Abstract
Post-transplant cyclophosphamide (PTCy) has emerged as a promising graft-versus-host disease (GvHD) prophylaxis in allogeneic hematopoietic stem cell transplantation (allo-HSCT). However, no studies have reported the efficacy of a GvHD prophylaxis based on PTCy with sirolimus (Sir-PTCy) in patients with acute myeloid leukemia (AML). In this retrospective study, we analyze the use of sirolimus in combination with PTCy, with or without mycophenolate mofetil (MMF), on 242 consecutive adult patients with AML undergoing a myeloablative first allo-HSCT from different donor types, in three European centers between January 2017 and December 2020. Seventy-seven (32%) patients received allo-HSCT from HLA-matched sibling donor, 101 (42%) from HLA-matched and mismatched unrelated donor, and 64 (26%) from haploidentical donor. Except for neutrophil and platelet engraftment, which was slower in the haploidentical cohort, no significant differences were observed in major transplant outcomes according to donor type in univariate and multivariate analysis. GvHD prophylaxis with Sir-PTCy, with or without MMF, is safe and effective in patients with AML undergoing myeloablative allo-HSCT, resulting in low rates of transplant-related mortality, relapse/progression, and acute and chronic GvHD in all donor settings.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is an increasingly offered and potentially curative option for patients with acute myeloid leukemia (AML). Regarding GvHD prophylaxis, the success of post-transplant cyclophosphamide (PTCy) in the haploidentical setting has led to the expansion of its use also in recipients of allo-HSCT from HLA-matched sibling donor (MSD) and unrelated donor (MUD) [1, 2]. PTCy combined with additional immunosuppression, mainly calcineurin inhibitors (CNI), has proved to reduce the risk of severe GvHD [3,4,5,6,7]. Looking for a favorable balance between safety and efficacy, encouraging results have recently been reported with CNI-free approaches based on PTCy and sirolimus (Sir-PTCy) [8,9,10,11,12]. Sirolimus demonstrated a favorable toxicity profile, particularly in terms of reduced incidence of acute renal failure [13] and improved regulatory T cells reconstitution [14, 15]. In fact, two large real-life studies have recently reported promising results with Sir-PTCy, with or without mycophenolate mofetil (MMF), as GvHD prophylaxis in patients with hematologic malignancies undergoing allo-HSCT from all donor sources [16, 17]. However, as far as we know, to date, no studies have reported the efficacy of such GvHD prophylaxis with Sir-PTCy restricted to patients with AML.
The aim of this study was to analyze the impact of donor type on transplant outcomes in a large series of patients with AML undergoing myeloablative first allo-HSCT using a uniform platform of GvHD prophylaxis based on Sir-PTCy.
Patients and methods
Eligibility criteria and data collection
This is an observational retrospective study. All consecutive patients with AML who received a first allo-HSCT between January 2017 and December 2020 at Hospital Universitari i Politècnic La Fe (Valencia, Spain), Hospital Clínico Universitario (Valencia, Spain), and Ospedale San Raffaele (Milan, Italy) were included in the study.
Data of patients, transplant procedures, toxicity and complications were prospectively collected in all patients and then settled in a computerized database. Clinical charts were additionally reviewed for inconsistent or missing data.
Donor selection
For donor selection, MSD was the primary option. If not available, a MUD registry search was started. If a matched donor ≥9/10 was not readily available, the best related haploidentical donor (Haplo) was selected according to the following: absence of recipient HLA antibodies against donor antigens, male sex, younger age, matched cytomegalovirus (CMV) serostatus, matched ABO group, and, for female donors, lowest number of prior pregnancies.
Conditioning regimens and GvHD prophylaxis
Conditioning regimens and GvHD prophylaxis schemes used at the three centers have already been described elsewhere [16, 17]. Sirolimus was started on day +5, with dose modifications to achieve targeted plasma levels between 8 and 14–16 ng/mL, and, in the absence of GvHD or relapse, was gradually tapered from day +90 and finally discontinued on day +150/+180.
All conditioning regimens used in the present study are considered myeloablative according to the latest definitions [18, 19].
Eight patients transplanted at San Raffaele received a single dose of anti-thymocyte globulin 5 mg/Kg on day +5 according to center guidelines due to high graft content of CD3+ cells (≥3 ×108/Kg) [20].
Supportive care
Supportive care measures have already been described elsewhere [16, 17]. CMV prophylaxis with letermovir at a daily dose of 480 mg from day 0 to +100 was implemented at San Raffaele starting from March 2019 in CMV-seropositive recipients [21]. All patients in the Spanish centers received granulocyte colony-stimulating factor (filgrastim) 5 mcg/Kg/day from day +7 until absolute neutrophil count >1 ×109/L for three consecutive days, while this strategy was more recently adopted in San Raffaele (starting from May 2020).
Definitions
Patients were classified at the time of transplantation according to DRI [22, 23] and the 2017 revised European LeukemiaNet (ELN) genetic risk stratification [24]. Disease status and minimal residual disease (MRD) at the time of transplant were defined according to the ELN recommendations [24, 25]. MRD monitoring was performed with multiparameter flow cytometry or standardized quantitative PCR assays [24, 25]. Comorbidities were evaluated according to the HCT-CI [26]. Post-transplant hematological response and MRD were evaluated at day +30, +90, +180, and +365. Hematologic relapse was defined according to the 2017 ELN recommendations [24]. Myeloid engraftment was defined as the first of 3 consecutive days with neutrophil counts ≥0.5 ×109/L after transplantation. Platelet engraftment was defined as the first of 7 consecutive days with platelet counts ≥20 ×109/L without platelet transfusions. Clinical diagnosis and grading of acute GvHD (aGvHD) and chronic GvHD (cGvHD) were made according to the Glucksberg criteria [27] and the National Institutes of Health consensus criteria [28], respectively. CMV DNAemia and disease [29], Epstein-Barr virus (EBV) DNAemia [30], invasive fungal infection [31], and BK polyomavirus-associated hemorrhagic cystitis [32] were diagnosed according to consensus criteria. Toxicities were graded using NCI Common Toxicity Criteria version 5.0 except for SOS, which was graded using the EBMT criteria [33].
Statistical analysis
Endpoints of the study were leukemia-free survival (LFS), overall survival (OS), graft-versus-host-free/relapse-free survival (GRFS), transplant-related mortality (TRM), cumulative incidence of relapse/progression (CIR), cumulative incidence of neutrophils and platelet engraftment, and cumulative incidence of aGvHD and cGvHD. Last follow-up was considered the 1st of July 2021. Unadjusted time-to-event analyses were performed using the Kaplan-Meier estimate [34], and, for comparisons, the log-rank tests [35]. LFS was defined as the time to death or relapse/progression, whichever came first. OS was defined as the time from transplant to death from all causes. For the analysis of GRFS, grade III-IV aGvHD, moderate-to-severe cGvHD, relapse, graft failure, and death were considered uncensored events. The probabilities of engraftment, TRM, GvHD, CIR, SOS, CMV DNAemia, and hemorrhagic cystitis were calculated using the competing risk structure [34, 35]. Competing risks data were considered as follows: for myeloid and platelet engraftment, early death or second allo-HSCT with no evidence of engraftment; for aGvHD, relapse before aGvHD or death without aGvHD before day +100; for cGvHD, death without development of cGvHD or relapse before the development of cGvHD; for TRM, relapse; for CIR, death with no previous relapse; and for other post-transplant events, death or relapse with no previous event. Patient and transplantation characteristics according to donor type were compared using the chi-square test for categorical variables and the Wilcoxon rank-sum test for continuous variables. A 95% confidence interval (95% CI) was considered. A p-value lower than 0.05 was interpreted as significant. The Cox proportional hazard model or the Gray method for competing events were used for multivariate analysis [36]. All factors known to influence outcome and factors associated with a univariate analysis p-value <0.10 were first included in the model; a stepwise backward procedure was used with a cut-off significance level of 0.10 for deleting factors from the model. The type I error rate was fixed at 0.05 for determination of factors associated with time to event. Statistical analyses were performed using R statistical software version 4.0.4 (R Development Core Team, Vienna, Austria) and SPSS version 25.0 (IBM Corporation, Armonk, NY).
Results
Patient, disease and transplant characteristics of the overall population and according to donor type are summarized in Table 1 and Table 2. Briefly, a total of 242 AML patients were included in the study, of which 77 (32%) received an allo-HSCT from MSD, 101 (42%) from MUD—including 16 9/10-HLA-mismatched unrelated donor (MMUD)—and 64 (26%) from Haplo. Median follow-up of surviving patients was 25 months (range, 6–52), with no differences according to donor type. MSD, MUD, and Haplo recipients did not differ with respect to patient and disease characteristics, except for a higher age in the MSD cohort (p = 0.02) and a slightly greater proportion of adverse genetic category in MUD recipients (p = 0.045). Regarding transplant characteristics, donor age was also higher in the MSD cohort (p < 0.0001).
Engraftment
Eight patients died without evidence of myeloid engraftment, 5 in the MUD cohort (4 infections and 1 acute renal failure), 2 in the Haplo cohort (cerebral hemorrhage and disease progression), and one from MSD (infection). Primary graft failure was only observed in 2 haploidentical recipients with high titer of anti-HLA donor specific antibodies; both patients were successfully retransplanted from the same donor after a desensitization therapy. The remaining 232 patients achieve neutrophil engraftment at a median time of 19 days (range, 13–51). Median time to neutrophil recovery for MSD, MUD, and Haplo was 17 days (range, 13–51), 19 days (range, 13–43), and 21 days (range, 13–49), respectively. No secondary graft failure was observed. All engrafted patients achieved full donor chimerism. Ten patients (2 MSD, 1 MUD, and 7 Haplo) underwent a CD34+ selected boost for secondary poor graft function. Cumulative incidence of neutrophil recovery at 60 days was lower in haploidentical recipients (p = 0.003) (Table 3) and higher (97%) and faster (16 days) in those patients receiving a higher CD34+ graft cell content (beyond percentile 75, 7.8 ×106/Kg) (p = 0.008).
Median time of platelet recovery was 25 days (range, 11–313) for the overall population and 20 days (range, 17–259) for MSD, 26 days (range, 11–257) for MUD, and 33 days (range, 17–313) for Haplo. Cumulative incidence of platelet recovery was lower in the Haplo cohort (p = 0.01) (Table 3).
There was no statistical difference in immune reconstitution data according to the type of donor (Table S1).
GvHD
There were 9 aGvHD that were diagnosed after day 100 without any difference according to donor source (2 MSD, 4 MUD, 3 Haplo; p = 0.7), with a median time to diagnosis of 129 days (range, 105–204); 3 patients developed late onset aGvHD after infusion of a CD34-selected boost administered due to poor graft function.
Fifteen patients developed an overlap cGvHD in our series at a median time of 155 days (range, 79–538). No statistical difference was observed according to donor groups (4 MSD, 3, 8 Haplo; p = 0.2). Three of these patients developed the condition after infusion of a CD34-selected stem cell boost for poor graft function, and two patients after respectively 3 and 4 months of therapy with a FLT3-inhibitor.
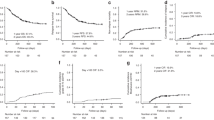
Cumulative incidence of aGvHD and cGvHD according to donor type are displayed in Table 3. There was no statistical difference in the incidence and pattern of acute or chronic GvHD according to donor type (Fig. 1).
Overall, aGvHD occurred in 100 (41%) patients at a median time of 37 days (range, 8–170): 44 (45%) grade I, 36 (35%) grade II, 15 (15%) grade III, and 5 (5%) grade IV. No variables were associated with an increased risk aGvHD in multivariate analysis.
Overall, cGvHD occurred in 100 (41%) patients at a median time of 173 days (range, 59–930). According to the NIH classification, 35 (35%) were mild, 46 (46%) moderate, and 19 (19%) severe. Results of multivariate analysis are displayed in Table 4.
Post-transplant complications
The main post-transplant complications are detailed in Table S2. There were no differences in the cumulative incidence of these complications according to the type of donor. In multivariate analysis, busulfan-based conditioning regimen was identified as risk factor for mucositis (p < 0.0001) and hemorrhagic cystitis (p < 0.0001). Patients receiving treosulfan-based conditioning regimen had a significantly lower incidence of SOS (0.8% versus 5%; p = 0.02) in univariate analysis, but this result was not confirmed in multivariate analysis.
TRM, CIR, and survival
Thirty-four patients died without prior relapse or progression at a median time of 82 days (range, 5–1187). All causes of death according to donor type are shown in Table S3. According to the type of donor, differences in TRM were not statistically significant (Table 3 and Fig. 2). However, MSD recipients had a lower TRM compared with alternative donors in univariate analysis (8% versus 16%, p = 0.046), but this was not confirmed in multivariate analysis.
Thirty-eight patients relapsed or progressed after allo-HSCT at a median time of 7 months (range, 1–43). Extramedullary relapse occurred in 15 patients, either isolated (n = 7) or in combination with marrow relapse (n = 8), with central nervous system being the most common site involved (n = 5). Patients with extramedullary relapse did not have different characteristics than those with hematological relapse. One additional patient was diagnosed with HLA loss relapse 6 months after Haplo. We did not observe significant differences in the pattern of relapses and the CIR according to the type of donor (Table 3 and Fig. 2).
There were no statistically significant differences in OS, LFS and GRFS according to the type of donor (Table 3). Results of univariate analysis of survival outcomes are showed in Table 5.
Results of multivariate analysis are displayed in Table 4.
Discussion
The present study shows that Sir-PTCy, with or without MMF, for GvHD prophylaxis is safe and effective in patients with AML undergoing myeloablative allo-HSCT not only from Haplo but also from MSD and MUD, resulting in low rates of TRM, CIR, aGvHD, and cGvHD in all transplant settings. Patient age (≥55 years) and active disease status at allo-HSCT were the only independent risk factors found for TRM, with the latter along with MRD positive status being also associated with a higher risk of relapse/progression. The lack of statistically significant differences in TRM and relapse/progression according to the type of donor translated into an absence of significant differences also in OS, LFS, and GRFS.
Although non-randomized, this study included a real-life unselected population of AML patients who underwent first allo-HSCT with a similar CNI-free GvHD prophylaxis in three European centers during the same study period. Recently reported studies have demonstrated that this approach is not only feasible and effective after Haplo, but also in allo-HSCT from MSD and MUD for patients with a variety of hematologic malignancies [8,9,10,11,12, 16, 17]. However, to the best of our knowledge, this is the first to compare the results of such GvHD prophylaxis across different donor types in AML. Since donor selection was based primarily on availability and not on patient or disease characteristics, there were no significant differences between the three cohorts in most baseline features, with the exception of younger age in the MSD cohort and higher proportion of adverse cytogenetics in those transplanted from MUD. Regarding transplant characteristics, some additional differences were also observed. While GvHD prophylaxis was relatively homogeneous (Sir-PTCy-MMF) in the vast majority of patients (88%), 28 patients transplanted from MSD received Sir-PTCy without MMF. It should also be noted that the proportion of treosulfan-based conditioning was higher in the haploidentical cohort, while the proportion of busulfan-based conditioning and donor age were higher in the MSD cohort.
The relatively low rates of grade II-IV and grade III-IV aGvHD, as well as moderate-to-severe cGvHD, are similar to those previously reported separately in hematologic malignancies with this GvHD prophylaxis by the Italian [17] and Spanish [16] centers participating in the present study. Our results were apparently better than that reported with standard CNI-based GvHD prophylaxis [37,38,39,40,41,42] and comparable to those reported with PTCy in combination with CNI [1, 3, 43,44,45,46], particularly considering that most transplants in our series were performed with peripheral blood as stem cell source (MSD and MUD, 99%; Haplo, 94%). Interestingly, the type of donor did not have a significant impact on the incidence of aGvHD and cGvHD, with donor age (older than 40 years) and a higher CD34+ content in the graft (beyond percentile 75, 7.8 × 106/Kg) being the main variables associated with an increased risk of cGvHD in multivariate analysis.
In addition to the acceptable incidence of aGvHD and cGvHD, encouraging results were obtained in terms of CIR, TRM, OS, LFS, and GRFS when compared with other series that used PTCy in patients with AML [3, 4, 6, 38, 43], without significant differences between donor types. Notably, in our study a slower recovery of neutrophil and platelet was observed in the Haplo cohort, which, in contrast with reports from other authors [47, 48], did not translate into a higher incidence of TRM or post-transplant complications. In the same group, we documented two cases of primary graft failure and seven of secondary poor graft function requiring a CD34-selected boost, two conditions already described to be more associated with mismatched allo-HSCT [49, 50].
The fact that the median time to neutrophil and platelet recovery appears somewhat longer in our study than with CNI-based GvHD prophylaxis is likely due to PTCy. In fact, a recently reported randomized phase III trial that compared two CNI-free approaches (CD34-selected grafts and PTCy) to standard CNI-based GvHD prevention, with tacrolimus and methotrexate, showed that grafting after PTCy was slower compared to the others [51].
Our results are partially in contrast with a recent registry-based study in which patients with AML undergoing Haplo allo-HSCT displayed a higher rate of aGvHD and TRM, coupled with a lower incidence of relapse, compared to recipients of MSD and MUD [6]. In fact, other comparative studies have also suggested a superior graft-versus-leukemia effect in Haplo compared to MSD transplants for high-risk AML [52,53,54], but we were unable to demonstrate this effect in the present study. Another recent analysis that compared recipients of MUD to those of Haplo reported better outcomes with MUD in transplants with reduced-intensity conditioning but not with myeloablative regimens [47].
The relatively low incidence of relapse (16% at 2 years) reported in the present study, despite the considerable number of patients transplanted with active disease (15%) or ≥CR2 (19%), should be highlighted. Although conflicting results have been reported by other authors regarding the impact of conditioning intensity on the risk of relapse [55,56,57,58], our GvHD prophylaxis in combination with myeloablative conditioning showed potent antileukemic efficacy and was well tolerated even in older patients with comorbidities. Other alternative or complementary explanations to consider could be the possible synergistic effect of Sir-PTCy on the in vivo expansion of regulatory T cells in order maintain a balance between GvHD and disease recurrence [15, 59] or the potential antileukemic effect of sirolimus [60]. Another indirect proof of the graft-versus-leukemia effect displayed with our approach could be the relatively high proportion of extramedullary relapses (15 out of 38 relapses), as an expression of the mechanisms adopted by leukemic cells to evade immune recognition. We were unable to find a correlation of extramedullary relapses with any genomic characteristic or MRD status (data available in only 140 patients).
In addition to the well-known prognostic factors such as DRI, 2017 ELN risk classification, and disease status at allo-HSCT, we also confirmed in our study the independent prognostic impact of pretransplant MRD status on the risk of relapse [61, 62]. Although very high DRI and active disease status at transplant were unfavorable variables for relapse risk and survival, a considerable fraction of these very high-risk patients could be saved with our strategy showing a 2-year LFS of respectively 29% and 40% (Table 5).
Furthermore, we were unable to detect any impact on engraftment, GvHD, and infections when MMF was omitted from GvHD prophylaxis, but it should be noted that this group consisted of only 28 patients, which represents 11% of the total and a third of those transplanted from MSD, a very small sample size to analyze its impact.
In conclusion, myeloablative allo-HSCT for AML with Sir-PTCy, with or without MMF, as GvHD prophylaxis resulted in a low incidence of relapse/progression and TRM, acceptable rates of aGvHD and cGvHD, and good survival outcomes for all donor types. Despite the absence of major differences in transplant outcomes by donor type using this GvHD prophylaxis, a possible change in donor selection algorithm for AML patients in need of an allo-HSCT should still await confirmation of our results in prospective controlled studies. Future studies should clarify whether other donor characteristics should take priority over donor type under certain circumstances in the setting of Sir-PTCy GvHD prophylaxis.
Data availability
The dataset generated and analyzed during the current study is available in the Figshare repository, https://doi.org/10.6084/m9.figshare.19688673.
References
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-Haploidentical Bone Marrow Transplantation for Hematologic Malignancies Using Nonmyeloablative Conditioning and High-Dose, Posttransplantation Cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50. https://doi.org/10.1016/j.bbmt.2008.03.005
Kanakry CG, Tsai HL, Bolaños-Meade J, Smith BD, Gojo I, Kanakry JA, et al. Single-agent GVHD prophylaxis with posttransplantation cyclophosphamide after myeloablative, HLA-matched BMT for AML, ALL, and MDS. Blood. 2014;124:3817–27. https://doi.org/10.1182/blood-2014-07-587477
Ruggeri A, Labopin M, Bacigalupo A, Afanasyev B, Cornelissen JJ, Elmaagacli A, et al. Post-transplant cyclophosphamide for graft-versus-host disease prophylaxis in HLA matched sibling or matched unrelated donor transplant for patients with acute leukemia, on behalf of ALWP-EBMT. J Hematol Oncol. 2018;11:40 https://doi.org/10.1186/s13045-018-0586-4
Lorentino F, Labopin M, Ciceri F, Vago L, Fleischhauer K, Afanasyev B, et al. Post-transplantation cyclophosphamide GvHD prophylaxis after hematopoietic stem cell transplantation from 9/10 or 10/10 HLA-matched unrelated donors for acute leukemia. Leukemia. 2021;35:585–94. https://doi.org/10.1038/s41375-020-0863-4
Mielcarek M, Furlong T, O’Donnell PV, Storer BE, McCune JS, Storb R, et al. Posttransplantation cyclophosphamide for prevention of graft-versus-host disease after HLA-matched mobilized blood cell transplantation. Blood. 2016;127:1502–8. https://doi.org/10.1182/blood-2015-10-672071
Sanz J, Galimard JE, Labopin M, Afanasyev B, Angelucci E, Ciceri F, et al. Post-transplant cyclophosphamide after matched sibling, unrelated and haploidentical donor transplants in patients with acute myeloid leukemia: a comparative study of the ALWP EBMT. J Hematol Oncol. 2020;13:46. https://doi.org/10.1186/s13045-020-00882-6
Ruggeri A, Sun Y, Labopin M, Bacigalupo A, Lorentino F, Arcese W, et al. Post-transplant cyclophosphamide versus anti-thymocyte globulin as graft-versus-host disease prophylaxis in haploidentical transplant. Haematologica. 2017;102:401–10. https://doi.org/10.3324/haematol.2016.151779
Cieri N, Greco R, Crucitti L, Morelli M, Giglio F, Levati G, et al. Post-transplantation Cyclophosphamide and Sirolimus after Haploidentical Hematopoietic Stem Cell Transplantation Using a Treosulfan-based Myeloablative Conditioning and Peripheral Blood Stem Cells. Biol Blood Marrow Transpl. 2015;21:1506–14. https://doi.org/10.1016/j.bbmt.2015.04.025
Bejanyan N, Pidala JA, Wang X, Thapa R, Nishihori T, Elmariah H, et al. A phase 2 trial of GVHD prophylaxis with PTCy, sirolimus, and MMF after peripheral blood haploidentical transplantation. Blood Adv. 2021;5:1154–63. https://doi.org/10.1182/bloodadvances.2020003779
Solomon SR, Sanacore M, Zhang X, Brown S, Holland K, Morris LE, et al. Calcineurin inhibitor–free graft-versus-host disease prophylaxis with post-transplantation cyclophosphamide and brief-course sirolimus following reduced-intensity peripheral blood stem cell transplantation. Biol Blood Marrow Transpl. 2014;20:1828–34. https://doi.org/10.1016/j.bbmt.2014.07.020
Hernani R, Piñana JL, Pérez A, Quintero A, Montoro J, Hernández-Boluda JC, et al. Sirolimus versus cyclosporine in haploidentical stem cell transplantation with posttransplant cyclophosphamide and mycophenolate mofetil as graft-versus-host disease prophylaxis. EJHaem. 2021;2:236–48. https://doi.org/10.1002/jha2.183
Greco R, Lorentino F, Morelli M, Giglio F, Mannina D, Assanelli A, et al. Posttransplantation cyclophosphamide and sirolimus for prevention of GVHD after HLA-matched PBSC transplantation. Blood. 2016;128:1528–31. https://doi.org/10.1182/blood-2016-06-723205
Morales JM, Wramner L, Kreis H, Durand D, Campistol JM, Andres A, et al. Sirolimus does not exhibit nephrotoxicity compared to cyclosporine in renal transplant recipients. Am J Transpl. 2002;2:436–42. https://doi.org/10.1034/j.1600-6143.2002.20507.x
Zeiser R, Nguyen VH, Beilhack A, Buess M, Schulz S, Baker J, et al. Inhibition of CD4+CD25+ regulatory T-cell function by calcineurin-dependent interleukin-2 production. Blood. 2006;108:390–9. https://doi.org/10.1182/blood-2006-01-0329
Peccatori J, Forcina A, Clerici D, Crocchiolo R, Vago L, Stanghellini MTL, et al. Sirolimus-based graft-versus-host disease prophylaxis promotes the in vivo expansion of regulatory T cells and permits peripheral blood stem cell transplantation from haploidentical donors. Leukemia. 2015;29:396–405. https://doi.org/10.1038/leu.2014.180
Montoro J, Piñana JL, Hernández-Boluda JC, Hernani R, Lorenzo I, Pérez A, et al. Uniform graft-versus-host disease prophylaxis with posttransplant cyclophosphamide, sirolimus, and mycophenolate mofetil following hematopoietic stem cell transplantation from haploidentical, matched sibling and unrelated donors. Bone Marrow Transpl. 2020;55:2147–59. https://doi.org/10.1038/s41409-020-0921-6
Greco R, Lorentino F, Albanese S, Lupo Stanghellini MT, Giglio F, Piemontese S, et al. Posttransplantation cyclophosphamide- and sirolimus-based graft-versus-host-disease prophylaxis in allogeneic stem cell transplant. Transpl Cell Ther. 2021;27:776.e1–776.e13. https://doi.org/10.1016/j.jtct.2021.05.023
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transpl. 2020;55:1114–25. https://doi.org/10.1038/s41409-020-0803-y
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33. https://doi.org/10.1016/j.bbmt.2009.07.004
Mussetti A, De Philippis C, Carniti C, Bastos-Oreiro M, Gayoso J, Cieri N, et al. CD3+ graft cell count influence on chronic GVHD in haploidentical allogeneic transplantation using post-transplant cyclophosphamide. Bone Marrow Transpl. 2018;53:1522–31. https://doi.org/10.1038/s41409-018-0183-8
Xue E, Lorentino F, Clerici D, Farina F, Oltolini C, Giglio F, et al. Coadministration of letermovir and sirolimus in allogeneic hematopoietic cell transplant recipients. Bone Marrow Transpl. 2022;57:128–30. https://doi.org/10.1038/s41409-021-01486-5
Armand P, Gibson CJ, Cutler C, Ho VT, Koreth J, Alyea EP, et al. A disease risk index for patients undergoing allogeneic stem cell transplantation. Blood. 2012;120:905–13. https://doi.org/10.1182/blood-2012-03-418202
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71. https://doi.org/10.1182/blood-2014-01-552984
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47. https://doi.org/10.1182/blood-2016-08-733196
Schuurhuis GJ, Heuser M, Freeman S, Béne MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91. https://doi.org/10.1182/blood-2017-09-801498
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: A new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9. https://doi.org/10.1182/blood-2005-05-2004
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304. https://doi.org/10.1097/00007890-197410000-00001
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. diagnosis and staging working group report. Biol Blood Marrow Transpl. 2005;11:945–56. https://doi.org/10.1016/j.bbmt.2005.09.004
Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017;64:87–91. https://doi.org/10.1093/cid/ciw668
Styczynski J, Van Der Velden W, Fox CP, Engelhard D, De La Camara R, Cordonnier C, et al. Management of epstein-barr virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European conference on infections in leukemia (ECIL-6) guidelines. Haematologica. 2016;101:803–11. https://doi.org/10.3324/haematol.2016.144428
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21. https://doi.org/10.1086/588660
Cesaro S, Dalianis T, Rinaldo CH, Koskenvuo M, Pegoraro A, Einsele H, et al. ECIL guidelines for the prevention, diagnosis and treatment of BK polyomavirus-associated haemorrhagic cystitis in haematopoietic stem cell transplant recipients. J Antimicrob Chemother. 2018;73:12–21. https://doi.org/10.1093/jac/dkx324
Mohty M, Malard F, Abecassis M, Aerts E, Alaskar AS, Aljurf M, et al. Revised diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a new classification from the european society for blood and marrow transplantation. Bone Marrow Transpl. 2016;51:906–12. https://doi.org/10.1038/bmt.2016.130
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457 https://doi.org/10.2307/2281868
Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep. 1966;50:163–70.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. https://doi.org/10.1080/01621459.1999.10474144
Beelen DW, Trenschel R, Stelljes M, Groth C, Masszi T, Reményi P, et al. Treosulfan or busulfan plus fludarabine as conditioning treatment before allogeneic haemopoietic stem cell transplantation for older patients with acute myeloid leukaemia or myelodysplastic syndrome (MC-FludT.14/L): a randomised, non-inferiority, phase 3 trial. Lancet Haematol. 2020;7:e28–e39. https://doi.org/10.1016/S2352-3026(19)30157-7
Battipaglia G, Labopin M, Hamladji RM, Blaise D, Chevallier P, Brissot E, et al. Post-transplantation cyclophosphamide versus antithymocyte globulin in patients with acute myeloid leukemia undergoing allogeneic stem cell transplantation from HLA-identical sibling donors: A retrospective analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Cancer. 2021;127:209–18. https://doi.org/10.1002/cncr.33255
Rambaldi A, Grassi A, Masciulli A, Boschini C, Micò MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: An open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16:1525–36. https://doi.org/10.1016/S1470-2045(15)00200-4
Brissot E, Labopin M, Moiseev I, Cornelissen JJ, Meijer E, Van Gorkom G, et al. Post-transplant cyclophosphamide versus antithymocyte globulin in patients with acute myeloid leukemia in first complete remission undergoing allogeneic stem cell transplantation from 10/10 HLA-matched unrelated donors. J Hematol Oncol. 2020;13:87. https://doi.org/10.1186/S13045-020-00923-0
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96:2062–8. https://doi.org/10.1182/blood.V96.6.2062
Scott BL, Pasquini MC, Fei M, Fraser R, Wu J, Devine SM, et al. Myeloablative versus reduced-intensity conditioning for hematopoietic cell transplantation in acute myelogenous leukemia and myelodysplastic syndromes—long-term follow-up of the BMT CTN 0901 clinical trial. Transpl Cell Ther. 2021;27:483.e1–483.e6. https://doi.org/10.1016/J.JTCT.2021.02.031
Ciurea SO, Zhang MJ, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126:1033–40. https://doi.org/10.1182/BLOOD-2015-04-639831
Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK, et al. Haploidentical transplantation using T cell replete peripheral blood stem cells and myeloablative conditioning in patients with high-risk hematologic malignancies who lack conventional donors is well tolerated and produces excellent relapse-free survival: results of a prospective phase II trial. Biol Blood Marrow Transpl. 2012;18:1859–66. https://doi.org/10.1016/J.BBMT.2012.06.019
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6. https://doi.org/10.1200/JCO.2012.44.3523
Sugita J, Kawashima N, Fujisaki T, Kakihana K, Ota S, Matsuo K, et al. HLA-haploidentical peripheral blood stem cell transplantation with post-transplant cyclophosphamide after busulfan-containing reduced-intensity conditioning. Biol Blood Marrow Transpl. 2015;21:1646–52. https://doi.org/10.1016/j.bbmt.2015.06.008
Gooptu M, Romee R, St. Martin A, Arora M, Al Malki M, Antin JH, et al. HLA-haploidentical vs matched unrelated donor transplants with posttransplant cyclophosphamide-based prophylaxis. Blood. 2021;138:273–82. https://doi.org/10.1182/blood.2021011281
Hickey CL, Kim HT, Nikiforow S, Gooptu M, Koreth J, Ritz J, et al. Graft failure after haploidentical hematopoietic stem cell transplantation. Blood. 2019;134:4486–4486. https://doi.org/10.1182/blood-2019-121659
Lv WR, Zhou Y, Xu J, Fan ZP, Huang F, Xu N, et al. Haploidentical donor transplant is associated with secondary poor graft function after allogeneic stem cell transplantation: A single-center retrospective study. Cancer Med. 2021;10:8497–506. https://doi.org/10.1002/cam4.4353
Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, et al. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transpl. 2013;48:537–43. https://doi.org/10.1038/bmt.2012.239
Luznik L, Pasquini MC, Logan B, Soiffer RJ, Wu J, Devine SM, et al. Randomized phase III BMT CTN trial of calcineurin inhibitor-free chronic graft-versus-host disease interventions in myeloablative hematopoietic cell transplantation for hematologic malignancies. J Clin Oncol. 2022;40:356–68. https://doi.org/10.1200/JCO.21.02293
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103:1317–28. https://doi.org/10.3324/haematol.2018.189258
Yu S, Huang F, Wang Y, Xu Y, Yang T, Fan Z, et al. Haploidentical transplantation might have superior graft-versus-leukemia effect than HLA-matched sibling transplantation for high-risk acute myeloid leukemia in first complete remission: a prospective multicentre cohort study. Leukemia. 2019;34:1433–43. https://doi.org/10.1038/s41375-019-0686-3
Chang YJ, Wang Y, Liu YR, Xu LP, Zhang X-H, Chen H, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol. 2017;10:134. https://doi.org/10.1186/S13045-017-0502-3
Yu J, Du Y, Ahmad S, Patel RD, Varela JC, Chang CC, et al. Comparison of myeloablative versus reduced-intensity conditioning regimens in allogeneic stem cell transplantation recipients with acute myelogenous leukemia with measurable residual disease-negative disease at the time of transplantation: a retrospective cohort study. Transpl Cell Ther. 2021;27:663.e1–663.e6. https://doi.org/10.1016/j.jtct.2021.04.017
Ringdén O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N, et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol. 2009;27:4570–7. https://doi.org/10.1200/JCO.2008.20.9692
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. J Clin Oncol. 2017;35:1154–61. https://doi.org/10.1200/JCO.2016.70.7091
Bornhäuser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13:1035–44. https://doi.org/10.1016/S1470-2045(12)70349-2
Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Posttransplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Invest. 2019;129:2357–73. https://doi.org/10.1172/JCI124218
Récher C, Beyne-Rauzy O, Demur C, Chicanne G, Dos Santos C, Mas VMD, et al. Antileukemic activity of rapamycin in acute myeloid leukemia. Blood. 2005;105:2527–34. https://doi.org/10.1182/blood-2004-06-2494
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of allogeneic transplantation for acute myeloid leukemia with genomic evidence of residual disease. J Clin Oncol. 2020;38:1273–83. https://doi.org/10.1200/JCO.19.03011
Morsink LM, Sandmaier BM, Othus M, Palmieri R, Granot N, Bezerra ED, et al. Conditioning intensity, pre-transplant flow cytometric measurable residual disease, and outcome in adults with acute myeloid leukemia undergoing allogeneic hematopoietic cell transplantation. Cancers. 2020;12:1–18. https://doi.org/10.3390/cancers12092339
Acknowledgements
We would like to thank the hematology teams of IRCCS Ospedale San Raffaele, Hospital Universitari i Politècnic La Fe, and Hospital Clínico Universitario for their help in the care of these patients.
Author information
Authors and Affiliations
Contributions
All authors contributed to patient clinical care and data collection. LL, ABR, JS, MAS, CS, JP, and FC designed the study. LL and ABR updated and interpreted the dataset, performed statistical analysis, and prepared the figures and tables. LL, ABR, and MAS wrote the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
Ethics approval and consent to participate: each center’s institutional review boards approved treatment protocols according to the Declaration of Helsinki. All patients were treated according to institutional programs upon written informed consent for transplant procedures and use of medical records for research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lazzari, L., Balaguer-Roselló, A., Montoro, J. et al. Post-transplant cyclophosphamide and sirolimus based graft-versus-host disease prophylaxis after allogeneic stem cell transplantation for acute myeloid leukemia. Bone Marrow Transplant 57, 1389–1398 (2022). https://doi.org/10.1038/s41409-022-01725-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01725-3
This article is cited by
-
Posttransplant cyclophosphamide beyond haploidentical transplantation
Annals of Hematology (2024)
-
Impact of post-transplant cyclophosphamide (PTCy)-based prophylaxis in matched sibling donor allogeneic haematopoietic cell transplantation for patients with myelodysplastic syndrome: a retrospective study on behalf of the Chronic Malignancies Working Party of the EBMT
Bone Marrow Transplantation (2024)