Abstract
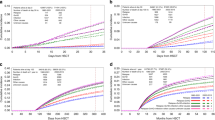
We previously analyzed trends in incidence and factors associated with lethal complications in ALL/AML/CML patients (causes of deaths; COD-1 study). The objective of this study was the analysis of incidence and specific causes of death after HCT, with focus on infectious deaths in two time periods, 1980–2001 (cohort-1) and 2002–2015 (cohort-2). All patients with HCT for lymphoma, plasma cell disorders, chronic leukemia (except CML), myelodysplastic/myeloproliferative disorders, registered in the EBMT-ProMISe-database were included (n = 232,618) (COD-2 study). Results were compared to those in the ALL/AML/CML COD-1 study. Mortality from bacterial, viral, fungal, and parasitic infections decreased in very early, early and intermediate phases. In the late phase, mortality from bacterial infections increased, while mortality from fungal, viral, or unknown infectious etiology did not change. This pattern was similar for allo- and auto-HCT in COD-1 and COD-2 studies, with a distinct and constant lower incidence of all types of infections at all phases, after auto-HCT. In conclusion, infections were the main cause of death before day +100, followed by relapse. Mortality from infectious deaths significantly decreased, except late phase. Post-transplant mortality has significantly decreased in all phases, from all causes after auto-HCT; it has decreased in all phases after allo-HCT except late phase.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Styczynski J, Tridello G, Koster L, Iacobelli S, van Biezen A, van der Werf S. et al. Death after hematopoietic stem cell transplantation: changes over calendar year time, infections and associated factors. Bone Marrow Transpl. 2020;55:126–36. https://doi.org/10.1038/s41409-019-0624-z.
Holmqvist AS, Chen Y, Wu J, Battles K, Francisco L, Hageman L. et al. Late Mortality after Allogeneic Bone Marrow Transplantation in Childhood for Bone Marrow Failure Syndromes and Severe Aplastic Anemia. Biol Blood Marrow Transpl. 2019;25:749–55. https://doi.org/10.1016/j.bbmt.2018.12.063.
Norkin M, Shaw BE, Brazauskas R, Tecca HR, Leather HL, Gea-Banacloche J. et al. Characteristics of Late Fatal Infections after Allogeneic Hematopoietic Cell Transplantation. Biol Blood Marrow Transpl. 2019;25:362–8. https://doi.org/10.1016/j.bbmt.2018.09.031.
Gratwohl A, Brand R, Frassoni F, Rocha V, Niederwieser D, Reusser P. et al. Cause of death after allogeneic haematopoietic stem cell transplantation (HSCT) in early leukaemias: an EBMT analysis of lethal infectious complications and changes over calendar time. Bone Marrow Transpl. 2005;36:757–69. https://doi.org/10.1038/sj.bmt.1705140.
Hahn T, Sucheston-Campbell LE, Preus L, Zhu X, Hansen JA, Martin PJ. et al. Establishment of Definitions and Review Process for Consistent Adjudication of Cause-specific Mortality after Allogeneic Unrelated-donor Hematopoietic Cell Transplantation. Biol Blood Marrow Transpl. 2015;21:1679–86. https://doi.org/10.1016/j.bbmt.2015.05.019.
Copelan E, Casper JT, Carter SL, van Burik JA, Hurd D, Mendizabal AM. et al. A scheme for defining cause of death and its application in the T cell depletion trial. Biol Blood Marrow Transpl. 2007;13:1469–76. https://doi.org/10.1016/j.bbmt.2007.08.047.
Gratwohl A, Sureda A, Cornelissen J, Apperley J, Dreger P, Duarte R. et al. Alloreactivity: the Janus-face of hematopoietic stem cell transplantation. Leukemia. 2017;31:1752–9. https://doi.org/10.1038/leu.2017.79.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304.
Gratwohl A, Sureda A, Baldomero H, Gratwohl M, Dreger P, Kröger N, et al. Economics and Outcome After Hematopoietic StemCell Transplantation: A Retrospective Cohort Study. EBioMedicine. 2015;2:2101–9.
Iacobelli S. Suggestions on the use of statistical methodologies in studies of the European Group for Blood and Marrow Transplantation. Bone Marrow Transpl. 2013;48:S1–37. https://doi.org/10.1038/bmt.2012.282.
Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. New York: Springer-Verlag; 2003.
Gratwohl A, Pasquini MC, Aljurf M, Atsuta Y, Baldomero H, Foeken L. et al. One million haemopoietic stem-cell transplants: a retrospective observational study. Lancet Haematol. 2015;2:e91–100. https://doi.org/10.1016/S2352-3026(15)00028-9.
Niederwieser D, Baldomero H, Bazuaye N, Bupp C, Chaudhri N, Corbacioglu S. et al. One and a half million hematopoietic stem cell transplants: continuous and differential improvement in worldwide access with the use of non-identical family donors. Haematologica. 2022;107:1045–53. https://doi.org/10.3324/haematol.2021.279189.
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M. et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N. Engl J Med. 2010;363:2091–101. https://doi.org/10.1056/NEJMoa1004383.
Meyers JD, Bowden RA, Counts GW. Infectious complications of marrow transplant: risk factors for infection. Prog Clin Biol Res. 1989;309:357–66.
Styczynski J, Piekarska A, Zaucha-Prażmo A, Zaucha JM, Zając-Spychała O, Wróbel T. et al. Antimicrobial prophylaxis in adults and children undergoing hematopoietic cell transplantation: 2021 Polish recommendations. Acta Haematol Pol. 2021;52:528–42. https://doi.org/10.5603/AHP.a2021.0097.
Gratwohl A, Brand R, McGrath E, van Biezen A, Sureda A, Ljungman P. et al. Use of the quality management system “JACIE” and outcome after hematopoietic stem cell transplantation. Haematologica. 2014;99:908–15. https://doi.org/10.3324/haematol.2013.096461.
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF. et al. Letermovir Prophylaxis for Cytomegalovirus in Hematopoietic-Cell Transplantation. N. Engl J Med. 2017;377:2433–44. https://doi.org/10.1056/NEJMoa1706640.
Acknowledgements
The authors acknowledge the cooperation of the participating teams and their staff. They acknowledge the excellent work of the EBMT and IDWP Leiden Study Unit.
Author information
Authors and Affiliations
Contributions
JSt and GT designed the study and drafted the manuscript. LK, AvB, SvW, and HB were responsible for the data collection and assembly. GT conducted the statistical analysis. MM, LG, CC, PL, DA, SC, CC, SCo, HD, BG, RG, NK, RPL, MM, BN, ZP, JAS, AS, IYA, and RC were responsible for the integrity of the data and gave scientific input. All authors have seen and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Styczynski, J., Tridello, G., Koster, L. et al. Decrease of lethal infectious complications in the context of causes of death (COD) after hematopoietic cell transplantation: COD-2 and COD-1 study of the Infectious Diseases Working Party EBMT. Bone Marrow Transplant 58, 881–892 (2023). https://doi.org/10.1038/s41409-023-01998-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01998-2