/2008, Cwm Taf has been one of the most deprived health boards in Wales, yet it has the best access and some of the smallest clawback figures. This is because Cwm Taf is aware of its challenges and has worked to address them.
While the current contract makes it impossible for practitioners to focus on prevention, Cwm Taf has used and created other schemes to support their patients. As well as the community dental services' 'Designed to Smile' programme, which has enjoyed successes such as a falling rate in tooth decay among five-year-olds,8 Cwm Taf runs its own toothbrushing scheme. This scheme employs oral health educators to visit 38 schools in Cwm Taf.9 Now, only 15 schools in Cwm Taf do not participate in a toothbrushing scheme. Tooth decay is an entirely preventable disease and using schemes to educate children on oral health can have a huge impact. Cwm Taf also runs the scheme 'Baby Teeth Do Matter', which sees dental teams working with GP practices to promote the oral health of children, particularly those age 0-2 years and 3-5 years. This scheme has seen an increase of 41.7% of children attending dental appointments in the Merthyr locality.10 There has also been a significant 70.25% increase in children aged 0-2 visiting the dentist.10 This shows that schemes such as those employed by Cwm Taf can help to address the inverse care law and improve access.
Cardiff and Vale Health Board
Cardiff and Vale had the worst access to NHS dentistry. A mere 3% of practices were accepting adult NHS patients in 2017, and only 6% of practices were accepting NHS patients who were 'children up to secondary school age' (up to 16 years of age or 18 years of age if in full-time education). However, 86% of practices were accepting private patients, which was the highest in Wales. During the telephone survey, a practice in Cardiff and Vale Health Board disclosed that they felt they did not have an NHS contract large enough for the area they covered. They had a waiting list of over 300 patients which caused the dentists stress, as they wanted to be able to provide more NHS dental care. They were aware of expansion projects planned for their area and felt that without a larger NHS contract even more people in Cardiff and Vale would not receive NHS general dental care.
Cardiff and Vale has already seen a population increase of 26,241 from 2009 to 2016. In the longer-term, the Welsh Assembly Government study suggests the city's population will grow to 468,200 by the year 2033, from its present level of 330, 500.11 The expansion plan the practice was referring to is the 2012 approved project that will see 45,400 new homes built by 2026, which would give Cardiff a population predicted to top 400,000.12 Cardiff and Vale Health Board would undoubtedly see a vast rise in patients in their area. Yet, they were currently unable to treat the patients already in their care. If the difficulties with access in Cardiff and Vale are not resolved, these will only get worse and yet practices were still experiencing clawback, handback and even contract reduction. In a health board where only two out of 66 practices are accepting new NHS patients, 11 practices experienced clawback in the last three years.
Commentary
Access for new patients
Our research shows that access for new NHS patients has declined significantly in the last few years. In Wales, on average, only 15% of all NHS practices were accepting new adult NHS patients in 2017 and only 28% were accepting new child NHS patients. The Welsh Liberal Democrats Party research showed that, in 2012, 37% of practices were accepting new adult NHS patients.13 However, Kirsty Williams AM found even that level 'astonishing' and 'woeful'.14 In the five years since then, access for new patients has more than halved.
Although access to NHS dentistry is a problem across Wales, the story behind the access figures varies from health board to health board. While practices in Cardiff and Vale Health Board need a larger NHS contract to cover patients in their area, practices in rural Wales are struggling to see patients as they are having trouble recruiting and retaining associates. To address the access problem in Wales, each of the health board's difficulties must be studied individually. Nevertheless, the telephone survey, which covered all the health boards, is likely to be representative of practices across Wales. Of those practices surveyed, 50% of them blamed recruitment and retention as the reason for clawback and thus causing a knock-on effect on access.
Access for children with different needs
This paper has discussed access to NHS dentistry from a variety of different patient classifications, be it children, charge-exempt NHS patients, or adults. However, it is vital to remember that within these classifications are a variety of different patients, with different needs, who have the same right to primary care NHS dentistry. Bhatia and Collard (2012) found that 'many children with cleft lip and/or palate find it difficult or impossible to access NHS primary dental care'.15 They believed that this highlights the shortcomings in the provision of NHS dental care in areas of Wales. Their research showed that 39% of parents of children with cleft lip and/or palate found it difficult or impossible to find an NHS dentist. Evidence has shown that patients with cleft lip and/or palate are at greater risk of developing dental caries compared with the general population.16 The problems created by the limited access to an NHS dentist in Wales are wider than the general population.
Oral health
Most oral health problems such as tooth decay are entirely preventable, but only if patients have the knowledge and ability to care for their oral health. However, the current GDS contract limits dentists' ability to put prevention first. Moreover, dentists are disincentivised to treat those with poor oral health who then suffer. The current UDA system creates problems for dentists and patients, or would-be patients alike.
The Royal College of Paediatrics and Child Health's State of Child Health 2017 report lists access to timely primary dental care as a key health objective.17 The reality is that this objective is currently not possible due to the widespread lack of children's access to NHS general dentistry. Only 28%, on average, of NHS dental practices in Wales are accepting children and a mere 23% are accepting children with learning disabilities. If children cannot access NHS dentistry, then good oral health cannot be achieved and maintained. The State of Child Health 2017 report also states that good oral health is essential for children's overall health and wellbeing. The British Dental Association (BDA) wholeheartedly endorses this viewpoint and is concerned that this connection is poorly understood by politicians and policymakers.
The standard of oral health in Wales lags behind England. The most common reason for a child to attend hospital is to have a dental extraction under general anaesthetic; this is more common than a child being admitted with a broken arm.18 This is stressful for the child, expensive for the public purse, and wholly avoidable. Children need early, regular contact with a dental practice to improve and maintain their oral health.
The 2013 Children's Oral Health Survey found that dental decay was present in 41% of five-year-olds.7 By the age of 12, around half (52%) of children in Wales had obvious decay experience. By the age of 15, the prevalence of obvious decay experience in permanent teeth increased further to 63% of children and 11% of 15-year-old children had teeth missing due to decay.
Deprivation has been shown to have a negative effect on oral health. Children in Wales receiving free school meals aged 12 were 6% more likely to have had toothache in the last three months than those not eligible for free school meals. However, this may not be the full picture. The work of Monahan et al.,19 examined the fact that since 2007/08 positive consent has been required for dental surveys. They found that since this introduction there has been a greatly decreased participation, which is reduced most for children with caries experience. The study concluded that 'because caries is more prevalent in deprived areas, the impact [of positive consent] on participation and d3mft scores is greater there'.19 In other words, it is likely that there is under-reporting in children of a correlation between deprivation and poor oral health. More work needs to be done to examine the correlation between dental health and deprivation, and to ascertain the impact of increasingly limited access to NHS general dentistry.
Contract reform
As previously discussed, dentists are disincentivised in the current UDA-based contract to treat patients with high oral health needs. Treating many patients with poor oral health can mean that, in an area of deprivation and poorer oral health, the practice would likely fail to reach its targets, and subsequently face clawback, handback or contract reduction, and possible closure. Aneurin Bevan has one of the highest levels of deprivation in Wales.7 The impacts of highly reduced access to NHS GDS for new patients, together with the inbuilt health inequalities that the 2006 contract engenders, will have inevitable impacts and outcomes for patients.
The latest Wales Government contract reform project currently sees 10% of practices in Wales in the pilot with a contract reduction of 10% of UDAs for data gathering on oral health needs assessment.20 The Cabinet Secretary for Health and Social Services expects a minimum of 20% of all dental practices in each health board area to be taking part from April 2019, with further expansion planned for October 2019.21 This is a step in the right direction, but until a bigger percentage of the contract can be freed from the vice-like grip of UDAs, this situation is unlikely to materially change. The government has already indicated their direction of travel with skills mix and the aim of increasing numbers of dental care professionals in dental teams. The authors have concerns about the proof of efficacy of the business model when running a chair with fixed overheads, particularly in smaller practices.22
Factors affecting access to NHS dentistry
Despite the considerable evidence of clawback and recruitment and retention problems provided by BDA Wales to the DDRB 2018 review, the commentary from the Review Body on Doctors' and Dentists' Remuneration (DDRB) Board was to ignore this evidence as anecdotal in favour of government figures. These government statistics, however, failed to account for population growth which means that dental activity as a percent of the population has remained stubbornly at 54% of the population of Wales for the last six years or more. That leaves 46% of the population without access to general NHS dentistry and many of those will not be able to afford private treatment. Therefore, there appears to be a lack of political will to recognise this ongoing shortfall in NHS provision.
The evidence presented here suggests that very soon the percentage accessing NHS dentistry is likely to decrease with access now being so low for new patients. In fact, the most recent Welsh Government data for dentistry activity show that the number of treatments actually dropped between 2017 and 2018 by 8,820.23 Moreover, the government figure of 4.7 dentists performing NHS contracts per 100,000 people is misleading. This is a head count figure, not a whole time equivalent (WTE) figure, and more dentists are now working part-time. NHS Digital in 2018 said: 'During the last decade there has been a notable drop in the amount of time dentists spend on clinical work across the UK'.24
The levels of clawback and contract reduction in Wales are unacceptable. In the three years surveyed alone circa £20 million was lost from frontline NHS dental services in Wales. Rather than further investment in dentistry to address the poor access and oral health deficits, every health board's budget is being underspent. While it is recognised that some health boards have reinvested some of the clawback money into specific expenditures for dental practices this does not, however, translate into any more patient appointments.
The effects of 'Brexit' are already being felt across the medical and dental professions, and the greatly reduced influx of dentists from mainland Europe is going to further impact on recruitment and retention of dentists in Wales. It is no coincidence that the corporate practices, which rely heavily on contracting with Eastern European dentists, have been closing significant numbers of practices in England and Wales in the last 12 months. At the time of writing, the corporate practice in Builth Wells was the latest to announce its closure.
Impact on urgent and non-dental services
This access crisis is likely having a negative effect on other NHS services in Wales. Many patients with dental pain are forced to visit their GP. It is estimated that 600,000 GP appointments are made every year in the UK by patients seeking dental care; the estimated cost to the NHS is £26 million a year.25 That translates to an estimated 30,000 GP appointments in Wales, at a cost of £1.3 million.
Publications on this topic have considered that the problem primarily resulted from patients avoiding dental charges or was caused by dental phobia. Many articles referring to these data discussed the patient charges involved in NHS dentistry, but declined to acknowledge the problems with patient access to NHS dentistry, quite possibly due to lack of data hitherto. However, the responses to these articles from members of the public show that the struggle to be seen by an NHS dentist is a significant factor.26 People discuss the pain they have experienced, the inability to even get on a waiting list for an NHS dentist, and the costs of private dentistry as an alternative. This can also be seen in the responses to articles discussing DIY dentistry.27 While patient charge costs were deemed the reason for a rise in DIY dentistry by the author, responses from the public show that difficulty accessing a dentist also plays a substantial part.
While the NHS 111 service is currently being developed to try to address patients accessing A&E and GP services with dental problems, it has yet to be rolled out across Wales. There are currently no data available to show whether the enhanced urgent service is relieving such pressure.
Recommendations
-
1.
More research must be done into the impacts of low levels of access for new patients to NHS dentistry in Wales
-
2.
More research needs to be done to examine the correlation between dental health and deprivation, and to ascertain the impact of restricted access to NHS general dentistry
-
3.
Research is needed to review the effects of population growth on limited NHS dental services
-
4.
Research is needed on the access of GPs and emergency medical services by patients with dental pain and how much of this is related to their inability to access NHS dentistry
-
5.
The NHS 111 dental service data need to be routinely collected and analysed to demonstrate both the efficacy of the system and to provide a proper measure of the service use for urgent versus non-urgent dental needs; and whether it is relieving pressure in non-dental services
-
6.
There needs to be an annual review of access to NHS dentistry, as part of Welsh Government data gathering, and the results should be published on the StatsWales website
-
7.
Health boards as commissioners of these services need to be held accountable by the Welsh Government for the decline in access for new patients to NHS dentistry
-
8.
It is vital that new research is conducted on recruitment and retention in NHS dentistry in Wales and then acted upon. The last systematic review was published in 2012.
Summary
In conclusion, increasingly low levels of access to NHS dentistry in Wales are caused by a number of factors, with each factor more or less prevalent in each health board. It is possible that a rise in private dentistry in certain areas has occurred because NHS dentistry is not financially viable for many practices. It is evident that the pressures of clawback, handback and contract reduction affect many practices in every health board in Wales. As well as the loss of money from the GDS budget, dental practitioners are disincentivised in taking on new patients. Because the state of new patients' oral health is unknown, declining to take them on could potentially avoid hours of work that earn a low UDA value.
If these difficulties are not addressed, NHS dentistry capacity in Wales will continue to decline and access will become an ever larger problem, with inevitable consequences for the country's oral health. The Welsh Government's new contract reform pilot20 could bring about the beginnings of much needed changes, including a reduction in the percentage of UDAs for the contract value and also a minimum UDA value. If these changes are sufficiently amplified in the future, they may slow or even halt this decline. The Welsh Assembly's Committee for Health and Social Care has been conducting an inquiry into dentistry in Wales, including the nature of GDS contract reform, to which the authors extensively contributed.22 Our recommendations here echoed several of those we presented to the committee.
Further research needs to be carried out to help address the many problems caused by the GDS contract. Research must be conducted into patients with dental problems accessing emergency dentistry, GPs and A&E departments. There should be a coordinated needs assessment across Wales to identify the local, regional and national dental health requirements. This intelligence, together with vital new resources, could help shape the future of NHS dentistry in Wales into a fairer and more robust service.
References
Mumsnet. Finding an NHS dentist. 2013. Available at https://www.mumsnet.com/Talk/am_i_being_unreasonable/1864523-Finding-an-NHS-dentist (accessed May 2019).
Mail Online. Why can't you find an NHS dentist? Available at http://www.dailymail.co.uk/health/article-191300/Why-NHS-dentist.html (accessed May 2019).
StatsWales. NHS performers by local health board and dentist type. 2018. Available at https://statswales.gov.wales/Catalogue/Health-and-Social-Care/General-Dental-Services/Current-Contract/nhsperformers-by-localhealthboard-dentisttype (accessed May 2019).
British Dental Association. BDA Survey. 2016.
Dentistry.co.uk. Many dentists facing clawback. 2007. Available at https://www.dentistry.co.uk/2007/11/19/many-dentists-facing-clawback/ (accessed May 2019).
StatsWales. Welsh Index of Multiple Deprivation. 2014. Available at https://statswales.gov.wales/Download/File?fileId=540 (accessed May 2019).
NHS Digital. Children's Dental Health Survey 2013, Country specific report: Wales. 2013. Available at https://files.digital.nhs.uk/publicationimport/pub17xxx/pub17137/cdhs2013-wales-report.pdf (accessed May 2019).
Cardiff University. Designed to Smile: Activity Data: September 2016-July 2017, Monitoring Report. Cardiff: Cardiff University School of Dentistry, 2018. Available at https://gweddill.gov.wales/docs/phhs/publications/designed-to-smile.pdf (accessed May 2019).
Cwm Taf University Health Board. Oral Health Delivery Plan, 2013-2018. 2013. Available at http://www.cwmtafuhb.wales.nhs.uk/sitesplus/documents/865/Oral%20Health%20Delivery%20Plan.pdf (accessed May 2019).
Baby teeth do matter presentation. Dental Symposium, 2018.
Welsh Government. Local authority population projections. 2016. Available at https://gweddill.gov.wales/statistics-and-research/local-authority-population-projections/?lang=en (accessed May 2019).
BBC News. Cardiff expansion: Council backs big growth plan. 2012. Available at https://www.bbc.co.uk/news/uk-wales-20068875 (accessed May 2019).
Welsh Liberal Democrats. Dentistry in Wales: A Wales-wide survey of access to dental care and treatment. 2012. Available at https://d3n8a8pro7vhmx.cloudfront.net/ldwales/pages/962/attachments/original/1444132517/2012_-_Dentistry_Survey.pdf?1444132517 (accessed May 2019).
Wales Online. Six-year waiting list to register with dental practice in Wales. 2012. Available at https://www.walesonline.co.uk/news/wales-news/six-year-waiting-list-register-dental-2046012 (accessed May 2019).
Bhatia S K, Collard M M. Access to primary dental care for cleft lip and palate patients in South Wales. Br Dent J 2012; 212: E10.
Cheng L L, Moor S L, Ho C T. Predisposing factors to dental caries in children with cleft lip and palate: a review and strategies for early prevention. Cleft Palate Craniofac J 2007; 44: 67-72.
Royal College of Paediatrics and Child Health. State of Child Health 3 - Early years indicators. 2017. Available at https://www.rcpch.ac.uk/resources/state-child-health-3-early-years-indicators (accessed May 2019).
NHS Digital. Hospital Admitted Patient Care Activity, 2016-17. 2017. Available at http://digital.nhs.uk/catalogue/PUB30098 (accessed May 2019).
Monahan N P, Jones S J, Morgan M Z. Do parents of children with caries choose to opt out of positive consent dental surveys in Wales? Br Dent J 2011; 210: E1.
NHS Wales. Taking Oral Health Improvement and Dental Services Forward in Wales: A Framework outlining priorities for dentistry and a future work programme. 2017. Available at https://gov.wales/docs/phhs/publications/170815oralhealthen.pdf (accessed May 2019).
Welsh Government. Progress on plans to improve NHS dental services in Wales. 2018. Available at https://gov.wales/newsroom/healthandsocial-services/2018/dental-services/?lang=en (accessed May 2019).
The Welsh Assembly's Health, Social Care and Sport Committee's Inquiry into Dentistry in Wales 2018. Response by the BDA Wales "More than Words". 2018. Available at https://bda.org/about-the-bda/officers-and-contacts/Documents/Wales%20-%20Consultations/Dentistry%20in%20Wales%20BDA%20Wales.pdf (accessed May 2019).
Welsh Government. NHS Dental Statistics in Wales, 2017-2018. 2018. Available at https://gweddill.gov.wales/docs/statistics/2018/180830-nhs-dental-services-2017-18-en.pdf (accessed May 2019).
NHS Digital. Dental Working Hours - 2016/17 and 2017/18: Working Patterns, Motivation and Morale [PAS]. 2018. Available at https://digital.nhs.uk/data-and-information/publications/statistical/dental-working-hours/2016-17-and-2017-18-working-patterns-motivation-and-morale (accessed May 2019).
Smyth C. Toothache patients cost GPs £26m a year. The Times (London) 2016 September 6. Available at https://www.thetimes.co.uk/article/toothache-patients-cost-gps-26m-a-year-7hd9w8f5v (accessed May 2019).
Campbell D. Why are people taking dental complaints to their GP? The Guardian (London) 2016 September 10. Available at https://www.theguardian.com/global/2016/sep/10/why-are-people-taking-dental-complaints-gp-instead-dentist (accessed May 2019).
Johnston L. Now we pull out our own teeth: Boom in DIY dental kits as patients cannot afford NHS fees. Daily Express (London) 2013 May 12. Available at https://www.express.co.uk/life-style/health/399032/Now-we-pull-out-our-own-teeth-Boom-in-DIY-dental-kits-as-patients-cannot-afford-NHS-fees (accessed May 2019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Owen, C., Seddon, C., Clarke, K. et al. NHS general dentistry in Wales: evaluation of patient access and budget expenditure. Br Dent J 226, 967–978 (2019). https://doi.org/10.1038/s41415-019-0407-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0407-3