Abstract
Objectives The aim of this article is to present an easy to use, conservative method for managing discolouration in enamel in general practice.
Materials and methods Microabrasion was used in this case to remove superficial layers of discoloured enamel utilising abrasive acids, which was further improved by using ICON, a newly developed resin infiltrant.
Results Significant improvement shown by the presented case suggests that this modality of treatment could be used more frequently.
Discussion This simple yet extremely effective treatment can be used by the general dental practitioner despite not having the necessary equipment as readily available alternatives can be used.
Conclusion Using minimally invasive options in managing superficial enamel lesions can be effective and prevent the use of invasive procedures in the first instance.
Similar content being viewed by others
Key points
-
Demonstrates techniques for managing discoloured enamel defects without the use of invasive methods.
-
Explores new resin infiltrant techniques to further improve the aesthetic appearances of enamel opacities.
-
Gives step-by-step instructions on how to incorporate these techniques into general clinical practice.
Introduction
Children with enamel staining and discolouration frequently present to the general dental practitioner. The aetiology of enamel discolouration can vary and commonly results in aesthetic concerns. It can occur due to staining from extrinsic sources such as coffee, tea and tobacco, whereas other causes can be of intrinsic aetiology. Intrinsic staining may be congenital for example, amelogenesis imperfecta, or acquired, such as tetracycline staining and pathology to primary predecessors.
In the past, colour anomalies were restored using direct or indirect restorative materials that produced satisfactory aesthetic results. However, these restorations required long-term repair and replacement which resulted in the tooth entering the restorative cycle.1 The microabrasion technique was introduced by Croll and Cavanaugh, who proposed the utilisation of 18% hydrochloric acid along with pumice to improve brown enamel lesions.2 Eventually, this was developed into a non-invasive, simple technique called 'enamel microabrasion'. This technique removes superficial and intrinsic defects from teeth with minimal tissue loss.3
Enamel microabrasion works by simultaneous abrasion and erosion, bringing about an 'abrosion' effect. The technique involves removing the porous surface of enamel, along with any staining, by mechanical application of a combination of acid gel and an abrasive compound.1 A prismless and dense layer also forms as an intrinsic portion of the enamel and it reflects and refracts light in such a way that mild colour imperfections in the underlying enamel can be camouflaged.4
Case report
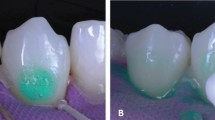
A case of a nine-year-old girl with enamel discolouration of the maxillary right central incisor is reported. The patient came with her mother complaining of the 'brown colour' on her tooth (Fig. 1) which was affecting her confidence.
Clinical examination of the patient revealed:
-
A permanent dentition which was clinically caries free
-
A class II division 2 malocclusion with crowding in the upper and lower labial segments
-
A well-demarcated brown lesion on the labial surface of the 11.
Enamel microabrasion
Method
-
1.
Place a rubber dam to isolate the tooth, in this case a dry dam was used
-
2.
Clean the tooth before treatment using prophy paste and a rubber cup
-
3.
Dry the tooth and the surrounding mucosa
-
4.
Apply 37.5% phosphoric acid onto the tooth covering the full surface of the enamel defect and leave for one minute
-
5.
Wash and dry the tooth
-
6.
Using a rubber cup, apply pumice to the enamel defect continuously for one minute
-
7.
Wash and dry the tooth
-
8.
Repeat steps four to seven, two more times
-
9.
Post-treatment fluoride varnish is applied.
Step 1 is shown in Figure 2, Step 4 is shown in Figures 3 and 4, Step 5 is shown in Figures 5 and 6 and Step 6 is shown in Figure 7.
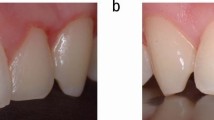
This marks the end of cycle one. The treatment showed significant improvement on the first visit (Fig. 8). However, there was still improvement to be made; therefore, cycle two and cycle three were completed with one-month intervals. A resin infiltrant (ICON) was used in this case to further enhance the appearance of the white patch that remained post-microabrasion (Fig. 11).
Discussion
In many cases, diagnosing the cause of staining can pose challenges. This is particularly so when staining is of intrinsic aetiology. For example, there is often insufficient information from the history to determine whether a child has ingested high amounts of fluoride in the past to verify fluorosis. Trauma to primary teeth can cause developmental disturbances, with the most frequent malformation being enamel hypoplasia, including enamel discolouration, also known as 'Turner's tooth'.
Microabrasion is a simple technique which conserves tooth tissue and can prevent restorative intervention on the tooth. It is often disregarded, as many practitioners are unaware of the significant aesthetic results that can be achieved. It is also inexpensive, making it a viable treatment option for most dental practices. Croll and Cavanaugh suggested removing dental enamel stains by applying 18% hydrochloric acid. Over the years, the development of the acid and the clinical technique has been ongoing to acquire an ideal acid mixture for improved oral soft tissue safety.4 Croll evaluated many acids with different concentrations, such as hydrochloric acid, citric acid, phosphoric acid and nitric acid, with a variety of different abrasive particles to determine the more successful and safer options to use for dental microabrasion.1
Many safe combinations of acid and abrasive particles have been developed and marketed, such as 'Opalustre' which is a pre-mixed version of 6.6% hydrochloric acid slurry and silicon carbide microparticles.1 Opalustre may be more easily applied due to the single agent used, rather than using the 37.5% phosphoric acid and pumice that was used in the case mentioned above (see Fig. 9). Other alternative techniques include mixing the phosphoric acid and pumice before application.Figure 3 shows the use of a microbrush for the application of the acid etch which can be exchanged for a broken wooden stick, such as a tongue depressor, depending on availability and operator choice.
It is essential that the tooth undergoing the procedure is isolated to prevent damage to the adjacent soft tissues by the acid and to ensure the tooth is dry for optimum results. In the case above, a dry-dam was used, however it is more common to have a rubber dam in most dental practices which can of course be substituted instead. As the procedure involves the use of strong acids, it is imperative for both the patient and operators to wear full personal protection equipment throughout the treatment.
Depending on the degree of the discolouration remaining after the first cycle, microabrasion can be repeated after a few weeks. On many occasions, the brown discolouration can be completely eliminated but a white 'patch' may be left behind, as shown in Figure 10. Although this is a significant improvement for patients, the patient may not be completely satisfied with the microabrasion alone, as in this case. Another conservative approach was explored, to further better the results without the use of destructive methods. A resin infiltration technique, such as ICON, can be used after maximum improvement has been achieved with microabrasion to reduce the prominence of white lesions (Fig. 11).5 This works by using new light-polymerised resins to infiltrate the microporosities created by an acid. Its use is indicated for 'white spots' on smooth surfaces that are limited to enamel. Cavitated enamel and deep-seated lesions are contraindicated. ICON is composed of three tubes: Icon-Etch, Icon-Dry and Icon-Infiltrant, all of which come with easy to use instructions. Care must be taken when using Icon-Etch, as it can cause the patient pain if used on dentine lesions.
It is important to note, microabrasion and resin infiltration techniques can be used side-by-side to achieve drastic improvements when removing discoloured lesions without entering the tooth into the permanent restorative sequence. If microabrasion does not completely remove the discolouration then alternative methods can be used such as external/internal bleaching, direct composite restorations, veneers and crowns. Indirect restorations can be destructive to tooth tissue; thus, it is more beneficial to carry out microabrasion techniques before the use of any of the more destructive methods.
Summary
Advantages of microabrasion
-
Safe and practical
-
Quick
-
Less destructive than its alternative treatment (restorative intervention)
-
Reduces plaque adhesion
-
Local analgesia is not required
-
Good aesthetic outcome
-
No significant postoperative sensitivity.
Contraindications for microabrasion
-
Uncooperative patients
-
Patients with a history of sensitivity to hot, cold or acidic foods
-
Not recommended for patients with hypoplastic lesions such as amelogenesis imperfecta and should not be used for dentinogenesis imperfecta.
Indications for microabrasion
-
White and brown spots and bands caused by fluorosis
-
Decalcification defects (often seen after removal of orthodontic brackets).
References
Sundfeld R H, Croll T P, Briso A L, de Alexandre R S, Sundfeld Neto D. Considerations about enamel microabrasion after 18 years. Am J Dent 2007; 20: 67-72.
Pini N I, Sundfeld-Neto D, Aguiar F H et al. Enamel microabrasion: an overview of clinical and scientific considerations. World J Clin Cases. 2015; 3: 34-41.
Deshpande A N, Joshi N H, Pradhan N R, Raol R Y. Microabrasion-remineralization (MAb-Re): An innovative approach for dental fluorosis. J Indian Soc Pedod Prev Dent 2017; 35: 384-387.
Donly K, O'Neill M, Croll T P. Enamel microabrasion: a microscopic evaluation of the "abrosion effect". Quintessence Int 1992; 23: 175-179.
Lee J H, Kim D G, Park C J, Cho L R. Minimally invasive treatment for esthetic enhancement of white spot lesion in adjacent tooth. J Adv Prosthodont 2013; 5: 359-363.
Elkhazindar M M, Welbury R R. Enamel microabrasion. Dent Update 2000; 27: 194-196.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ashfaq, N., Grindrod, M. & Barry, S. A discoloured anterior tooth: enamel microabrasion. Br Dent J 226, 486–489 (2019). https://doi.org/10.1038/s41415-019-0152-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0152-7