Abstract
Mucopolysaccharidosis type I-H (MPS I-H) is a rare lysosomal storage disorder caused by α-L-Iduronidase deficiency. Early haematopoietic stem cell transplantation (HSCT) is the sole available therapeutic option to preserve neurocognitive functions. We report long-term follow-up (median 9 years, interquartile range 8–16.5) for 51 MPS I-H patients who underwent HSCT between 1986 and 2018 in France. 4 patients died from complications of HSCT and one from disease progression. Complete chimerism and normal α-L-Iduronidase activity were obtained in 84% and 71% of patients respectively. No difference of outcomes was observed between bone marrow and cord blood stem cell sources. All patients acquired independent walking and 91% and 78% acquired intelligible language or reading and writing. Intelligence Quotient evaluation (n = 23) showed that 69% had IQ ≥ 70 at last follow-up. 58% of patients had normal or remedial schooling and 62% of the 13 adults had good socio-professional insertion. Skeletal dysplasia as well as vision and hearing impairments progressed despite HSCT, with significant disability. These results provide a long-term assessment of HSCT efficacy in MPS I-H and could be useful in the evaluation of novel promising treatments such as gene therapy.
Similar content being viewed by others
Introduction
Mucopolysaccharidosis type I (MPS I) is a lysosomal storage disorder caused by α-L-Iduronidase deficiency, responsible for glycosaminoglycan (GAG) deposition in many tissues. Patients display coarse facial features, hepatosplenomegaly, neurocognitive decline, progressive skeletal dysplasia, heart valvular disease and vision and hearing loss. In its most severe form, Hurler disease (MPS I-H), symptoms are already present before 18 months of age, with death occurring by the age of 10 years in the absence of treatment [1].
Although gene therapy using lentiviral vectors has shown promising results in the treatment of children with MPS I-H [2], haematopoietic stem cell transplantation (HSCT) remains the standard of care to prevent neurocognitive decline, when performed before 24–30 months of age and in the absence of significant pre-existing neurological impairment [3, 4]. The aim of HSCT is to restore a normal enzymatic activity in all organs, and especially in the central nervous system through corrected microglial cells. Due to poor vascularization, corneal clouding and skeletal dysplasia are incompletely corrected following HSCT and they remain the two main disabilities at adulthood despite transplantation [1, 3]. Enzyme replacement therapy (ERT) is the only alternative therapeutic option for MPS I, but it cannot cross the blood-brain barrier and is only effective for soft tissue GAG deposits [5, 6]. Few studies have assessed the long-term outcome after HSCT [3, 7].
In this study, we retrospectively analyzed long-term outcome after HSCT in a multicentric retrospective cohort of MPS I-H patients.
Material and methods
51 patients with MPS I-H, defined on the severity of the initial clinical presentation, who underwent HSCT between 1986 and 2018 were included in this study. Patients with a Hurler-Scheie (milder) phenotype were excluded. Patients or patients’ parents/legal guardians provided written consent (RADICO National study approved by independent ethics committee). Patients were monitored in reference centers in Paris (n = 34), Marseille (n = 7), Montpellier (n = 5), Lille (n = 2), Tours (n = 2) or Bordeaux (n = 1). Follow-up was performed in their respective centers: closely the first year after HSCT, then every 6 months for check-up and annually for their multidisciplinary evaluation according to published guidelines [8]. Follow-up was more frequent for patients who had resumed ERT after HSCT.
Data from clinical examination, neurocognitive development assessment, ENT or ophtalmologist evaluation, imaging (echocardiography, brain magnetic resonance imaging/MRI), pulmonary function tests and laboratory parameters (whole blood chimerism, urinary GAG quantification, α-L-Iduronidase activity) were retrospectively collected and analyzed. For the neurocognitive evaluation, results of developmental quotient (DQ) before HSCT (Brunet Lezine scale) and intelligence quotient (IQ) after HSCT (WPPSI, WISC or WAIS scales according to age) were graded based on the IQ mental retardation scale: IQ/DQ ≥ 85, between 70 and 85, between 50 and 70 or <50/not evaluable. Academic achievements were classified as follows for children ≥ 6 years of age: 1. Normal or remedial schooling (for minor learning disabilities such as dyslexia, hyperactivity); 2. Specialized schools for intellectual disability; 3. Medically supervised full-time institution (for severe mental retardation). For the adult patients, achievements were graded as follows: 1. Good socio-professional insertion, if patients were able to work or to be involved in vocation training or graduate education; 2. Adapted employment in a specific institution for mentally disabled workers; 3. Neither of the above.
Quantitative variables are presented as median and inter-quartile range Q1–Q3 (IQR) or range (for low sample size). Quantitative variables were compared using the two-sided Student’s T test (similar variances) and qualitative variables using the Chi-square test if expected sample sizes were >5 or the Fisher exact test if <5. Survival curves were evaluated using Kaplan–Meier estimates, using the R software (version 4.2.0).
Results
HSCT and early outcome
Patients were diagnosed at a median age of 10 months and displayed typical Hurler disease features (Table 1), as well as frequent truncating IDUA gene mutations, as described in MPS I-H [9]. Active non-obstructive hydrocephalus was present in 9 patients before HSCT (18%), and half of the patients displayed white matter hyperintensities (WMH) on MRI (Table 1). DQ was higher than 70 in 33 patients (89%) and higher than 85 in 17 patients (46%) (Table 2).
HSCT was performed at a median age of 18 months (IQR 14–25, Table 2), after 24 months of age in 13 children (median 26 months). Bone marrow was the main stem cell source (67%) whereas all remaining patients received cord blood stem cells. 20 patients (44%) received a graft from matched unrelated donor (MUD), 14 patients (31%) from mismatched unrelated donor (MMUD) and 10 patients (22%) from matched sibling donor (MSD). Among the 10 MSD, 7 were carrier for IDUA mutations, 1 was non-carrier and this information was not available for 2 patients. Donor α-L-Iduronidase enzymatic activity was only available for 4 patients with median values of 61% of control (range 49–96%). Conditioning regimen evolved with time, relying on busulfan-cyclophosphamide for HSCT before 2012 or busulfan-fludarabine for more recent HSCT. GvHD prophylaxis included cyclosporine-A (100%), anti-thymocyte globulin (86%), mycophenolate-mofetil (43%), methotrexate (13%) and/or steroids (13%). Since 2004, pre-transplant ERT is available to reduce the storage phenotype while waiting for the HSCT [5, 6], and was given to 31 of the 37 patients transplanted after 2004 (84%). It was stopped at the time of stem cells infusion in 14 patients (45%) or maintained for a median duration of 22 weeks after HSCT (IQR 17–52) for the remaining patients.
8 patients experienced rejection (16%, primary n = 3/8, secondary n = 5/8), most frequently with cord blood (n = 5/8) and a MMUD (n = 4/8). One patient did not receive a second HSCT because of parental choice, whereas all 7 remaining patients received a second HSCT after a median delay of 4 months (range 2–27), successful in all. Acute graft vs host disease (GvHD) occurred in 29 patients (59%, Table 2), with 8 patients (16%) having GvHD ≥ grade III, and responded well to treatment in most patients. Chronic GvHD developed in 7 patients (14%), with 3 patients (6%) having GvHD ≥ grade III. Viral replication was the second most frequent complication. 4 patients died from transplant-related mortality (TRM) within the first year after HSCT (severe GvHD: n = 2; thrombotic microangiopathy with sepsis: n = 1; sepsis few days after HSCT: n = 1).
Long-term follow-up after HSCT
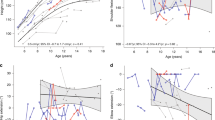
47 patients survived beyond the first year after HSCT (Fig. 1). The median follow-up after HSCT was 9 years (IQR 8–16.5, Table 2), with 13 patients having reached adulthood (range 18–34 years old). One patient (already reported) died during follow-up at 20 years of age from pulmonary hypertension [10].
At last follow-up, 38 patients out of 45 (84%) displayed a complete chimerism on whole blood (≥ 95% donor chimerism) and 30 patients out of 42 (71%) had leukocyte α-L-Iduronidase activity within normal range (Table 2). None of the patients needed immunosuppressive therapy for GvHD. Serum α-L-Iduronidase activity, available for only 6 patients, was low (median 36% of control values). At last follow-up, 6 patients still received ERT: 2 continuously since HSCT (including the patient with rejection and no second HSCT) and 4 because of disease progression during follow-up (see below).
Neuro-developmental outcome
All children had a delay in motor milestones and all acquired unaided walking (Table 3). Intelligible speech was acquired by 91% of patients. By the age of 8 years, 78% of patients had acquired writing and reading abilities. 10 patients had hydrocephalus, prior to HSCT in 9 and within a few months after HSCT in a last patient. WMH or cortical atrophy were present in one third of the patients (Table 3). An IQ evaluation was available for 23 patients at a median age of 9 years (IQR 5.7–12) and was within “normal” range (≥70, i.e above -2 standard deviations) in 69% of patients (71% of patients <10 years old and 69% of patients ≥10 years old), with most patients displaying an IQ between 70 and 85 (Table 3). Results were homogenous between “verbal” and “non-verbal” IQ items. There were no signs of neurocognitive regression during follow-up. Academic achievements for patients older than 6 years old (n = 43) were comparable to the general population in 25 patients (58%), defined as normal or remedial school (for minor learning disabilities) (Table 3). Nonetheless, 11 patients (26%) required a specialized school for intellectual disability, and 7 patients (16%) required a full-time medically supervised institution. At adulthood (Table 3), 8 out of 13 patients had a good socio-professional insertion, defined as the ability to work (n = 3) or to be involved in vocation training (n = 4) or graduate education (n = 1).
Non-neurological outcome
Skeletal dysplasia progressed despite HSCT and required surgery for kyphoscoliosis and lower limb deformities in 24 (51%) and 16 patients (34%), respectively (Table 4). Some rarer complications such as thoraco-lumbar spinal cord and C1-C2 cervical cord compressions were respectively observed in 5 and 6 patients, often after 10 years of age. Progression of skeletal dysplasia with age led to a significant motor impairment (use of cane or wheelchair) at last follow-up in 17 patients (37%), including 10 of the 13 adult patients. Seven patients (all adults) completely lost the ability to walk, mainly because of hip dysplasia. Most patients also had short stature, with a median final height of 140 cm (IQR 134–146).
Sensory impairment was the second main disability, primarily with visual impairment and deafness (Table 4). Almost all patients displayed progressive corneal clouding and a corneal graft was required in 7 patients (15%) at a median age of 20 years, with significant visual improvement. Obvious clinical signs of retinal degeneration (rod-cone dystrophy) were present in 5 patients (11%, median age 20 years). Detailed multimodal imaging (comprising spectral domain optical coherence tomography and ultra-wide field autofluorescence imaging) and electrophysiological assessment (comprising full field electroretinography) were not always systematically performed. Out of 12 patients without clinical signs of retinal involvement who underwent these investigations (median age of 11.5 years old), 6 exhibited signs of retinal dystrophy. Visual acuity was ≤5/10 in half of the patients, including all patients older than 18 years except one. Hearing loss was present in 35 patients (74%) and responsible for speech delay in childhood.
Multiple causes of airway obstruction were present (Table 4). Obstructive sleep apnea (OSA) was common in older patients as already described [11], with 9 patients (20%) requiring non-invasive ventilation in our cohort. 3 patients required surgery for temporo-mandibular ankylosis and maximum mouth opening of less than 1 cm, with disappointing results. 2 patients had typical tracheal involvement with tracheal deformity as well as endoluminal infiltration. Anticipated difficult airway management during general anesthesia was frequent (36%), requiring nasal fiberoptic intubation. Tracheal extubation was often also difficult.
Almost all patients displayed thickened cardiac valves after HSCT, with a valvular stenosis or regurgitation in 34 patients (72%, Table 4). Decreased lung volume due to skeletal dysplasia was present in half of the patients and worsened with age. Nonetheless, no patient had cardio-pulmonary symptoms except the patient who died from pulmonary hypertension [10].
4 patients were treated with ERT during follow-up because of disease progression: one at 16 years of age for severe OSA and mouth opening reduction, despite a 95% donor chimerism and 50% leukocyte α-L-Iduronidase activity; one at 19 years of age due to OSA, severe tracheal stenosis and aortic valve regurgitation with left ventricle dilatation, with a 37% donor chimerism and 60% leukocyte α-L-Iduronidase activity; one at 13 years of age because of OSA and descending aortic stenosis causing upper-body systemic hypertension, despite a full donor chimerism and normal α-L-Iduronidase activity; one at 14 years for airway obstruction and pulmonary hypertension (already reported [10]). There was a striking improvement in soft tissue infiltration with a complete disappearance of OSA, but a lower efficacy for skeletal dysplasia and cardio respiratory features as already reported. No efficacy was reported for the descending aorta stenosis, with the need to implant an aortic stent.
One patient had an uncomplicated and successful spontaneous pregnancy.
Analysis of outcome according to the stem cell source used
We compared the late outcome as a function of stem cell source among recipients of bone marrow (n = 32) and cord blood (n = 16) (Table 5). Cord blood transplants were performed more recently and were mainly HLA-mismatched whereas HSCT with bone marrow source were mostly from HLA-matched donors (MSD, MUD). Median follow-up was similar between the two groups, although the IQR range in the bone marrow group was wider. Rates of GvHD, complete chimerism and normal α-L-Iduronidase activity were similar between the two groups. Neurocognitive outcomes were similar between the two groups, whereas there was a trend toward better non-neurological outcomes with cord blood, with higher height at last follow-up (p = 0.07) and less valvular disease (p = 0.09).
Discussion
Although HSCT is a validated therapeutic option for patients with MPS I-H, few studies have assessed long-term outcomes [7]. We present herein data on a large cohort of 51 patients with a median follow-up of 9 years after HSCT, including 13 patients having reached adulthood. Although neurocognitive outcome was good in half of the patients, significant disabilities remains, especially because of skeletal dysplasia and visual impairment.
A younger age at HSCT and the absence of a significant developmental delay are known to be associated with a better neurocognitive outcome [1, 3]. DQ is often assessed in France using the Brunet-Lezine scale, but results are often heterogeneous in MPS I-H patients, with better preserved coordination and sociability, and poorer results for postural and language criteria because of hearing loss and skeletal dysplasia [1]. This scale may not reflect their actual cognitive development.
Neuro-developmental outcomes are difficult to assess retrospectively, especially in MPS I-H patients because of confounding factors (hearing loss, visual impairment, motor disabilities). We used semi-quantitative assessments to reflect global neurocognitive outcomes. Neurocognitive outcomes were satisfactory in two-thirds of patients, in line with previous studies [3], and more than half could follow an education in normal or remedial schools. Most patients required a variable degree of assistance in daily activities due to motor and sensory disabilities. Although imperfect, one has to consider the severity of the disease if left untreated [12]. As a comparison, 4 MPS I-H patients could not receive HSCT during the same period (DQ < 70, n = 2; no compatible donor, n = 1; age >30 months, n = 1), and were treated with ERT from a median age of 17 months. After a median follow-up of 10 years, all are severely disabled (unevaluable IQ: n = 4/4; no speech: n = 2/4; no reading/writing: n = 4/4), all require a full-time institution (vs. 16% of HSCT-treated patients) and one died at 9 years of age.
In our study, we did not observe significant differences in cognitive and non-neurological outcomes, chimerism and α-L-Iduronidase enzymatic activity according to the type of stem cell source. While previous studies have suggested that cord blood transplants were associated with better donor chimerism and higher α-L-Iduronidase activity as compared to HSCT performed with bone marrow [13, 14], a recent publication by Orchard et al. showed similar leukocytes and plasma α-L-Iduronidase activity between bone marrow and cord blood HSCT recipients after a longer follow-up [15]. In our study, we did not observe differences in donor chimerism and α-L-Iduronidase enzymatic activity according to the stem cell source, but our cohort was smaller and cord blood was used in only one third of transplants.
As the correction of the neurological features are mediated by corrected microglial cells from the bone marrow and by their secretion of α-L-Iduronidase into the brain [1], it is likely that the patients with a low leukocyte α-L-Iduronidase activity also have a low intra-cerebral activity. A low cerebral α-L-Iduronidase activity despite HSCT was demonstrated in a mouse model of Hurler disease [16]. Serum α-L-Iduronidase activity could better reflect the secretion and enzyme level in tissues. It was only available in 6 patients, and was much lower than the leukocyte enzymatic activity. In addition, a low enzymatic activity could also worsen the hearing loss and vision impairment, as suggested by others [3], and therefore could have an impact on the cognitive outcome.
Hydrocephalus is a known complication of MPS I-H due to cerebrospinal fluid (CSF) resorption impairment, and some studies described that HSCT, but not ERT alone, could prevent its occurrence [3, 12]. Hydrocephalus always occurred prior to HSCT or in the months immediately after HSCT, and with no occurrence during later follow-up, as described [3].
HSCT is unable to fully prevent the development of visceral complications, although milder compared to historical cohorts. In line with previous studies [3, 7], skeletal dysplasia and vision impairment are the two main handicaps in our cohort, likely because of the poor vascularization of bone and cornea. Complex surgeries with prolonged rehabilitation are required, which can significantly impact on neurocognitive development. In older patients as well as in almost all adult patients, a severe reduction of mobility is present, mostly because of hip dysplasia. Finally, height remains low despite HSCT (final height: 140 cm), although it was higher than in previously published cohorts treated with ERT alone (<−3 SD with shorter follow-up [17]), and in our 4 patients without HSCT after a median follow-up of 10 years (median height −4.5 SD, including one adult patient with a final height of 123 cm).
The second most disabling complication is visual impairment. All patients experienced corneal clouding with a progressive decrease of visual acuity and corneal grafts were indicated in the older patients. Retinal dystrophy is present in older patients and can be difficult to assess due to corneal clouding; it is responsible for visual field restriction, hemeralopia, and can eventually worsen visual acuity [18]. In contrast to the hearing loss that persists after HSCT, airway obstruction rapidly improved following ERT and HSCT but can recur post-HSCT, with OSA and anticipated difficult airway management during anesthesia. Some patients resumed ERT with good efficacy, allowing a weaning from non-invasive ventilation. Finally, although most patients displayed reduced lung volume and valvular disease, this was often mild and without clinical symptoms in most of them.
Despite prolonged survival and a favorable neurocognitive outcome, HSCT is still associated with significant morbidity and mortality including rejection and GvHD [13]. 14% of our patients displayed chronic GvHD, which is in line with previous studies (rates ranging from 5.6 to 16%) [13, 14, 19]. Almost all deaths described in our cohort were attributed to TRM, with two patients having experienced fatal chronic GvHD. Nonetheless, no surviving patients still required immunosuppressive therapy at last follow-up. Gene therapy using lentiviral transduction of autologous hematopoietic stem cells could avoid the occurrence of GvHD, reduce the delay between diagnosis and HSCT and allow supraphysiological α-L-Iduronidase activity levels. Studies in mice treated with gene therapy have shown that the level of α-L-Iduronidase in brain is much higher than what can be obtained using HSCT [16]. Recently published results in patients confirmed the safety and the supraphysiological α-L-Iduronidase activity level in both blood and CSF, as well as a striking reduction of GAG accumulation, again both in blood and CSF [2].
Finally, although we did not notice the high rate of severe depression and acute psychotic episode described by others [7], it is clear that the high disease burden remaining after HSCT has a major impact on the quality of life of the patients and could lead to depression.
Our study provides retrospective data on long-term outcome after HSCT in a large cohort of MPS I-H. Currently, HSCT remains the standard of care to both prolong survival, prevent neurological decline and slow the progression of the visceral features of the disease despite severe residual motor and sensory handicaps. Future studies will assess if supraphysiological enzymatic correction obtained using gene therapy will translate in better long-term outcome.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Clarke L. Mucopolysaccharidosis type I. In: Adam MP, Ardinger HH, Pagon RA, et al. GeneReviews®. Seattle: University of Washington; 2002.
Gentner B, Tucci F, Galimberti S, Fumagalli F, De Pellegrin M, Silvani P, et al. Hematopoietic stem- and progenitor-cell gene therapy for hurler syndrome. N Engl J Med. 2021;385:1929–40.
Aldenhoven M, Wynn RF, Orchard PJ, O’Meara A, Veys P, Fischer A, et al. Long-term outcome of Hurler syndrome patients after hematopoietic cell transplantation: an international multicenter study. Blood. 2015;125:2164–72.
Wynn R, Schulz A. Inborn Errors of Metabolism and Osteopetrosis. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies. 7th ed. Ch. 90. Cham (CH): Springer; 2019.
Jameson E, Jones S, Wraith JE. Enzyme replacement therapy with laronidase (Aldurazyme®) for treating mucopolysaccharidosis type I. Cochrane Database Syst Rev. 2013;6:CD009354.
Kakkis ED, Muenzer J, Tiller GE, Waber L, Belmont J, Passage M, et al. Enzyme-replacement therapy in mucopolysaccharidosis I. N Engl J Med. 2001;344:182–8.
Guffon N, Pettazzoni M, Pangaud N, Garin C, Lina-Granade G, Plault C, et al. Long term disease burden post-transplantation: three decades of observations in 25 Hurler patients successfully treated with hematopoietic stem cell transplantation (HSCT). Orphanet J Rare Dis. 2021;16:60.
Muenzer J, Wraith JE, Clarke LA, and the International Consensus Panel on the Management and Treatment of Mucopolysaccharidosis I. Mucopolysaccharidosis I: management and treatment guidelines. Pediatrics. 2009;123:19–29.
Bunge S, Kleijer WJ, Steglich C, Beck M, Zuther C, Morris CP, et al. Mucopolysaccharidosis type I: identification of 8 novel mutations and determination of the frequency of the two common α-L-iduronidase mutations (W402X and Q70X) among European patients. Hum Mol Genet. 1994;3:861–6.
Valayannopoulos V, de Blic J, Mahlaoui N, Stos B, Jaubert F, Bonnet D, et al. Laronidase for cardiopulmonary disease in hurler syndrome 12 years after bone marrow transplantation. Pediatrics. 2010;126:e1242–7.
Moreau J, Brassier A, Amaddeo A, Neven B, Caillaud C, Chabli A, et al. Obstructive sleep apnea syndrome after hematopoietic stem cell transplantation in children with mucopolysaccharidosis type I. Mol Genet Metab. 2015;116:275–80.
Eisengart JB, Rudser KD, Xue Y, Orchard P, Miller W, Lund T, et al. Long-term outcomes of systemic therapies for Hurler syndrome: an international multicenter comparison. Genet Med. 2018;20:1423–9.
Boelens JJ, Wynn RF, O’Meara A, Veys P, Bertrand Y, Souillet G, et al. Outcomes of hematopoietic stem cell transplantation for Hurler’s syndrome in Europe: a risk factor analysis for graft failure. Bone Marrow Transpl. 2007;40:225–33.
Boelens JJ, Aldenhoven M, Purtill D, Ruggeri A, DeFor T, Wynn R, et al. Outcomes of transplantation using various hematopoietic cell sources in children with Hurler syndrome after myeloablative conditioning. Blood. 2013;121:3981–7.
Orchard PJ, Gupta A, Eisengart JB, Polgreen LE, Pollard LM, Braunlin E, et al. Hematopoietic stem cell transplant for Hurler Syndrome: does using bone marrow or umbilical cord blood make a difference? Blood Adv. 2022;6:6023–7.
Visigalli I, Delai S, Politi LS, Di Domenico C, Cerri F, Mrak E, et al. Gene therapy augments the efficacy of hematopoietic cell transplantation and fully corrects mucopolysaccharidosis type I phenotype in the mouse model. Blood 2010;116:5130–9.
Wraith JE, Beck M, Lane R, van der Ploeg A, Shapiro E, Xue Y, et al. Enzyme replacement therapy in patients who have mucopolysaccharidosis i and are younger than 5 years: results of a multinational study of recombinant human -L-Iduronidase (Laronidase). Pediatrics. 2007;120:e37–46.
Ashworth JL, Biswas S, Wraith E, Lloyd IC. The ocular features of the mucopolysaccharidoses. Eye. 2006;20:553–63.
Wadhwa A, Chen Y, Holmqvist A, Wu J, Ness E, Parman M, et al. Late mortality after allogeneic blood or marrow transplantation for inborn errors of metabolism: a report from the blood or marrow transplant survivor study-2 (BMTSS-2). Biol Blood Marrow Transpl. 2019;25:328–34.
Acknowledgements
The authors would like to acknowledge the contributions of the teams in each center, the physiotherapy and occupational therapy teams, « Relais handicap rare » team taking care of the patients, and of course the patients and their families.
Author information
Authors and Affiliations
Contributions
The design of the study was performed by AG and AB. Data collection was performed for AG, AC, JP, ASG, MT and DL in their respective centers. MR reviewed data on ophthalmological findings. Supervision was performed by AB. Data analysis was performed by AG, AB and MC. Original draft was written by AG and extensive reviewing and editing was performed by AB and the rest of the authors in their domain of expertise.
Corresponding author
Ethics declarations
Competing interests
AB has received fees and travel support for conferences from Sanofi-Genzyme. DL has received fees for boards from Sanofi-Genzyme and Amicus. Other authors declare no competing interests.
Ethics approval
Patients or patients’ parents/legal guardians provided written consent (RADICO National study approved by independent ethics committee).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gardin, A., Castelle, M., Pichard, S. et al. Long term follow-up after haematopoietic stem cell transplantation for mucopolysaccharidosis type I-H: a retrospective study of 51 patients. Bone Marrow Transplant 58, 295–302 (2023). https://doi.org/10.1038/s41409-022-01886-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01886-1