Abstract
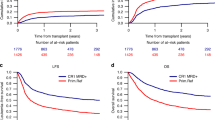
Measurable residual disease (MRD) assessment before allogeneic hematopoietic cell transplantation (HCT) may help physicians to identify a subgroup of patients at high risk of relapse for de novo acute myeloid leukemia (AML) but its relevance among patients affected by secondary AML (sAML) is still unknown. We assessed the impact of MRD among 318 adult patients with sAML who received an allogeneic HCT in first complete remission. At the time of HCT, a total of 208 (65%) patients achieved MRD negativity, while 110 (35%) had positive MRD. 2-year overall survival (OS) was 58.8 % (95% CI 52.2–64.9) with leukemia-free survival (LFS) of 50.0 % (95% CI 43.7–56.1), relapse incidence of 34.2% (95% CI 28.4–40.1) and non-relapse mortality (NRM) of 23.3 % (95% CI 19–27.7) for the entire cohort. In multivariate analysis, HCT recipients with KPS ≥ 90 experienced less disease recurrence (HR 0.61, 95% CI 0.4–0.94) with better LFS (HR 0.63, 95% CI 0.44–0.89) and OS (HR 0.58, 95% CI 0.39–0.86). There were no differences in major clinical endpoints between patients with MRD-positive and MRD-negative status at the time of HCT. Pre-transplantation assessment of MRD was not informative on post-HCT outcomes in this retrospective registry-based analysis among patients affected by sAML.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Published data are available on specific request via email to the corresponding author.
References
Brüggemann M, Raff T, Flohr T, Gokbuget N, Nakao M, Droese J, et al. German Multicenter Study Group for Adult Acute Lymphoblastic Leukemia. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood. 2006;107:1116–23.
Bassan R, Spinelli O, Oldani E, Intermesoli T, Tosi M, Peruta B, et al. Improved risk classification for risk-specific therapy based on the molecular study of minimal residual disease (MRD) in adult acute lymphoblastic leukemia (ALL). Blood. 2009;113:4153–62.
Vora A, Goulden N, Wade R, Mitchell C, Hancock J, Hough R, et al. Treatment reduction for children and young adults with low-risk acute lymphoblastic leukaemia defined by minimal residual disease (UKALL 2003): a randomised controlled trial. Lancet Oncol. 2013;14:199–209.
Short NJ, Zhou S, Fu C, Berry DA, Walter RB, Freeman SD, et al. Association of measurable residual disease with survival outcomes in patients with acute myeloid leukemia: a systematic review and meta-analysis. JAMA Oncol. 2020;6:1890–9.
Kohlmann A, Nadarajah N, Alpermann T, Grossmann V, Schindela S, Dicker f, et al. Monitoring of residual disease by next-generation deep-sequencing of RUNX1 mutations can identify acute myeloid leukemia patients with resistant disease. Leukemia. 2014;1:129–37.
Jongen-Lavrencic M, Grob T, Hanekamp D, Kavelaars FG, al Hinai A, Zeilemaker A, et al. Molecular minimal residual disease in acute myeloid leukemia. N Engl J Med. 2018;378:1189–99.
Schuurhuis GJ, Heuser M, Freeman S, Béné MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91.
Terwijn M, van Putten WL, Kelder A, van der Velden VH, Brooimans RA, Pabst T, et al. High prognostic impact of flow cytometric minimal residual disease detection in acute myeloid leukemia: data from the HOVON/SAKK AML 42A study. J Clin Oncol. 2013;31:3889–97.
Loken MR, Alonzo TA, Pardo L, Gerbing RB, Raimondi SC, Hirsch BA, et al. Residual disease detected by multidimensional flow cytometry signifies high relapse risk in patients with de novo acute myeloid leukemia: a report from Children’s Oncology Group. Blood. 2012;120:1581–8.
Freeman SD, Hills RK, Virgo P, Khan N, Couzens S, Dillon R, et al. Measurable residual disease at induction redefines partial response in acute myeloid leukemia and stratifies outcomes in patients at standard risk without NPM1 mutations. J Clin Oncol. 2018;36:1486–97.
Freeman SD, Virgo P, Couzens S, Grimwade D, Russel N, Hills RK, et al. Prognostic relevance of treatment response measured by flow cytometric residual disease detection in older patients with acute myeloid leukemia. J Clin Oncol. 2013;31:4123–31.
Langebrake C, Creutzig U, Dworzak M, Hrusak O, Mejstrikova E, Griesinger F, et al. Residual disease monitoring in childhood acute myeloid leukemia by multiparameter flow cytometry: the MRD-AML-BFM Study Group. J Clin Oncol. 2006;24:3686–92.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A.UK National Cancer Research Institute AML Working Group et al. Assessment of minimal residual disease in standard-risk AML. N Engl J Med. 2016;374:422–33.
Buckley SA, Wood BL, Othus M, Hourigan CS, Ustun C, Linden MA, et al. Minimal residual disease prior to allogeneic hematopoietic cell transplantation in acute myeloid leukemia: a meta-analysis. Haematologica. 2017;102:865–73.
Walter RB, Gooley TA, Wood BL, Milano F, Fang M, Sorror ML, et al. Impact of pretransplantation minimal residual disease, as detected by multiparametric flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute myeloid leukemia. J Clin Oncol. 2011;29:1190–7.
Balsat M, Renneville A, Thomas X, de Botton S, Caillot D, Marceau A, et al. Postinduction minimal residual disease predicts outcome and benefit from allogeneic stem cell transplantation in acute myeloid leukemia with NPM1 mutation: a study by the Acute Leukemia French Association Group. J Clin Oncol. 2017;35:185–93.
Gilleece MH, Labopin M, Yakoub-Agha I, Volin L, Socié G, Ljungman P, et al. Measurable residual disease, conditioning regimen intensity, and age predict outcome of allogeneic hematopoietic cell transplantation for acute myeloid leukemia in first remission: A registry analysis of 2292 patients by the Acute Leukemia Working Party European Society of Blood and Marrow Transplantation. Am J Hematol. 2018;93:1142–52.
Leung W, Pui CH, Coustan-Smith E, Yang J, Pei D, Gan K, et al. Detectable minimal residual disease before hematopoietic cell transplantation is prognostic but does not preclude cure for children with very-high-risk leukemia. Blood. 2012;120:468–72.
Oran B, Jorgensen JL, Marin D, Wang S, Ahmed S, Alousi AM, et al. Pre-transplantation minimal residual disease with cytogenetic and molecular diagnostic features improves risk stratification in acute myeloid leukemia. Haematologica. 2017;102:110–7.
Ustun C, Wiseman AC, Defor TE, Yohe S, Linden MA, Oran B, et al. Achieving stringent CR is essential before reduced-intensity conditioning allogeneic hematopoietic cell transplantation in AML. Bone Marrow Transpl. 2013;48:1415–20.
Anthias C, Dignan F, Morilla R, Morilla A, Ethell ME, Potter MN, et al. Pre-transplant MRD predicts outcome following reduced-intensity and myeloablative allogeneic hemopoietic SCT in AML. Bone Marrow Transpl. 2014;49:679–83.
Canaani J, Labopin M, Huang XJ, Ciceri F, Van Lint MT, Bruno B, et al. Minimal residual disease status predicts outcome of acute myeloid leukaemia patients undergoing T‐cell replete haploidentical transplantation. An analysis from the Acute Leukaemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT). Br J Hematol. 2018;183:411–20.
Othus M, Wood BL, Stirewalt DL, Estey EH, Petersdorf SH, Appelbaum FR, et al. Effect of measurable (‘minimal’) residual disease (MRD) information on prediction of relapse and survival in adult acute myeloid leukemia. Leukemia. 2016;30:2080–3.
Chen X, Xie H, Wood BL, Walter RB, Pagel JM, Becker PS, et al. Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. J Clin Oncol. 2015;33:1258–64.
Gilleece MH, Shimoni A, Labopin M, Robinson S, Beelen D, Sociè G, et al. Measurable residual disease status and outcome of transplant in acute myeloid leukemia in second complete remission: a study by the acute leukemia working party of the EBMT. Blood Cancer J. 2021;11:88.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, revised 4th edition. (Eds), International Agency for Research on Cancer (IARC), Lyon 2017.
Granfeldt Østgård LS, Medeiros BC, Sengeløv H, Nørgaard M, Andersen MK, Dufva IH, et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a national population-based cohort study. J Clin Oncol. 2015;33:3641–9.
Kayser S, Döhner K, Krauter J, Köhne CH, Horst HA, Held G, et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood. 2011;117:2137–45.
Schmaelter AK, Labopin M, Socié G, Itälä-Remes M, Blaise D, Yakoub-Agha I, et al. Inferior outcome of allogeneic stem cell transplantation for secondary acute myeloid leukemia in first complete remission as compared to de novo acute myeloid leukemia. Blood Cancer J. 2020;10:1–9.
Ciurea S, Labopin M, Sociè G, Volin L, Passweg J, Chevalier P, et al. Relapse and survival after transplantation for complex karyotype acute myeloid leukemia: a report from the acute leukemia working party of the European society for blood and marrow transplantation and the university of Texas MD Anderson cancer center. Cancer 2018;124:2134–41.
Kanate AS, Nagler A, Savani BN. Summary of scientific and statistical methods, study endpoints and definitions for observational and registry-based studies in hematopoietic. Cell Transplant Clin Hematol Int. 2020;2:2–4.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: i. the 2014 diagnosis and staging working group report. Biol Blood Marrow Transpl. 2005;11:945–55.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP–EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1.
Nagler A, Baron F, Labopin M, Polge E, Esteve J, Bazarbachi A, et al. Measurable residual disease (MRD) testing for acute leukemia in EBMT transplant centers: a survey on behalf of the ALWP of the EBMT. Bone Marrow Transpl. 2021;56:218–24.
Tazi Y, Arango JE, Zhou Y, Thomas I, Bernard E, Gilkes A, et al. A unified classification and risk stratification algorithm to support clinical decisions in acute myeloid leukemia. Haematologica. 2021;406-4:S133.
Morsink LM, Othus M, Bezerra ED, Wood BL, Fang M, Sandmaier BM, et al. Impact of pre-transplant measurable residual disease on outcome of allogeneic hematopoietic cell transplantation in adult monosomal karyotype AML. Leukemia. 2020;34:1577–87.
Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T. Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia. 2004;18:120–5.
Ornstein MC, Mukherjee S, Mohan S, Elson P, Tiu RV, Saunthararajah Y, et al. Predictive factors for latency period and a prognostic model for survival in patients with therapy-related acute myeloid leukemia. Am J Hematol. 2014;89:168–73.
Stölzel F, Pfirrmann M, Aulitzky WE, Kaufmann M, Bodenstein H, Bornhäuser M, et al. Risk stratification using a new prognostic score for patients with secondary acute myeloid leukemia: results of the prospective AML96 trial. Leukemia 2011;25:420–8.
Kröger N, Brand R, van Biezen A, Zander A, Dierlamm J, Niederwieser D, et al. Risk factors for therapy-related myelodysplastic syndrome and acute myeloid leukemia treated with allogeneic stem cell transplantation. Haematologica 2009;94:542.
Sengsayadeth S, Labopin M, Boumendil A, Finke J, Ganser A, Stelljes M, et al. Transplant outcomes for secondary acute myeloid leukemia: acute leukemia working party of the european society for blood and bone marrow transplantation study. Biol Blood Marrow Transpl. 2018;24:1406–14.
Fianchi L, Pagano L, Piciocchi A, Candoni A, Gaidano G, Breccia M, et al. Characteristics and outcome of therapy-related myeloid neoplasms: Report from the Italian network on secondary leukemias. Am J Hematol. 2015;90:E80–5.
Saraceni F, Labopin M, Forcade E, Kroger N, Socié G, Niittyvuopio R, et al. Allogeneic stem cell transplant in patients with acute myeloid leukemia and karnofsky performance status score less than or equal to 80%: A study from the acute leukemia working party of the European Society for Blood and Marrow Transplantation (EBMT). Cancer Med. 2021;10:23–33.
Carrè M, Poercher R, Finke J, Ehninger G, Koster L, Beelen D, et al. Role of age and hematopoietic cell transplantation-specific comorbidity index in myelodysplastic patients. Biol Blood Marrow Transpl. 2020;3:451–7.
Wedding U, Röhrig B, Klippstein A, Fricke HJ, Sayer HG, Höffken K. Impairment in functional status and survival in patients with acute myeloid leukaemia. J Cancer Res Clin Oncol. 2006;132:665.
Deschler B, Binek K, Ihorst G, Marks R, Wasch R, Bertz H, et al. Prognostic factor and quality of life analysis in 160 patients aged > or =60 years with hematologic neoplasias treated with allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2010;16:967–75.
Buchner T, Berdel WE, Haferlach C, Haferlach T, Schnittger S, Muller-Tidow C, et al. Age-related risk profile and chemotherapy dose response in acute myeloid leukemia: a study by the German Acute Myeloid Leukemia Cooperative Group. J Clin Oncol. 2009;27:61–69.
Kyriakou C, Boumendil A, Finel H, Schmitz N, Andersen NS, Blaise D, et al. The impact of advanced patient age on mortality after allogeneic hematopoietic cell transplantation for non-hodgkin lymphoma: a retrospective study by the European society for blood and marrow transplantation lymphoma working party. Biol Blood Marrow Transpl. 2019;25:86–93.
Muffly L, Pasquini MC, Martens MC, Brazauskas R, Zhu X, Adekola K, et al. Increasing use of allogeneic hematopoietic cell transplantation in patients aged 70 years and older in the United States. Blood. 2017;130:1156–64.
Ringden O, Boumendil A, Labopin M, Canaani J, Beelen D, Ehninger G, et al. Outcome of allogeneic hematopoietic stem cell transplantation in patients age >69 years with acute myelogenous leukemia: on behalf of the acute leukemia working party of the European society for blood and marrow transplantation. Biol Blood Marrow Transpl. 2019;25:1975–83.
Milano F, Gooley T, Wood B, Woolfrey A, Flowers ME, Doney K, et al. Cord-blood transplantation in patients with minimal residual disease. N Eng J Med. 2016;375:944–55.
Morsink LM, Sandmaier BM, Othus M, Palmieri R, Granot N, Bezerra ED, et al. Conditioning intensity, pre-transplant flow cytometric measurable residual disease, and outcome in adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Cancers. 2020;12:2339.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of Allogeneic Transplantation for acute myeloid leukemia with Genomic evidence of residual disease. J Clin Oncol. 2021;38:1273–84.
Liu FJ, Cheng WY, Lin XJ, Wang SY, Jiang TY, Ma TT, et al. Measurable residual disease detected by multiparameter Flow Cytometry and Sequencing improves prediction of Relapse and survival in Acute Myeloid Leukemia. Front Oncol. 2021;11:677833. https://doi.org/10.3389/fonc.2021.677833.
Brooimans RA, van der Velden VHJ, Boeckx N, Boeckx N, Slomp J, Preijers F, et al. Immunophenotypic measurable residual disease (MRD) in acute myeloid leukemia: is multicentric MRD assessment feasible? Leuk Res. 2019;76:39–47.
Paras G, Morsink LM, Othus M, Milano F, Sandmaier B, Zarling LC, et al. Conditioning intensity and peritransplant flow cytometric MRD dynamics in adult AML. Blood. 2022;139:1694–706.
Zhou Y, Othus M, Walter RB, Estey EH, Wu D, Wood BL, et al. Deep NPM1 sequencing following allogeneic hematopoietic cell transplantation improves risk assessment in adults with NPM1-mutated AML. Biol Blood Marrow Transpl. 2018;24:1615–20.
Lesieur A, Thomas X, Nibourel O, Boissel N, Fenwarth L, De Botton S, et al. Minimal Residual Disease monitoring in acute myeloid leukemia with non A/B/D-NPM1 mutations by digital polymerase chain reaction: feasibility and clinical use. Haematologica. 2021;106:1767–9.
Mannina D, Badbaran A, Wolschke C, Klyuchnikov E, Christopeit M, Fehse B, et al. Digital-droplet PCR assays for IDH, DNMT3A and driver mutations to monitor after allogeneic stem cell transplantation minimal residual disease of myelofibrosis. Bone Marrow Transpl. 2022;57:510–2.
Levine RL, Valk PJM. Next-generation sequencing in the diagnosis and minimal residual disease assessment of acute myeloid leukemia. Haematologica 2019;104:868–71.
Thol F, Gabdoulline R, Liebich A, Klement P, Schiller J, Kandziora C, et al. Measurable residual disease monitoring by NGS before allogeneic hematopoietic cell transplantation in AML. Blood. 2018;132:1703–13.
Kim T, Moon JH, Ahn JS, Kim YK, Lee SS, Ahn SY, et al. Next-generation sequencing-based posttransplant monitoring of acute myeloid leukemia identifies patients at high risk of relapse. Blood. 2018;132:1604–13.
Author information
Authors and Affiliations
Contributions
EM analyzed the data and wrote the manuscript; ML contributed to the statistical analysis. AN, JE, and MM critically appraised the paper. All the Authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maffini, E., Labopin, M., Beelen, D.W. et al. Measurable residual disease (MRD) status before allogeneic hematopoietic cell transplantation impact on secondary acute myeloid leukemia outcome. A Study from the Acute Leukemia Working Party (ALWP) of the European society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant 57, 1556–1563 (2022). https://doi.org/10.1038/s41409-022-01748-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01748-w
This article is cited by
-
Factors predicting survival following alloSCT in patients with therapy-related AML and MDS: a multicenter study
Bone Marrow Transplantation (2023)
-
Significance of measurable residual disease in adults with secondary acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2022)
-
Measurable residual disease for secondary acute myeloid leukemia prior to allogeneic hematopoietic cell transplantation: does it make a difference?
Bone Marrow Transplantation (2022)