Abstract
Allogeneic hematopoietic stem cell transplantation (HSCT) is still needed for many children with very high-risk acute leukemia. An HLA-haploidentical family donor is a suitable option for those without an HLA-matched donor. Here we present outcomes of a novel HLA-haploidentical HSCT (haplo-HSCT) strategy with adoptive immunotherapy with thymic-derived CD4+CD25+ FoxP3+ regulatory T cells (Tregs) and conventional T cells (Tcons) performed between January 2017 and July 2021 in 20 children with high-risk leukemia. Median age was 14.5 years (range, 4–21), 15 had acute lymphoblastic leukemia, 5 acute myeloid leukemia. The conditioning regimen included total body irradiation (TBI), thiotepa, fludarabine, cyclophosphamide. Grafts contained a megadose of CD34+ cells (mean 12.4 × 106/Kg), Tregs (2 × 106/Kg) and Tcons (0.5–1 × 106/Kg). All patients achieved primary, sustained full-donor engraftment. Only one patient relapsed (5%). The incidence of non-relapse mortality was 15% (3/20 patients). Five/20 patients developed ≥ grade 2 acute Graft versus Host Disease (aGvHD). It resolved in 4 who are alive and disease-free; 1 patient developed chronic GvHD (cGvHD). The probability of GRFS was 60 ± 0.5% (95% CI: 2.1–4.2) (Fig. 6), CRFS was 79 ± 0.9% (95% CI: 3.2–4.9) as 16/20 patients are alive and leukemia-free. The median follow-up was 2.1 years (range 0.5 months–5.1 years). This innovative approach was associated with very promising outcomes of HSCT strategy in pediatric patients.
Similar content being viewed by others
Introduction
Prognosis of pediatric patients with acute leukemia (AL), particularly acute lymphoblastic leukemia (ALL), has greatly improved. The 5-year event-free survival (EFS) rate is now over 80% [1], due to more in-depth genetic and molecular characterization predicting treatment response, design of risk-adapted therapy and new chemotherapy protocols [2]. Blinatumomab, inotuzumab ozogamicin (InO) and the CD19 chimeric antigen receptor T-cell (tisagenlecleucel) improved response rates and survival compared with historic controls in children with ALL [3,4,5,6]. Despite this new approach, many patients may still require HSCT to maintain disease remission [7]. In fact, at specific time-points, monitoring minimal residual disease predicts the risk of relapse and therefore guides the indication to HSCT in first complete remission [8,9,10].
The need for alternative donors has always driven HLA-haploidentical HSCT (haplo-HSCT). Originally based on a megadose of CD34+ stem cells, the haplo-HSCT protocol has been modified over time to improve immunological reconstitution and to reduce non-relapse mortality rates (NRM). It has included T-cell depletion, α/β T and CD19+ B-cell depletion, and post-transplant high-dose cyclophosphamide (PT/Cy) in T-cell replete haplo-HSCT [11,12,13]. Despite all these approaches, relapse is still, at present, the major cause of haplo-HSCT failure in pediatric patients with high-risk (HR) leukemia. Indeed, the cumulative incidence of relapse in the main pediatric protocols of haplo-HSCT is about 24%. In adult patients with AL in Perugia BMT Center, haplo-HSCT with Treg/Tcon adoptive immunotherapy and no post-transplant pharmacological immunosuppression, had a very low incidence of relapse (4%) and 75% chronic GvHD/relapse-free survival (CRFS) [14]. From 2017 to date the Perugia Pediatric Oncology-Hematology Unit has adopted the adult protocol in 20 pediatric patients. Such transplantation protocol is based on high-dose myeloablative conditioning regimen which include total body irradiation (TBI) and chemotherapy, T-cell depleted hematopoietic CD34+ stem cells and the add-back of 2 million/kg body weight of regulatory T cells followed by 1 million/kg body weight conventional T cells. Tregs were able to control otherwise lethal aGvHD in the haplo setting and, at the same time, did not inhibit Graft-versus-Leukemia effect. Here, we show the results of this transplantation strategy in very HR patients.
Subjects and methods
The haplo-HSCT protocol was approved by the Umbria Regional Hospital Ethics Committee and registered as protocol ID 02/14 and as NCT03977103 in ClinicalTrials.gov. Patients with HR ALL or AML without a matched related or unrelated donor were eligible. Before enrollment, patients’ parents provided written informed consent in accordance with the Helsinki Declaration. Between January 2017 and July 2021, 20 pediatric patients (15 ALL, 5 AML, median age 14.5 years; range 4–21) with HR AL were enrolled. Six patients were transplanted in CR1, 9 patients in CR2, 5 in ≥CR3. Tables 1 and 2 report demographics, disease characteristics, cytogenetics and molecular markers, status at transplant of each patient and donor characteristics. Five patients showed extramedullary disease (Table 1). Median time from diagnosis to transplantation was 9.5 months (range 3–40), median time from relapse to transplantation for CR2 and CR3 patients was 3 months (range 3–15).
Donors
Donors were healthy family members with one HLA-haplotype identical to the patient’s (Table 1). Mothers were selected in 13/20 cases, mainly because they were available and the survival rate was reported to be better with mother as donor [15, 16]. Natural killer-alloreactive donors were available for 10/20 patients [17].
Transplant procedure
The conditioning regimen included TBI and chemotherapy. In 16 patients TBI was delivered with this schedule: 1.5 Gy × 2/day for 4.5 days, total 13.5 Gy; in 4 patients with median age of 4 years, TBI was delivered with this schedule: 3.3 Gy/day for 3 days, total: 9.9 Gy. Since patients with median age of 4 years needed to be sedated before irradiation, schedule of TBI was different and consequently also total radiation dose in order to reduce radiotherapy sessions. Chemotherapy included thiotepa (5 mg/kg for 2 days), fludarabine (40 mg/m2 for 4 days), cyclophosphamide (15 mg/kg/day for 2 days). All patients received T-regs on day −4 (2 × 106/Kg), T-cons on day −1 (0.5 × 106/Kg for 10 patients; 1 × 106/Kg for the other 10) and megadose positively selected CD34+ cells (mean 12.4 × 106/Kg, range 7.1–24.5) on day 0 (Fig. 1), sirolimus, a selective mTOR inhibitor (2 mg/m2 from days −8 to −4). Sirolimus blood levels were monitored daily so as to reach the therapeutic range (between 5–10 ng/ml) on day −4 (Treg infusion) and achieve clearance on day 0 (CD34+ cell infusion). On day −2 Rituximab (200 mg/mq) was administered as post-transplant lymphoproliferative disorder (PTLD) prophylaxis. No post-transplant pharmacological GvHD prophylaxis was given.
Graft processing
Before administering granulocyte colony-stimulating factor (G-CSF) to mobilize hematopoietic progenitor cells, donor Tregs and Tcons were collected. CD3+ T cells were separated from the leukapheresis product on a Ficoll-Hypaque gradient. In total, 0.5 × 106/kg of Tcons were infused into ten patients, 1 × 106/kg in 10. Doses of CD3+ T cells was established according to the purity of Tregs. After, the leukapheresis product was depleted of CD8+/CD19+ cells and then CD25+ cells were positively selected and then, CD4+CD25+ Tregs were selected by an immunomagnetic procedure using the CliniMACS device (Miltenyi Biotec GmbH, Bergisch Gladbach, Germany). On average the Treg product contained 84 ± 4.9% of CD4+CD25+FOXP3+ cells and 25 ± 6.7% of CD127+ cells. In total, 2 × 106/kg Tregs were infused into each patient. After G-CSF administration, donor CD34+ cells were collected from 2–3 leukaphereses and positively immuno-selected (CliniMACS) [18, 19].
End-points and definitions
Primary end-points were the cumulative incidences of NRM and relapse (defined as disease recurrence according to marrow morphology, flow cytometry, cytogenetics, fluorescence in situ hybridization and polymerase chain reaction). Secondary end-points were: full donor-type engraftment, the cumulative incidences of grades ≥2 aGvHD and cGvHD, the probability of GvHD/relapse-free survival (GRFS) and CRFS. Immune reconstitution was monitored by means of T-cell counts and specific responses to pathogens. The method and evaluation of clones were described elsewhere [18].
Statistics
Cumulative incidence estimates (as evaluated by the Gray test) were used for aGvHD and relapse and NRM which were competing risks. The Kaplan–Meier method evaluated GRFS and CRFS.
Results
Engraftment
All patients achieved primary, sustained full-donor-type engraftment, reaching ANC > 0.5 × 109/l at a median of 14 days (range 10–17). The median time to platelet counts >20 × 109/l was 17 days (range 10–35).
Conditioning regimen related toxicity
In accordance with the Common Terminology Criteria for Adverse Events, toxicity was mild (Grade 1) or moderate (Grade 2). No patient developed more than grade II oral mucositis.
GvHD
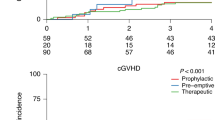
Grade ≥ II aGvHD developed in 5/20 patients, with 1/5 developing grade III/IV and dying on day 35 post-transplant. The cumulative incidence was 33% (±2%). Median time to onset was 19 days (range 8–80 days) (Fig. 2). Patients were treated with high-dose steroids and early extracorporeal photopheresis, with 3 procedures/week for a median of 6 weeks, tapering to two procedures/week and finally one/week. Photopheresis was concomitant with steroid therapy tapering after 7 days during which patients received sirolimus (2/5), cyclosporine (1/5) and mycophenolic acid (1/5). Infliximab was administered to 2/5 patients, Ruxolitinib to 3/5 and Begelomab, a CD26 monoclonal antibody, together with Anti-Thymocyte Globulins to 1/5. Immunosuppressive therapy lasted for a median of 6.5 months (range 6–9). Four patients are alive and have suspended immunosuppressive therapy. One patient, who developed cGvHD, is currently off-immunosuppressive therapy and in disease remission (Fig. 2).
Immune reconstitution
Peripheral blood CD3+ cells reached medians of 319/µl (range 119–2217/µl) and 727/µl (range 136–1656) at 30 and 100-day post-transplant respectively, CD4+ cells reached a median value of 149/µl (range 71–481/µl) and 235/µl (range 67–659) at 30 and 100-day post-transplant, respectively, CD8+ cells reached a median value of 151/µl (range 18–1465/µl) and 408/µl (range 69–1288) at 30 and 100-day post-transplant respectively (Fig. 3). Both CD19+ and CD20+ cells reached respectively a median of 56/µl (range 0–101) and 188/µl (range 38–248).
Specific CD4+ and CD8+ lymphocytes against opportunistic pathogens such as HHV-6, Aspergillus fumigatus, Candida albicans, CMV, adenovirus, human herpesvirus-6 (HHV6), herpes simplex virus, varicella zoster virus and toxoplasma soon emerged (Fig. 4).
Infectious complications
Six/20 patients (30%) presented EBV viremia (median viral load: 12,500 copies/ml; range 2817–400,000) at a median of 53 days post-transplant (range: 42–84). PTLD in 2/6 patients was successfully treated with 4 doses of Rituximab (375 mg/m2). Subsequently from June 2017 onwards, prophylaxis with Rituximab (200 mg/m2) was started on day −2 and no further cases of PTLD occurred. Post-transplant HHV-6 reactivation was observed in all 20 patients (median viral load 14,121 copies/ml; range 705–284,794 copies/ml), at a median of 9 days (range: 6–15). Organ involvement in 10 (50%) (1 encephalitis, 2 hepatitis, 1 pneumonia, 4 gastroenteritis and 2 multi-organ involvement with pneumonia and enteritis) was successfully treated with 90 mg/Kg foscarnet twice daily. Two patients with HCV RNA positivity before transplant developed HCV hepatitis and liver failure at 68 days and 25 days post-transplant with histological evidence of hepatitis associated with a significant increase in HCV viremia (respectively 3,519,000 UI/ml and 6,545,000 UI/ml). Direct-acting antivirals completely resolved liver failure and negativized viremia. Although the incidence of CMV infection was 35% (5/20 patients), no patient died of CMV. Two/20 patients developed invasive fungal infections (10%). Gram negative sepsis was demonstrated in 6/20 patients (30%) and 4/6 displayed multi drug resistance, Gram positive sepsis occurred in 2/20 (10%). One patient contracted SARS-CoV-2 on day +110 post-transplant and recovered without severe acute respiratory syndrome and/or apparent sequelae. Antiviral therapy with Remdesivir was started, together with intravenous immunoglobulins and 3 hyperimmune plasma infusions. SARS-CoV-2 positivity persisted in PCR on nasopharyngeal swabs for over 2 months, while patient presented no respiratory symptom nor fever. After 72 days, the patient was negative and SARS-Cov-2 antibodies were strongly positive (78.6 AU/ml).
NRM and causes of death
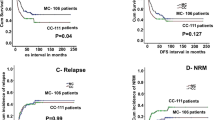
The NRM cumulative incidence was 15% (3/20) (Fig. 5). Causes were: invasive aspergillosis (1 patient), grade IV aGVHD [1], acute respiratory distress syndrome [1].
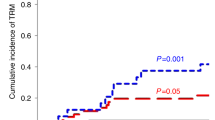
Relapse and GRFS
At a median follow up of 2.1 years (range 0.5 months–5.1 years), 1 patient who was transplanted in CR3 relapsed (Fig. 5). He underwent a second transplant from a different haploidentical familial donor but died of relapse 7 months after transplant. At a median follow up of 2.1 years, the probability of GRFS was 60 ± 0.5% (95% CI: 2.1–4.2) (Fig. 6), CRFS was 79 ± 0.9% (95% CI: 3.2–4.9) as 16/20 patients are alive and leukemia-free (Fig. 7).
Discussion
This study demonstrated that, in a small cohort of pediatric patients, the haplo-HSCT with a megadose of CD34+ hematopoietic stem cells and Treg/Tcon adoptive immunotherapy eradicated leukemia in most, achieving 80% leukemia-free survival and 75% leukemia/cGvHD free survival rates. All patients were affected by very HR leukemia according to cytogenetics, molecular markers and disease stage at transplant. Encouragingly, 5/20 patients who had extramedullary disease, are alive and well, in complete remission (Table 3).
These promising results, which need to be confirmed in a larger study, compare favorably with outcomes of several alternative haplo-HSCT protocols in similar HR patients. α/β T and CD19+ B-cell depletion in 80 children with AL was associated with 24% CI of relapse. Bertaina et al. [20] compared outcomes after transplants using this protocol (98 patients), matched unrelated donors (127 patients) and mismatched donors (118 patients). The α/β T and CD19+ B-cell depletion protocol emerged as intermediate for leukemia-free survival, with a lower CI of NRM and a better GFRS than the other approaches. After receiving CD3/CD19 depleted allografts 46 pediatric patients achieved an overall 38% probability of relapse at 2 years [21].
Our results show also better protection from relapse if compared with unmanipulated transplants in children. In fact, John Hopkins Hospital reported 52% cumulative incidence (CI) of relapse, 33% CI of Grade II–IV aGvHD, 24% CI of cGVHD and a 3-year EFS of 32% in children with HR AL who underwent T-replete HSCT with PT/Cy [22]. The AIEOP-GITMO retrospective multicenter study showed that T cell replete PT/Cy HSCT in 33 pediatric patients with HR hematological malignancies achived 24% CI of relapse and 72% OS at 1-year follow-up [11]. One factor that might influence relapse rates in T-cell depleted transplantation is the absence of effector T cells that are known to prevent leukemia relapse. On the contrary, in the unmanipulated transplants, the reason of high rate of leukemia relapse may be post-transplant pharmacological immunosuppression, like PT/Cy for example, as it inhibits alloreactive lymphocytes against leukemia.
Without any post-transplant pharmacological immunosuppression, the 4-year relapse rate of 1 in 20 in the present study indicates our haplo-HSCT protocol exerted a strong anti-leukemia effect (GvL) which also occurred in extramedullary sites. TBI not in single dose not only reduced toxicity but also contributed to a better GvL effect, as demonstrated by FORUM trial [23] and in matched T-depleted HSCT [24]. Even adult patients with AL who underwent HSCT with this protocol were protected from GvHD [18] and post-transplant leukemia relapse as the CI was significantly lower than in historical controls (0.05 versus 0.21; P 5.03) [18, 19].
The mechanism underlying maintenance of the GvL effect and GvHD prevention was studied in-depth in pre-clinical models [25]. Evidence that Tregs and Tcons exerted a strong GvL effect was obtained from an xenogenic murine transplant model of engrafted human lymphoblastic or myeloid leukemia. Infusion of Tregs and Tcons rescued mice which survived without GvHD. Different Treg and Tcon migratory properties were hypothesized to underlie the GvL effect without GvHD. Tcons colocalized with Tregs in the skin, liver and bowel, where Tcon inhibition prevented GvHD [19]. Since Tcons expressed the CXCR4 Bone Marrow homing molecule more intensely than Tregs, they alone homed to the bone marrow, exerting a powerful GVL effect through alloantigen recognition [19].
In the present study, although the cumulative incidence of aGvHD was 33%, 4/5 patients are alive, leukemia-free, off immune-suppressive therapy and free of cGVHD. Early photopheresis permitted steroid therapy to be soon tapered and suspended in all patients [26]. The incidence of aGvHD in such protocol [14, 18, 19] may be explained first with the fact that we infused otherwise lethal doses of effector T cells in a mismatched setting without infusion of Tregs. It should be emphasized that, as we previously demonstrated, Treg infusions largely prevented the potential lethality of infusing 0.5–1 million Tcons in the absence of any pharmacological GVHD prophylaxis [18, 19]. In fact, only 1 patient died as a result of aGVHD. Moreover, the present cohort had been heavily pre-treated before transplantation. Most had been subjected to many lines of therapy, often had an unclear disease history and did not have cytogenetics or molecular markers at diagnosis. Secondly, through CD3+ and CD8+ T-cell reactions, HHV-6 reactivation could have played role in aGvHD [27] as it occurred in all our patients medianly at day +9 post-transplant, with 50% developing non-fatal organ involvement [28]. Cytokine release in the peri-engraftment period, particularly of IL-6, may have been involved in triggering HHV6 infection [29]. Finally, post-transplant immune recovery with rapid increases in peripheral blood T-cells and pathogen-specific CD4+ and CD8+ T-cell responses against HHV-6 may have been a double-edged sword. On the one hand, it was probably responsible for clearing infection and the quite good final outcome but on the other, it may have triggered HHV6 reactivation. To reduce the aGvHD incidence we modified our transplant protocol to include sirolimus, an mTOR inhibitor (2 mg/m2 on days −8 to −4) in the conditioning regimen for the last ten patients. Evidence from several clinical trials in diverse transplant recipients showed that, unlike cyclosporine, it promoted Treg cell expansion in vivo [30] by converting CD4+CD25naive T cells into CD4+Foxp3+ Tregs [31], thus controlling the activity of the effector T lymphocytes that cause GvHD [32]. Although the incidence of aGvHD was similar in the two subgroups, the disease seemed less severe as patients in the later group required less immunosuppressive therapy. Undoubtedly, a larger cohort is needed before any definitive conclusions can be drawn on the validity of sirolimus as part of the conditioning regimen.
Although we observed high aGvHD rates, despite immune-suppressive therapy, CD4+ and CD8+ pathogen-specific frequencies reached normal levels by 2nd/3rd month post-transplant. Despite 35% incidence of CMV infection, only one patient developed CMV disease (pneumoniae) and at present is alive and well. In 2020 early in the pandemic, one patient contracted SARS-CoV-2 post-transplant, without severe acute respiratory syndrome and/or apparent sequelae. Since the original Covid variant was associated with immune hyper-reactivity, our patient’s immunodeficiency with few T cells may have protected against severe Covid-19 disease [33]. Moreover, it is of note that only one patient developed cGvHD (now he is off-therapy), and no patient who underwent immunosuppressive therapy died for TRM or relapsed. The extremely low incidence of cGVHD was probably related to Treg infusion [34].
This study is limited by the relatively small cohort and present outcomes need to confirmed in a large series. However, at a median follow up of 4 years the results are encouraging with only 1 relapse to date. In our view, this protocol of haplo-HSCT with adoptive Treg/Tcon immunotherapy is to be a good strategy for pediatric patients with very HR AL.
References
Merli P, Algeri M, Del Bufalo F, Locatelli F. Hematopoietic stem cell transplantation in pediatric acute lymphoblastic leukemia. Curr Hematol Malig Rep. 2019;14:94–105.
Borowitz MJ, Devidas M, Hunger SP, Bowman WP, Carroll AJ, Carroll WL, et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia and its relationship to other prognostic factors: a Children’s Oncology Group study. Blood. 2008;111:5477–85. https://doi.org/10.1182/blood-2008-01-132837.
Locatelli F, Zugmaier G, Mergen N, Bader P, Jeha S, Schlegel PG, et al. Blinatumomab in pediatric patients with relapsed/refractory acute lymphoblastic leukemia: results of the RIALTO trial, an expanded access study. Blood Cancer J 2020;10:77. https://doi.org/10.1038/s41408-020-00342-x.
Bhojwani D, Sposto R, Shah NN, Rodriguez V, Yuan C, Stetler-Stevenson M, et al. Inotuzumab ozogamicin in pediatric patients with relapsed/refractory acute lymphoblastic leukemia. Leukemia. 2019;33:884–92. https://doi.org/10.1038/s41375-018-0265-z.
Pasquini MC, Hu ZH, Curran K, Laetsch T, Locke F, Rouce R, et al. Real-world evidence of tisagenlecleucel for pediatric acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Adv. 2020;4:5414–24. https://doi.org/10.1182/bloodadvances.2020003092.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378:439–48. https://doi.org/10.1056/NEJMoa1709866.
Curran E, O’Brien M. Role of blinatumomab, inotuzumab, and CAR T-cells: which to choose and how to sequence for patients with relapsed disease. Semin Hematol. 2020;57:157–63. https://doi.org/10.1053/j.seminhematol.2020.11.001.
Kruse A, Abdel-Azim N, Kim HN, Ruan Y, Phan V, Ogana H, et al. Minimal residual disease detection in acute lymphoblastic leukemia. Int J Mol Sci. 2020;21:1054. https://doi.org/10.3390/ijms21031054.
Segerink WH, de Haas V, Kaspers GJL. Measurable residual disease in pediatric acute myeloid leukemia: a systematic review. Expert Rev Anticancer Ther. 2021;21:451–9. https://doi.org/10.1080/14737140.2021.1860763.
Conter V, Bartram CR, Valsecchi MG, Schrauder A, Panzer-Grümayer R, Möricke A, et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood. 2010;115:3206–14. https://doi.org/10.1182/blood-2009-10-248146.
Berger M, lanino E, Cesaro S, Zecca M, Vassallo E, Faraci M, et al. Feasibility and outcome of haploidentical hematopoietic stem cell transplantation with post-transplant high-dose cyclophosphamide for children and adolescents with hematologic malignancies: an AIEOP-GITMO retrospective multicenter study. Biol Blood Marrow Transplant. 2016;22:902–9. https://doi.org/10.1016/j.bbmt.2016.02.002.
Dufort G, Castillo S, Pisano S, Castiglioni M, Carolina P, Andrea I. Haploidentical hematopoietic stem cell transplantation in children with high-risk hematologic malignancies: outcomes with two different strategies for GvHD prevention. Ex vivo T-cell depletion and post-transplant cyclophosphamide: 10 years of experience at a single center. Bone Marrow Transplant. 2016;51:1354–60. https://doi.org/10.1038/bmt.2016.161.
Locatelli F, Merli P, Pagliara D, Li Pira G, Falco M, Pende D, et al. Outcome of children with acute leukemia given HLA-haploidentical HSCT after αβ T-cell and B-cell depletion. Blood. 2017;130:677–85. https://doi.org/10.1182/blood-2017-04-779769.
Pierini A, Ruggeri L, Carotti A, Falzetti F, Saldi S, Terenzi A, et al. Haploidentical age-adapted myeloablative transplant and regulatory and effector T cells for acute myeloid leukemia. Blood Adv. 2021;5:1199–208. https://doi.org/10.1182/bloodadvances.2020003739.
Stern M, Ruggeri L, Mancusi A, Bernardo ME, de Angelis C, Bucher C, et al. Survival after T cell-depleted haploidentical stem cell transplantation is improved using the mother as donor. Blood. 2008;112:2990–5. https://doi.org/10.1182/blood-2008-01-135285.
Kruchen A, Stahl T, Gieseke F, Binder TM, Özcan Z, Meisel R, et al. Donor choice in haploidentical stem cell transplantation: fetal microchimerism is associated with better outcome in pediatric leukemia patients. Bone Marrow Transpl. 2015;50:1367–70. https://doi.org/10.1038/bmt.2015.136.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295:2097–100.
Di Ianni M, Falzetti F, Carotti A, Terenzi A, Castellino F, Bonifacio E, et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood. 2011;117:3921–8. https://doi.org/10.1182/blood-2010-10-311894.
Martelli MF, Di Ianni M, Ruggeri L, Falzetti F, Carotti A, Terenzi A, et al. HLA-haploidentical transplantation with regulatory and conventional T-cell adoptive immunotherapy prevents acute leukemia relapse. Blood. 2014;124:638–44. https://doi.org/10.1182/blood-2014-03-564401.
Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical alpha/beta T-cell and B-cell depleted HSCT in children with acute leukemia. Blood. 2018;132:2594–607. https://doi.org/10.1182/blood-2018-07-861575.
Lang P, Teltschik HM, Feuchtinger T, Muller I, Pfeiffer M, Schumm M, et al. Transplantation of CD3/CD19 depleted allografts from haploidentical family donors in paediatric leukaemia. Br J Haematol. 2014;165:688–98. https://doi.org/10.1111/bjh.12810.
Klein OR, Buddenbaum J, Tucker N, Chen AR, Gamper CJ, Loeb D, et al. Nonmyeloablative haploidentical bone marrow transplantation with post-transplantation cyclophosphamide for pediatric and young adult patients with high-risk hematologic malignancies. Biol Blood Marrow Transpl. 2017;23:325–32. https://doi.org/10.1016/j.bbmt.2016.11.016.
Peters C, Dalle JH, Locatelli F, Poetschger U, Sedlacek P, Buechner J, et al. Total body irradiation or chemotherapy conditioning in childhood ALL: a multinational, randomized, noninferiority phase III study. J Clin Oncol. 2021;39:295–307. https://doi.org/10.1200/JCO.20.02529.
Aristei C, Carotti A, Palazzari E, Amico L, Ruggeri L, Perrucci E, et al. The total body irradiation schedule affects acute leukemia relapse after matched T cell-depleted hematopoietic stem cell transplantation. Int J Radiat Oncol Biol Phys. 2016;96:832–9. https://doi.org/10.1016/j.ijrobp.2016.07.025.
Edinger M, Hoffmann P, Ermann J, Drago K, Fathman CG, Strober S, et al. CD4+CD25+ regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow transplantation. Nat Med. 2003;9:1144–50. https://doi.org/10.1038/nm915.
Perotti C, Del Fante C, Tinelli C, Viarengo G, Scudeller L, Zecca M, et al. Extracorporeal photochemotherapy in graft-versus-host disease: a longitudinal study on factors influencing the response and survival in pediatric patients. Transfusion. 2010;50:1359–69.
Gotoh M, Yoshizawa S, Katagiri S, Suguro T, Asano M, Kitahara T, et al. Human herpesvirus 6 reactivation on the 30th day after allogenic hematopoietic stem cell transplantation can predict grade 2-4 acute graft versus-host disease. Transpl Infect Dis. 2014;16:440–9.
Perruccio K, Sisinni L, Perez-Martinez A, Valentin J, Capolsini I, Massei MS, et al. High incidence of early human Herpesvirus-6 infection in children undergoing haploidentical manipulated stem cell transplantation for hematologic malignancies. Biol Blood Marrow Transplant. 2018. https://doi.org/10.1016/j.bbmt.2018.07.033.
Ogata M, Satou T, Kawano R, Takakura S, Goto K, Ikewaki J, et al. Correlations of HHV-6 viral load and plasma IL-6 concentration with HHV-6 encephalitis in allogeneic stem cell transplant recipients. Bone Marrow Transpl. 2010;45:129–36. https://doi.org/10.1038/bmt.2009.116.
Cutler C, Antin JH. Sirolimus immunosuppression for graft-versus-host disease prophylaxis and therapy: an update. Curr Opin Hematol. 2010;17:500–4. https://doi.org/10.1097/MOH.0b013e32833e5b2e.
Bansal D, Yadav AK, Kumar V, Minz M, Sakhuja V, Jha V. Deferred pre-emptive switch from calcineurin inhibitor to sirolimus leads to improvement in GFR and expansion of T regulatory cell population: a randomized, controlled trial. PLoS ONE. 2013;8:e75591. https://doi.org/10.1371/journal.pone.0075591.
Tkachev V, Furlan SN, Watkins B, Hunt DJ, Zheng HB, Panoskaltsis-Mortari A, et al. Combined OX40L and mTOR blockade controls effector T cell activation while preserving T reg reconstitution after transplant. Sci Transl Med. 2017;9:eaan3085. https://doi.org/10.1126/scitranslmed.aan3085.
Massei MS, Capolsini I, Cerri C, Gurdo G, Mastrodicasa E, Perruccio K, et al. SARS-CoV-2 infection in an adolescent after haploidentical stem cell transplantation. Clin Oncol. 2021;6:1787.
Theil A, Tuve S, Oelschlägel U, Maiwald A, Döhler D, Oβmann D, et al. Adoptive transfer of allogeneic regulatory T cells into patients with chronic graft-versus-host disease. Cytotherapy. 2015;17:473–86. https://doi.org/10.1016/j.jcyt.2014.11.005.
Acknowledgements
The authors thank Geraldine Anne Boyd and Fabio De Paola for editorial assistance, the nonprofit charity associations Comitato per la Vita Daniele Chianelli and nurses and the multidisciplinary group of the hematopoietic stem cell transplantation program. The authors also thank the patients and their caregivers for participating in this study.
Author information
Authors and Affiliations
Contributions
MSM provided clinical care, performed research, and wrote the manuscript; IC performed research and evaluated suitability of donors; EM, KP, FA, CC, GG, SS and MB provided clinical care; FF, TZ and RIO processed the graft; SiSa designed and performed; RT performed HLA typing; OM evaluated suitability of donors; BMP and SS performed radiation treatment; MM collected clinical data; MaMa and OM evaluated suitability of donors and performed leukaphereses and photophereses; CA supervised radiation therapy and reviewed the manuscript; AV, AP, LR, MFM and AC reviewed the manuscript; MC provided clinical care, supervised the pediatric transplantation program, and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Massei, M.S., Capolsini, I., Mastrodicasa, E. et al. HLA-haploidentical hematopoietic stem cells transplantation with regulatory and conventional T-cell adoptive immunotherapy in pediatric patients with very high-risk acute leukemia. Bone Marrow Transplant 58, 526–533 (2023). https://doi.org/10.1038/s41409-023-01911-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01911-x