Abstract
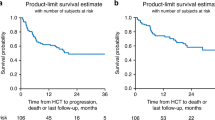
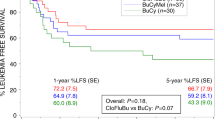
In adults with acute lymphoblastic leukemia (ALL), post-transplant relapse is a major risk factor for mortality after allogeneic hematopoietic stem cell transplantation (allo-HSCT). Our study investigated the efficacy and safety of decitabine (dec) with ALL patients post-transplantation. We performed a retrospective cohort study to assess the efficacy of decitabine (dec) with post-transplant ALL at the First Affiliated Hospital of Zhengzhou University from February 2016 to September 2021. A total of 141 consecutive ALL patients were analyzed and divided into decitabine (dec, n = 65) and control (ctrl, n = 76) groups based on whether they were treated with decitabine after allo-HSCT. The 3-year cumulative incidence of relapse (CIR) rate in the dec group was lower than that in the ctrl group (19.6 vs. 36.1%, p = 0.031), with a hazard ratio of 0.491 (95% confidence interval [CI], 0.257–0.936). Additionally, subgroup analyses revealed that the 3-year CIR rate of T-ALL and Ph-negative B-ALL patients in the dec and ctrl groups was 11.7 vs. 35.9% and 19.5 vs. 42.2% (p = 0.035, p = 0.068) respectively. In summary, ALL patients, especially those with T-ALL and Ph-negative B-ALL, may benefit from decitabine as maintenance therapy following allo-HSCT.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
References
Poon LM, Hamdi A, Saliba R, Rondon G, Ledesma C, Kendrick M, et al. Outcomes of adults with acute lymphoblastic leukemia relapsing after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19:1059–64. https://doi.org/10.1016/j.bbmt.2013.04.014.
Kumar AJ, Vassilev P, Loren AW, Luger SM, Reshef R, Gill S, et al. Time to unrelated donor leukocyte infusion is longer, but incidence of GVHD and overall survival are similar for recipients of unrelated DLI compared to matched sibling DLI. Am J Hematol. 2016;91:426–9. https://doi.org/10.1002/ajh.24308.
Pan J, Zuo S, Deng B, Xu X, Li C, Zheng Q, et al. Sequential CD19-22 CAR T therapy induces sustained remission in children with r/r B-ALL. Blood. 2020;135:387–91. https://doi.org/10.1182/blood.2019003293.
Toffalori C, Zito L, Gambacorta V, Riba M, Oliveira G, Bucci G, et al. Immune signature drives leukemia escape and relapse after hematopoietic cell transplantation. Nat Med. 2019;25:603–11. https://doi.org/10.1038/s41591-019-0400-z.
Christopher MJ, Petti AA, Rettig MP, Miller CA, Chendamarai E, Duncavage EJ, et al. Immune escape of relapsed AML cells after allogeneic transplantation. N Engl J Med. 2018;379:2330–41. https://doi.org/10.1056/NEJMoa1808777.
Wright KL, Ting JP. Epigenetic regulation of MHC-II and CIITA genes. Trends Immunol. 2006;27:405–12. https://doi.org/10.1016/j.it.2006.07.007.
Holling TM, Schooten E, Langerak AW, van den Elsen PJ. Regulation of MHC class II expression in human T-cell malignancies. Blood. 2004;103:1438–44. https://doi.org/10.1182/blood-2003-05-1491.
Figueroa ME, Chen SC, Andersson AK, Phillips LA, Li Y, Sotzen J, et al. Integrated genetic and epigenetic analysis of childhood acute lymphoblastic leukemia. J Clin Invest. 2013;123:3099–111. https://doi.org/10.1172/jci66203.
Dunwell TL, Hesson LB, Pavlova T, Zabarovska V, Kashuba V, Catchpoole D, et al. Epigenetic analysis of childhood acute lymphoblastic leukemia. Epigenetics. 2009;4:185–93. https://doi.org/10.4161/epi.4.3.8752.
Chatterton Z, Morenos L, Mechinaud F, Ashley DM, Craig JM, Sexton-Oates A, et al. Epigenetic deregulation in pediatric acute lymphoblastic leukemia. Epigenetics. 2014;9:459–67. https://doi.org/10.4161/epi.27585.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127:2391–405. https://doi.org/10.1182/blood-2016-03-643544.
Huguet F, Leguay T, Raffoux E, Thomas X, Beldjord K, Delabesse E, et al. Pediatric-inspired therapy in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia: the GRAALL-2003 study. J Clin Oncol. 2009;27:911–8. https://doi.org/10.1200/jco.2008.18.6916.
Brown PA, Shah B, Advani A, Aoun P, Boyer MW, Burke PW, et al. Acute lymphoblastic leukemia, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19:1079–109. https://doi.org/10.6004/jnccn.2021.0042.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17. https://doi.org/10.1016/0002-9343(80)90380-0.
Wong IH, Ng MH, Huang DP, Lee JC. Aberrant p15 promoter methylation in adult and childhood acute leukemias of nearly all morphologic subtypes: potential prognostic implications. Blood. 2000;95:1942–9.
Shen L, Toyota M, Kondo Y, Obata T, Daniel S, Pierce S, et al. Aberrant DNA methylation of p57KIP2 identifies a cell-cycle regulatory pathway with prognostic impact in adult acute lymphocytic leukemia. Blood. 2003;101:4131–6. https://doi.org/10.1182/blood-2002-08-2466.
Mai H, Liu X, Chen Y, Li C, Cao L, Chen X, et al. Hypermethylation of p15 gene associated with an inferior poor long-term outcome in childhood acute lymphoblastic leukemia. J Cancer Res Clin Oncol. 2016;142:497–504. https://doi.org/10.1007/s00432-015-2063-6.
Jiang D, Hong Q, Shen Y, Xu Y, Zhu H, Li Y, et al. The diagnostic value of DNA methylation in leukemia: a systematic review and meta-analysis. PLoS ONE. 2014;9:e96822. https://doi.org/10.1371/journal.pone.0096822.
Peirs S, Van der Meulen J, Van de Walle I, Taghon T, Speleman F, Poppe B, et al. Epigenetics in T-cell acute lymphoblastic leukemia. Immunol Rev. 2015;263:50–67. https://doi.org/10.1111/imr.12237.
Huether R, Dong L, Chen X, Wu G, Parker M, Wei L, et al. The landscape of somatic mutations in epigenetic regulators across 1,000 paediatric cancer genomes. Nat Commun. 2014;5:3630. https://doi.org/10.1038/ncomms4630.
Benton CB, Thomas DA, Yang H, Ravandi F, Rytting M, O’Brien S, et al. Safety and clinical activity of 5-aza-2’-deoxycytidine (decitabine) with or without Hyper-CVAD in relapsed/refractory acute lymphocytic leukaemia. Br J Haematol. 2014;167:356–65. https://doi.org/10.1111/bjh.13050.
Agirre X, Novo FJ, Calasanz MJ, Larráyoz MJ, Lahortiga I, Valgañón M, et al. TP53 is frequently altered by methylation, mutation, and/or deletion in acute lymphoblastic leukaemia. Mol Carcinog. 2003;38:201–8. https://doi.org/10.1002/mc.10159.
Zhang G, Gao X, Zhao X, Wu H, Yan M, Li Y, et al. Decitabine inhibits the proliferation of human T-cell acute lymphoblastic leukemia molt4 cells and promotes apoptosis partly by regulating the PI3K/AKT/mTOR pathway. Oncol Lett. 2021;21:340. https://doi.org/10.3892/ol.2021.12601.
Lu BY, Thanawala SU, Zochowski KC, Burke MJ, Carroll WL, Bhatla T. Decitabine enhances chemosensitivity of early T-cell precursor-acute lymphoblastic leukemia cell lines and patient-derived samples. Leuk Lymphoma. 2016;57:1938–41. https://doi.org/10.3109/10428194.2015.1110747.
Kong J, Chen N, Li M, Zhang J, Wu X, Zong L, et al. Venetoclax and decitabine in refractory TP53-mutated early T-cell precursor acute lymphoblastic leukemia. Ann Hematol. 2022;101:697–9. https://doi.org/10.1007/s00277-021-04530-y.
El Chaer F, Holtzman N, Binder E, Porter NC, Singh ZN, Koka M, et al. Durable remission with salvage decitabine and donor lymphocyte infusion (DLI) for relapsed early T-cell precursor ALL. Bone Marrow Transplant. 2017;52:1583–84. https://doi.org/10.1038/bmt.2017.191.
Rahmat LT, Nguyen A, Abdulhaq H, Prakash S, Logan AC, Mannis GN. Venetoclax in combination with decitabine for relapsed T-cell acute lymphoblastic leukemia after allogeneic hematopoietic cell transplant. Case Rep Hematol. 2018;2018:6092646. https://doi.org/10.1155/2018/6092646.
Baig MU, Rytting M, Roth M, Morani AC, Nunez C, Lin P, et al. Venetoclax and decitabine in pediatric refractory T-cell lymphoblastic lymphoma. J Pediatr Hematol Oncol. 2021;43:e991–96. https://doi.org/10.1097/mph.0000000000002050.
Liu J, Jiang ZX, Xie XS, Wan DM, Cao WJ, Wang M, et al. Maintenance treatment with low-dose decitabine after allogeneic hematopoietic cell transplantation in patients with adult acute lymphoblastic leukemia. Front Oncol. 2021;11:710545. https://doi.org/10.3389/fonc.2021.710545.
Hoshino K, Quintás-Cardama A, Yang H, Sanchez-Gonzalez B, Garcia-Manero G. Aberrant DNA methylation of the Src kinase Hck, but not of Lyn, in Philadelphia chromosome negative acute lymphocytic leukemia. Leukemia. 2007;21:906–11. https://doi.org/10.1038/sj.leu.2404615.
Bassan R, Spinelli O, Oldani E, Intermesoli T, Tosi M, Peruta B, et al. Improved risk classification for risk-specific therapy based on the molecular study of minimal residual disease (MRD) in adult acute lymphoblastic leukemia (ALL). Blood. 2009;113:4153–62. https://doi.org/10.1182/blood-2008-11-185132.
Brüggemann M, Raff T, Flohr T, Gökbuget N, Nakao M, Droese J, et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood. 2006;107:1116–23. https://doi.org/10.1182/blood-2005-07-2708.
Holowiecki J, Krawczyk-Kulis M, Giebel S, Jagoda K, Stella-Holowiecka B, Piatkowska-Jakubas B, et al. Status of minimal residual disease after induction predicts outcome in both standard and high-risk Ph-negative adult acute lymphoblastic leukaemia. The Polish Adult Leukemia Group ALL 4-2002 MRD Study. Br J Haematol. 2008;142:227–37. https://doi.org/10.1111/j.1365-2141.2008.07185.x.
Mortuza FY, Papaioannou M, Moreira IM, Coyle LA, Gameiro P, Gandini D, et al. Minimal residual disease tests provide an independent predictor of clinical outcome in adult acute lymphoblastic leukemia. J Clin Oncol. 2002;20:1094–104. https://doi.org/10.1200/jco.2002.20.4.1094.
Vidriales MB, Pérez JJ, López-Berges MC, Gutiérrez N, Ciudad J, Lucio P, et al. Minimal residual disease in adolescent (older than 14 years) and adult acute lymphoblastic leukemias: early immunophenotypic evaluation has high clinical value. Blood. 2003;101:4695–700. https://doi.org/10.1182/blood-2002-08-2613.
Zhao YL, Liu DY, Sun RJ, Zhang JP, Zhou JR, Wei ZJ, et al. Integrating CAR T-cell therapy and transplantation: comparisons of safety and long-term efficacy of allogeneic hematopoietic stem cell transplantation after CAR T-cell or chemotherapy-based complete remission in B-cell acute lymphoblastic leukemia. Front Immunol. 2021;12:605766. https://doi.org/10.3389/fimmu.2021.605766.
Gao L, Zhang Y, Wang S, Kong P, Su Y, Hu J, et al. Effect of rhG-CSF combined with decitabine prophylaxis on relapse of patients with high-risk MRD-negative AML after HSCT: an open-label, multicenter, randomized controlled trial. J Clin Oncol. 2020;38:4249–59. https://doi.org/10.1200/jco.19.03277.
Del Papa B, Ruggeri L, Urbani E, Baldoni S, Cecchini D, Zei T, et al. Clinical-grade-expanded regulatory T cells prevent graft-versus-host disease while allowing a powerful T cell-dependent graft-versus-leukemia effect in murine models. Biol Blood Marrow Transplant. 2017;23:1847–51. https://doi.org/10.1016/j.bbmt.2017.07.009.
Acknowledgements
This work was supported by Natural Science Foundation of Henan Province (182300410301), Medical Science and Technology Research Project of Henan Province (SBGJ202102147, SBGJ202003036, 2018020118), Science and Technology Plan of Henan Province (182102310160), Project of Higher Education of Henan Province (18A320050).
Author information
Authors and Affiliations
Contributions
RG, FH and YS designed the protocol. JF, RL and JZ searched databases and drafted the manuscript. JF and XG carried out the statistical analysis. JF and RL revised the final manuscript. All authors critically reviewed and provided final approval for submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, J., Lu, R., Zhu, J. et al. Effects of post-transplant maintenance therapy with decitabine prophylaxis on the relapse for acute lymphoblastic leukemia. Bone Marrow Transplant 58, 687–695 (2023). https://doi.org/10.1038/s41409-023-01948-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01948-y
This article is cited by
-
Immortal time bias in hematopoietic cell transplantation
Bone Marrow Transplantation (2023)