Abstract
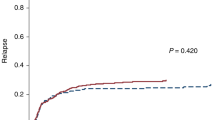
Reduced intensity conditionings (RIC) before after allogeneic hematopoietic stem cell transplantation (HSCT) allow older or unfit patients of being transplanted, but survival expectancy and burden of late complications are poorly described in this setting. All patients (N = 456) who were alive and relapse-free 2 years after HSCT following RIC were included. Cumulative incidences (CI), standardized incidence, or mortality, ratio (SIR or SMR), and competing risk models were used. The 10-year CIs of relapse and non-relapse mortality incidences were 13.9 and 13.4%, respectively. Seventy-eight patients died, late relapse being the most frequent cause of death leading to a SMR of 6.38 (95% CI, 5.1–8.0; p < 0.001). Among non-relapsing patients (n = 412), 30 died (SMR 4.38; 95% CI, 3.3–5.8: p < 0.001). A total of 37 patients developed 41 SM leading to a 10-year cumulative incidence of 12.9%, and a significant SIR relative to the general population (1.4). Finally, we found high CI of cardiovascular (CVC) and venous thromboembolic complications (VTE) (10-year CI; 15.1% and 11.7%, respectively). Older age was the only significant risk factor for CVC and VTE in multivariable analysis. In conclusion, with life expectancy rate of 70%, late survivors after RIC warrants long-term follow-up and active intervention on averting cardiovascular disease and screening cancers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data collected and analyzed in this article came from patient’s chart and from the PROMISE data base. If any reasonable inquiry occurs, please direct the request to the last author at: gerard.socie@aphp.fr.
References
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N. Engl J Med. 2010;363:2091–101.
Giralt S, Estey E, Albitar M, van Besien K, Rondón G, Anderlini P, et al. Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy. Blood 1997;89:4531–6.
McSweeney PA, Niederwieser D, Shizuru JA, Sandmaier BM, Molina AJ, Maloney DG, et al. Hematopoietic cell transplantation in older patients with hematologic malignancies: replacing high-dose cytotoxic therapy with graft-versus-tumor effects. Blood 2001;97:3390–400.
Giralt S, Thall PF, Khouri I, Wang X, Braunschweig I, Ippolitti C, et al. Melphalan and purine analog-containing preparative regimens: reduced-intensity conditioning for patients with hematologic malignancies undergoing allogeneic progenitor cell transplantation. Blood 2001;97:631–7.
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood 1998;91:756–63.
Khouri IF, Keating M, Körbling M, Przepiorka D, Anderlini P, O’Brien S, et al. Transplant-lite: induction of graft-versus-malignancy using fludarabine-based nonablative chemotherapy and allogeneic blood progenitor-cell transplantation as treatment for lymphoid malignancies. J Clin Oncol août. 1998;16:2817–24.
Little MT, Storb R. The future of allogeneic hematopoietic stem cell transplantation: minimizing pain, maximizing gain. J Clin Invest. 2000;105:1679–81.
D’Souza A, Fretham C, Lee SJ, Arora M, Brunner J, Chhabra S, et al. Current use of and trends in hematopoietic cell transplantation in the United States. Biol Blood Marrow Transplant août. 2020;26:e177–82.
Niederwieser D, Baldomero H, Szer J, Gratwohl M, Aljurf M, Atsuta Y, et al. Hematopoietic stem cell transplantation activity worldwide in 2012 and a SWOT analysis of the Worldwide Network for Blood and Marrow Transplantation Group including the global survey. Bone Marrow Transplant. 2016;51:778–85.
Passweg JR, Baldomero H, Chabannon C, Basak GW, Cámara R, Corbacioglu S, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years. Bone Marrow Transplant. 2021;56:1651–64.
Del Galy AS, Marouf A, Raffoux E, Robin M, Michonneau D, Sébert M, et al. Allogeneic hematopoietic stem cell transplantation in elderly patients with acute myeloid leukemia or myelodysplastic syndromes: myth and reality. Leukemia 2021;35:225–8.
Socié G, Stone JV, Wingard JR, Weisdorf D, Henslee-Downey PJ, Bredeson C, et al. Long-term survival and late deaths after allogeneic bone marrow transplantation. Late Effects Working Committee of the International Bone Marrow Transplant Registry. N. Engl J Med. 1999;341:14–21.
Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29:2230–9.
Deeg HJ, Socie G. Malignancies after hematopoietic stem cell transplantation: many questions, some answers. Blood. 1998;91:1833–44.
Tichelli A, Socié G. Considerations for adult cancer survivors. Hematology Am Soc Hematol Educ Program. 2005;516–22.
Socié G, Salooja N, Cohen A, Rovelli A, Carreras E, Locasciulli A, et al. Nonmalignant late effects after allogeneic stem cell transplantation. Blood. 2003;101:3373–85.
Bhatia S, Dai C, Landier W, Hageman L, Wu J, Schlichting E, et al. Trends in late mortality and life expectancy after allogeneic blood or marrow transplantation over 4 decades: a blood or marrow transplant survivor study report. JAMA Oncol. 2021;7:1626–34.
Martin PJ, Counts GW, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. 2010;28:1011–6.
Wong FL, Teh JB, Atencio L, Stiller T, Kim H, Chanson D, et al. Conditional survival, cause-specific mortality, and risk factors of late mortality after allogeneic hematopoietic cell transplantation. J Natl Cancer Inst. 2020;112:1153–61.
Shimoni A, Shem-Tov N, Chetrit A, Volchek Y, Tallis E, Avigdor A, et al. Secondary malignancies after allogeneic stem-cell transplantation in the era of reduced-intensity conditioning; the incidence is not reduced. Leukemia 2013;27:829–35.
Ringdén O, Brazauskas R, Wang Z, Ahmed I, Atsuta Y, Buchbinder D, et al. Second solid cancers after allogeneic hematopoietic cell transplantation using reduced-intensity conditioning. Biol Blood Marrow Transplant 2014;20:1777–84.
Zamora-Ortiz G, Velázquez-Sánchez-de-Cima S, Ponce-de-León S, Gutiérrez-Aguirre CH, Ruiz-Delgado GJ, Gomez-Almaguer D, et al. Secondary malignancies after allogeneic hematopoietic stem cell transplantation using reduced-intensity conditioning and outpatient conduction. Hematology 2014;19:435–40.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant 2009;15:1628–33.
Ades L, Mary J-Y, Robin M, Ferry C, Porcher R, Esperou H, et al. Long-term outcome after bone marrow transplantation for severe aplastic anemia. Blood 2004;103:2490–7.
University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Human Mortality Database. Disponible sur: www.mortality.org or www.humanmortality.de
Perme MP, Manevski D. relsurv: Relative Survival. 2021. Disponible sur: https://CRAN.R-project.org/package=relsurv
Varet J-PJ and H. survexp.fr: Relative survival, AER and SMR based on French death rates. 2013 [cité 14 févr 2022]. Disponible sur: https://CRAN.R-project.org/package=survexp.fr
Gu [aut Z, cre. circlize: Circular Visualization. 2022. Disponible sur: https://CRAN.R-project.org/package=circlize
Duell T, van Lint MT, Ljungman P, Tichelli A, Socié G, Apperley JF, et al. Health and functional status of long-term survivors of bone marrow transplantation. EBMT Working Party on Late Effects and EULEP Study Group on Late Effects. European Group for Blood and Marrow Transplantation. Ann Intern Med. 1997;126:184–92.
Leisenring W, Friedman DL, Flowers MED, Schwartz JL, Deeg HJ. Nonmelanoma skin and mucosal cancers after hematopoietic cell transplantation. J Clin Oncol. 2006;24:1119–26.
Curtis RE, Metayer C, Rizzo JD, Socié G, Sobocinski KA, Flowers MED, et al. Impact of chronic GVHD therapy on the development of squamous-cell cancers after hematopoietic stem-cell transplantation: an international case-control study. Blood 2005;105:3802–11.
Rizzo JD, Curtis RE, Socié G, Sobocinski KA, Gilbert E, Landgren O, et al. Solid cancers after allogeneic hematopoietic cell transplantation. Blood 2009;113:1175–83.
Clavert A, Peric Z, Brissot E, Malard F, Guillaume T, Delaunay J, et al. Late complications and quality of life after reduced-intensity conditioning allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2017;23:140–6.
Friedman DL, Rovo A, Leisenring W, Locasciulli A, Flowers MED, Tichelli A, et al. Increased risk of breast cancer among survivors of allogeneic hematopoietic cell transplantation: a report from the FHCRC and the EBMT-Late Effect Working Party. Blood 2008;111:939–44.
McDonald AM, Chen Y, Wu J, Hageman L, Francisco L, Kung M, et al. Total body irradiation and risk of breast cancer after blood or marrow transplantation: a blood or marrow transplantation survivor study report. J Clin Oncol. 2020;38:2872–82.
Armenian SH, Sun C-L, Francisco L, Steinberger J, Kurian S, Wong FL, et al. Late congestive heart failure after hematopoietic cell transplantation. J Clin Oncol. 2008;26:5537–43.
Chow EJ, Mueller BA, Baker KS, Cushing-Haugen KL, Flowers MED, Martin PJ, et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med 2011;155:21–32.
Chang EK, Chanson D, Teh JB, Iukuridze A, Peng K, Forman SJ, et al. Atrial fibrillation in patients undergoing allogeneic hematopoietic cell transplantation. J Clin Oncol. 2021;39:902–10.
Tichelli A, Bhatia S, Socié G. Cardiac and cardiovascular consequences after haematopoietic stem cell transplantation. Br J Haematol. 2008;142:11–26.
Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. 2013;34:3028–34.
Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37:3232–45.
Andersson C, Vasan RS. Epidemiology of cardiovascular disease in young individuals. Nat Rev Cardiol 2018;15:230–40. avr
Tuppin P, Ricci-Renaud P, Peretti C, Fagot-Campagna A, Alla F, Danchin N, et al. Frequency of cardiovascular diseases and risk factors treated in France according to social deprivation and residence in an overseas territory. Int J Cardiol. 2014;173:430–5.
Delluc A, Tromeur C, Le Ven F, Gouillou M, Paleiron N, Bressollette L, et al. Current incidence of venous thromboembolism and comparison with 1998: a community-based study in Western France. Thromb Haemost 2016;116:967–74.
Labrador J, Lopez-Anglada L, Perez-Lopez E, Lozano FS, Lopez-Corral L, Sanchez-Guijo FM, et al. Analysis of incidence, risk factors and clinical outcome of thromboembolic and bleeding events in 431 allogeneic hematopoietic stem cell transplantation recipients. Haematologica 2013;98:437–43.
Kekre N, Kim HT, Ho VT, Cutler C, Armand P, Nikiforow S, et al. Venous thromboembolism is associated with graft-versus-host disease and increased non-relapse mortality after allogeneic hematopoietic stem cell transplantation. Haematologica 2017;102:1185–91.
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 2020;395:795–808.
Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Biol Blood Marrow Transpl. 2012;18:348–71.
Hashmi SK, Bredeson C, Duarte RF, Farnia S, Ferrey S, Fitzhugh C, et al. National Institutes of Health Blood and Marrow Transplant Late Effects Initiative: The Healthcare Delivery Working Group Report. Biol Blood Marrow Transplant. 2017;23:717–25.
Author information
Authors and Affiliations
Contributions
ASDG: conducted statistical analyzes the data and wrote the manuscript; AR & AC: collect data; DM, MR, FSDF, AX, CF, LA, ER, CH, MB; recruited and took care of the patients and contributed to writing the report. RPDL; participated in study design, and to data interpretation, and contributed to writing the report: GS; was responsible for designing the study, interpreting results, analyzing data, and writing manuscript. All authors provided feedback and approved the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Del Galy, A.S., Rousseau, A., Capes, A. et al. Life expectancy and burden of late complications after reduced intensity conditioning allogeneic transplantation. Bone Marrow Transplant 57, 1365–1372 (2022). https://doi.org/10.1038/s41409-022-01715-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01715-5
This article is cited by
-
Managing Survivorship after Hematopoietic Cell Transplantation
Current Hematologic Malignancy Reports (2023)