Abstract
Introduction To determine the reasons why patients are referred requesting removal of third molar teeth.
Method Prospective evaluation of referrals requesting removal of third molar teeth only. Following review of symptoms, clinical, and if appropriate, radiographic findings, a diagnosis according to pre-defined criteria was made, and verified by a senior member of staff.
Results 662 individual referrals were received requesting removal of 1,117 individual third molar teeth, of which 73% were for mandibular teeth. A total of 195 teeth (17.6%) were not removed as there was no disease process or insufficient symptoms. In 124 cases (11.1%) a diagnosis of temporomandibular disorders was made with no dental surgery being required. Other reasons for patients not proceeding to surgery were: no symptoms or sign of disease; symptoms were from an adjacent tooth; only single episode of pericoronitis; late incisor crowding; and cervical sensitivity.
Conclusion While most patients referred did proceed to have removal of third molar teeth, a significant proportion had symptoms related to chronic orofacial pain that would not have been influenced by removal of third molar teeth. The overall incidence of temporomandibular disorders within the patient sample, either as a primary, secondary or tertiary diagnosis was 18.7%.
Similar content being viewed by others
Key points
-
Suggests dental caries is an increasing cause for removal of third molar teeth, followed by pericoronitis.
-
Approximately 18% of patients referred requesting removal of third molar teeth did not require removal of their third molar teeth.
-
Highlights that referring dental practitioners sometimes attribute chronic orofacial pain to disease-free third molar teeth.
Introduction
Few topics in dentistry arouse such passion, personal opinion, and contribution to discussion as the management of third molar teeth. Since the 1980s, there has been continual debate relating to the appropriate management of third molars. Within the United Kingdom, this has resulted in numerous reports and guidelines which still continue to undergo revisions.1,2,3,4 These guidelines have resulted in a change in the demographics of patients undergoing third molar extractions, with a shift to surgery being undertaken later in life.5,6 In particular, discussion continues into the appropriate management of horizontal and mesio-angular impactions, in terms of late stage disease of the second molar relating to dental caries or progressive periodontal bone loss.7,8 In 2016, the American Association of Oral and Maxillofacial Surgeons issued guidelines supportive of best evidence, but also endorsing the role of the surgeon in supporting their patient in making a decision that is in the best interests of the patient.9
Occurring alongside discussions on the appropriate management of third molar teeth has been discourse on the role that third molar teeth, particularly removal of such, have in the aetiology and management of temporomandibular disorders and chronic orofacial pain. Some report that the mechanism of third molar removal is the stimulus for temporomandibular disorders.10,11,12,13 Others have been unable to identify any statistically significant relationship; with no evidence of a direct causal link.14,15,16
Historical analysis of patients waiting for third molar tooth removal shows pain as being the predominant symptom, with some patients having received multiple courses of antibiotics as management.17,18 However, a prospective study performed on patients having third molar teeth removed recorded pain in the absence of signs of disease as being the second most common reason for surgery.19 It has been postulated that, historically, patients underwent third molar removal without sufficient clinical justification and, on reflection, perhaps the patient's symptoms were not related to their third molar teeth?19
This evaluation aimed to determine if the recommended changes in clinical practice, the changing patterns of disease presentation, the increased awareness of chronic orofacial pain diagnosis, and management by general practitioners, are reflected in the referrals made to a secondary care provider.
Method
During a 20-month period from 2016 to 2018, referrals from primary care practitioners to a secondary care oral and maxillofacial surgery service were analysed prospectively as to the reason for referral, the clinical diagnosis and the treatment outcome. The secondary care centre was a district general hospital in Scotland serving a population of 148,000. The Regional Research and Development Support Unit defined the study as an audit/service evaluation, such that ethical approval was not required as no change in treatment planning would result from the evaluation and there was no experimental component.
At consultation, a standardised approach was followed requesting the patient to describe their symptoms rather than relying on the reason for referral given by the referring practitioner. If the patient had no symptoms, the consultation proceeded directly to clinical examination, with radiographic evaluation if indicated, based on the reason for referral in the correspondence from the primary care practitioner.
When pain was the predominant symptom, further questioning led to discussion as to whether or not this was associated with gingival swelling, discharge or bleeding, food impaction or simply pain. When symptoms were of pain only, a standard approach of discussion of pain and any associated symptoms including distribution, functional impact and predisposing psychosocial factors was performed, followed by clinical examination; in keeping with research diagnostic criteria for temporomandibular disorders.20
Diagnostic criteria for dental caries was made by direct clinical and radiographic examination in keeping with the International Caries Detection and Assessment System (ICDAS).21 The radiographic changes occurring with an apical periodontitis were also recorded, although the diagnosis recorded was dental caries, except when there was an apical periodontitis of an adjacent tooth, rather than disease of the third molar.
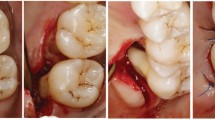
Internationally agreed diagnostic criteria for pericoronitis have not yet been established but are generally agreed to include direct swelling of the soft tissues around the impacted third molar, reported by the patient or observed clinically; and a history of: food packing, bloody or purulent discharge from the soft tissues involving the impacted third molar. Additional diagnostic criteria for pericoronitis include radiographic signs of pericoronal bone loss involving the crown of the impacted third molar tooth, with or without extension onto the distal surface of the adjacent second molar.
All diagnoses and treatment plans were verified by a senior member of staff. Findings were entered in a spreadsheet for data analysis.
Results
During the 20-month period, 662 referrals specifically requesting removal of third molar teeth were received. Data were analysed per individual tooth rather than individual patient as patients often presented with one or more diagnoses, with a different diagnosis for the contra or ipsi-lateral third molar tooth. Rather than analyse multiple diagnoses for an individual patient, the decision was taken to allocate a diagnosis or group of diagnoses per third molar tooth to provide clarity.
The 662 referrals involved requests for the removal of 1,117 individual third molar teeth. Most third molars, 816 (73%), that we were asked to remove were mandibular, with 301 (27%) maxillary. Furthermore, 922 third molar teeth fulfilled criteria as per current guidelines and were removed, 82.5% of all requests.3 Four hundred and sixty-six (41.7%) third molars were removed because of decay alone. An additional 19 (1.7%) third molars were removed because of decay; however, temporomandibular disorder was the primary diagnosis, as the extent of decay observed could not alone account for the symptoms of pain.
A further 288 (25.8%) teeth were removed because of a diagnosis of pericoronitis. In addition, 56 (5.0%) teeth were removed because of pericoronitis, but temporomandibular disorder was the primary diagnosis as pericoronitis alone could not account for the character or distribution of the symptoms of pain. This group included three patients who were initially determined to have temporomandibular disorders only, but were reviewed at six months after the initial diagnosis and proceeded to have third molar teeth removed because of convincing symptoms and signs of pericoronitis.
Sixty (5.4%) teeth were removed because of a combined diagnosis of pericoronitis and dental caries. In addition, ten (0.9%) teeth were removed due to combined symptoms of decay/pericoronitis, with the individual patients also experiencing temporomandibular disorders. In these cases, the extent of decay or the clinical radiographic signs of pericoronitis could not account for the history or nature of the pain experienced by the patient. For those third molar teeth that were removed, 922 (82.5%), temporomandibular disorder was the primary diagnosis in 85 cases (7.6%).
Although there were many horizontally and mesioangular impacted third molar teeth removed because of dental caries and pericoronitis without signs of disease in the adjacent second molar, 71 (6.4%) of third molars were removed because of disease in the adjacent second molar tooth, all of which were mandibular. Caries was the predominant cause in 53 teeth, with periodontal bone loss occurring in eight teeth. There were combined periodontal/endodontic lesions involving the second molar in two instances. Four individual third molar teeth required removal because of dentigerous cyst development.
Of those third molar teeth that did not proceed to removal, 195 (17.6%): 124 (11.1%) were not removed because the primary diagnosis was temporomandibular disorders without any signs or symptoms of disease affecting the third molar teeth. However, within this group, four patients demanded, and subsequently underwent, removal of third molar teeth on the basis of chronic pain; they were insistent that their third molars were the cause, despite no sign of disease being present either before or at the time of surgery. Another three patients that were reviewed six months later did not proceed to surgery on the basis that they had confirmed chronic temporomandibular disorders without third molar disease.
The next group that did not proceed to surgery was patients with 23 individual teeth, 2.1%, with the cause of the patients' symptoms being an adjacent tooth, along with an irreversible pulpitis or demonstrating an apical periodontitis for which the referring dentist had missed and attributed the symptoms to the disease free third molar tooth. Some patients were referred just because they had third molar teeth and had no symptoms or signs of disease (20 teeth, 1.8%).
There was a request for removal of 18 third molar teeth (1.6%) because of a single episode of mild pericoronitis that was not of sufficient severity for the patient to want to undergo surgery. Improvement in oral hygiene was all that was required. Less common referral reasons included late incisor crowding (seven third molars), and cervical sensitivity (three third molars). The cervical sensitivity cases arose from first molars and premolars with exposed dentine, with the mistaken assumption that disease free, impacted third molars would cause acute pulpitic symptoms.
Discussion
This evaluation has demonstrated that when third molar teeth are removed there is often more than one diagnosis for a particular patient. What was of interest to us, and the reason for the evaluation, was the proportion of patients referred that did not require removal of third molar teeth. There was often a misdiagnosis, particularly of orofacial pain, by the referring practitioner. We did experience some resistance from some patients when explaining that they did not require surgery, and the fact that their symptoms of pain were on most occasions of a functional nature, and not related to an organic disease process. There was, on occasion, significant frustration expressed by the patient at the decision not to remove the disease free third molar teeth, but these were often the patients with most psychosocial issues contributing to chronic orofacial pain.
The incidence of temporomandibular disorders in the whole group was 18.7%, either as a primary, secondary or tertiary diagnosis, with 11.1% of patients having their symptoms solely attributable to temporomandibular disorders. Within this group, temporomandibular disorders encompassed myalgia, myofascial pain with referral, headaches attributable to TMD, and disc displacement with and without reduction. Degenerative diseases of the temporomandibular joint were not encountered within the group referred requesting removal of third molar teeth. Some patients had also reported experiencing pain that they, and often their medical and dental practitioners, attributed to chronic paranasal sinus infection. This compares favourably with a 2009 Australian study, in which 23.3% of all patients had some of their symptoms attributable to temporomandibular disorder, with 13.3% of patients having symptoms attributable solely to temporomandibular disorder.22
On a historical basis, some patients have presented with chronic orofacial pain complaining that their symptoms only arose following removal of their third molar teeth. Some will occasionally state that it was the trauma involved in the removal of their third molar teeth, in terms of having their mouth held open during surgery or general anaesthetic airway management that has resulted in them experiencing orofacial pain, with clicking of the temporomandibular joint or intermittent trismus. Considering the incidence of temporomandibular disorder reported in this small study, and the Australian study, it is possible that the primary cause of some of the symptoms of pain that those patients experienced may have been due to temporomandibular disorders rather than third molar disease. This may explain previous reports that the surgical removal of third molar teeth contributes to temporomandibular disorders.10,11,12,13
Listening to patient's symptoms, not those reported by their referring dental practitioner, and identification of clinical signs are of vital importance in reaching a diagnosis before committing the patient to undergoing surgery. Although we have not been able to reliably demonstrate it within this sample, there does appear to be a tendency for some referring dental practitioners to relate the cause of orofacial pain to impacted, even un-erupted third molar teeth without any specific symptoms related to pericoronitis, or clinical and radiographic signs of disease. There appeared to be a tendency for pain as a standalone symptom to be attributed to third molar teeth.
On many occasions it was the patient's description of the nature and distribution of their pain that led to further discussion and the diagnosis of temporomandibular disorders. In some instances, third molar teeth were attributed to causing chronic pre-auricular and zygomatic pain as well as fronto-temporal headaches. Often, patients' used the term that their teeth were being squeezed together or that they were experiencing a pressure-like sensation in their jaws. It appeared to be these descriptions that led the referring dental practitioner to assume that as the symptoms of pain arose in the area of the jaw or teeth, then the third molar teeth must be the cause.
Holding a discussion with patients before surgery the fact that some or most of their symptoms of orofacial pain were not attributable to their third molar teeth allowed the patient to more readily accept that, while there may have been an indication to remove third molar teeth because of disease, the removal of such would not necessarily lead to complete resolution of their symptoms of orofacial pain.
The management of chronic orofacial pain, including temporomandibular disorders, with or without internal derangement, and the psychosocial factors that frequently accompany such, are best discussed before any elective surgery is undertaken. Discussion allows for more effective management of chronic symptoms. Such discussions are also pre-emptive rather than seen as an excuse when discussed post-operatively when the surgeon is often viewed as being defensive of their actions.
For those patients that were referred requesting removal of third molar teeth and were diagnosed as having temporomandibular disorders, there were multiple reports of patients having been prescribed antibiotics, sometimes on multiple occasions, for management of orofacial pain despite no clear history of intraoral swelling, bleeding or discharge. Where extraoral swelling was identified in those patients it was mostly attributable to masseteric hypertrophy rather than infection. This raises concern over the appropriate prescription of antibiotics without pyrexia or clinical signs of spreading infection, despite up to date, high-quality educational and advisory material on this subject.23
When patients were informed that they did not require removal of their impacted third molar teeth, or that their symptoms were of another origin, they were informed that should symptoms or signs of disease directly attributable to their third molar teeth arise at a later date, they would be reassessed and, if appropriate, surgery would be discussed. The purpose of the evaluation was to determine the proportion of correct diagnoses and treatment planning at the time of referral, not make a lifetime prediction of the risk of developing disease directly attributable to third molar teeth at a later date.
Conclusion
Approximately one in five patients referred requesting removal of third molar teeth did not require removal of such. This has implications for the provision of oral surgical services which are increasingly being provided in the primary healthcare setting; often on a direct access, single-visit appointment. Unless time is allowed pre-operatively to confirm the diagnosis, and discuss such with the patient there is a risk that third molar surgery may be undertaken unnecessarily, without resolution of the patient's symptoms of pain. The proportion of misdiagnosis of chronic orofacial pain in the presence of disease-free third molar teeth and the small proportion of cases where obvious dental disease from another source was missed, as well as the inappropriate prescription of antibiotics for non-infective chronic orofacial pain, emphasises the need for continuing education of primary care dental practitioners.
References
The Faculty of Dental Surgery. Current Clinical Practice and Parameters of Care: The Management of Patients with Third Molar (syn: Wisdom) Teeth. 1997. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/3rdmolar.pdf (accessed March 2019).
Scottish Intercollegiate Guideline Network. Management of unerupted and impacted third molar teeth. A National clinical guideline - SIGN 43. 2000. Available at https://www.scottishdental.org/library/management-of-unerupted-and-impacted-third-molar-teeth/ (accessed March 2019).
National Institute for Health and Care Excellence. Guidance on the Extraction of Wisdom Teeth. 2000. Available at https://www.nice.org.uk/guidance/ta1 (accessed March 2019).
Song F, O'Meara S, Wilson P, Golder S, Kleijnen J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technol Assess 2000; 4: 1-55.
McArdle L W, Renton T. The effect of NICE guidelines on the management of third molar teeth. Br Dent J 2012; 213: E8.
Renton T. Al-Haboubi M, Pau A, Shepherd J, Gallagher J E. What has been the United Kingdom's experience with the retention of third molars. J Oral Maxillofac Surg 2012; 70 (Spec Iss): S48-S57.
Ghaeminia H, Perry J, Neinhuijs M E et al. Surgical removal verses retention for the management of asymptomatic disease free impacted wisdom teeth. Cochrane Database Syst Rev 2016, 8: CD003879.
Toedtling V, Coulthard P, Thackray G. Distal caries of the second molar in the presence of a mandibular third molar - a prevention protocol. Br Dent J 2016; 221: 297-302.
American Association of Oral and Maxillofacial Surgeons. White Paper: Management of Third Molar Teeth. 2016. Available at https://www.aaoms.org/docs/govt_affairs/advocacy_white_papers/management_third_molar_white_paper.pdf (accessed March 2019).
Huang G J, LeResche L, Critchlow C W, Martin M D, Drangsholt M T. Risk factors for diagnostic subgroups of painful temporomandibular disorders (TMD). J Dent Res 2002; 81: 284-288.
Huang G J, Rue T C. Third molar extraction as a risk factor for temporomandibular disorder. J Am Dent Assoc 2006; 137: 1547-1554.
Akhter R, Hassan N M, Ohkubo R, Tsukazaki T, Aida J, Morita M. The relationship between jaw injury, third molar removal, and orthodontic treatment and TMD symptoms in university students in Japan. J Orofac Pain 2008; 22: 50-56.
Barbosa C, Gavinha S, Soares T, Manso M C. Coincidence and awareness of the relationship between temporomandibular disorders and jaw injury, orthodontic treatment, and third removal in university students. J Oral Facial Pain Headache 2016; 30: 221-227.
Juhl G I, Jensen T S, Norholt S E, Svensson P. Incidence and symptoms of signs of TMD following third molar surgery: a controlled prospective study. J Oral Rehabil 2009; 36: 199-209.
MacFarlane T V, Blinkhorn A S, Stevenson L J, Coulthard P. Third molar removal and orofacial Pain: a population based survey. J Oral Maxillofac Res 2010; 1: e4.
Widmer C G. Third molar extraction may increase relative risk for temporomandibular disorders. J Evid Based Dent Pract 2008; 8: 40-42.
Punwutikorn J, Waikakul A, Ochareon P. Symptoms of unerupted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87: 305-310.
Samsudin A R, Mason D A. Symptoms from impacted wisdom teeth. Br J Oral Maxillofac Surg 1994; 32: 380-383.
Lopes V, Mumenya R, Feinmann C, Harris M. Third molar surgery: an audit of the indications for surgery, post-operative complaints and patient satisfaction. Br J Oral Maxillofac Surg 1995; 33: 33-35.
Schiffman E, Ohrbach R, Truelove E et al. Diagnostic Criteria for Temporomandibular disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 2014; 28: 6-27.
Shivakumar K, Prasad S, Chandu G. International Caries and Detection System: A new paradigm in detection of dental caries. J Conserv Dent 2009; 12: 10-16.
DeAngelis A F, Chambers I G, Hall G M. Temporomandibular joint disorders in patients referred for third molar extraction. Aust Dent J 2009; 54: 323-325.
Scottish Dental Clinical Effectiveness Programme. Drug Prescribing for Dentistry. 3rd ed. Dundee: SDCEP, 2016.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mackie, L., Wong-McDermott, R. & Bell, G. An evaluation of referrals requesting third molar tooth removal: clinical diagnosis and treatment outcome. Br Dent J 226, 577–580 (2019). https://doi.org/10.1038/s41415-019-0199-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0199-5