Abstract
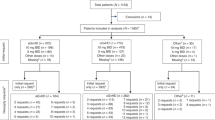
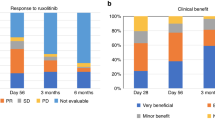
Outside of clinical trials and before commercial availability for acute and chronic graft-versus-host disease (GVHD), the Janus kinase (JAK) 1/JAK2 inhibitor ruxolitinib was available to US patients with steroid-refractory GVHD through an open-label, multicenter expanded access program (EAP) sponsored by Incyte Corporation. To assess the safety of ruxolitinib, data on serious adverse events (SAEs) reported among patients in the EAP were collected. Patients ≥12 years old who received allogeneic hematopoietic cell transplantation for a hematologic malignancy and developed any-grade acute or chronic steroid-refractory GVHD received ruxolitinib at a starting dose of 5 mg twice daily (BID; acute GVHD) or 10 mg BID (chronic GVHD). At data extraction (May 8, 2020), 60 patients with acute GVHD and 549 with chronic GVHD were enrolled. In the acute and chronic GVHD cohorts, 41 (68.3%) and 186 (33.9%) patients, respectively, had ≥1 SAE. Sepsis (8.3%) and respiratory failure (6.7%) were the most common SAEs in the acute GVHD cohort, and pneumonia (4.9%), sepsis (3.8%), and lung infection (3.5%) in chronic GVHD. Infection SAEs were reported in 23.3% and 20.0% of patients with acute and chronic GVHD, respectively. Overall, these safety findings demonstrate the tolerability of ruxolitinib in steroid-refractory GVHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Incyte Corporation (Wilmington, DE, USA) is committed to data sharing that advances science and medicine while protecting patient privacy. Qualified external scientific researchers may request anonymized datasets owned by Incyte for the purpose of conducting legitimate scientific research. Researchers may request anonymized datasets from any interventional study (except Phase 1 studies) for which the product and indication have been approved on or after 1—January 2020 in at least one major market (e.g., US, EU, JPN). Data will be available for request after the primary publication or 2 years after the study has ended. Information on Incyte’s clinical trial data-sharing policy and instructions for submitting clinical trial data requests are available at: https://www.incyte.com/Portals/0/Assets/Compliance%20and%20Transparency/clinical-trial-data-sharing.pdf?ver=2020-05-21-132838-960.
References
Phelan R, Arora M, Chen M. Current use and outcome of hematopoietic stem cell transplantation: CIBMTR US summary slides, 2020. https://www.cibmtr.org/ReferenceCenter/SlidesReports/SummarySlides/pages/index.aspx. Accessed 2 July 2021.
Passweg JR, Baldomero H, Basak GW, Chabannon C, Corbacioglu S, Duarte R, et al. The EBMT activity survey report 2017: a focus on allogeneic HCT for nonmalignant indications and on the use of non-HCT cell therapies. Bone Marrow Transplant. 2019;54:1575–85.
Duarte RF, Labopin M, Bader P, Basak GW, Bonini C, Chabannon C, et al. Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019;54:1525–52.
Zeiser R, Blazar BR. Acute graft-versus-host disease—biologic process, prevention, and therapy. N Engl J Med. 2017;377:2167–79.
Zeiser R, Blazar BR. Pathophysiology of chronic graft-versus-host disease and therapeutic targets. N Engl J Med. 2017;377:2565–79.
Lee SJ, Kim HT, Ho VT, Cutler C, Alyea EP, Soiffer RJ, et al. Quality of life associated with acute and chronic graft-versus-host disease. Bone Marrow Transplant. 2006;38:305–10.
Fiuza-Luces C, Simpson RJ, Ramirez M, Lucia A, Berger NA. Physical function and quality of life in patients with chronic GvHD: a summary of preclinical and clinical studies and a call for exercise intervention trials in patients. Bone Marrow Transplant. 2016;51:13–26.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8.
Atsuta Y, Hirakawa A, Nakasone H, Kurosawa S, Oshima K, Sakai R, et al. Late mortality and causes of death among long-term survivors after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22:1702–9.
Axt L, Naumann A, Toennies J, Haen SP, Vogel W, Schneidawind D, et al. Retrospective single center analysis of outcome, risk factors and therapy in steroid refractory graft-versus-host disease after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2019;54:1805–14.
Al Malki MM, Gendzekhadze K, Yang D, Mokhtari S, Parker P, Karanes C, et al. Long-term outcome of allogeneic hematopoietic stem cell transplantation from unrelated donor using tacrolimus/sirolimus-based GVHD prophylaxis: impact of HLA mismatch. Transplantation. 2020;104:1070–80.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS, et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood. 2012;119:296–307.
Arai S, Arora M, Wang T, Spellman SR, He W, Couriel DR, et al. Increasing incidence of chronic graft-versus-host disease in allogeneic transplantation: a report from the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2015;21:266–74.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389–401.e1.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Hematopoietic cell transplantation (HCT): pre-transplant recipient evaluation and management of graft-versus-host disease (Version 2.2021). https://www.nccn.org/professionals/physician_gls/pdf/hct.pdf. Accessed 9 June 2021.
Penack O, Marchetti M, Ruutu T, Aljurf M, Bacigalupo A, Bonifazi F, et al. Prophylaxis and management of graft versus host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2020;7:e157–67.
Major-Monfried H, Renteria AS, Pawarode A, Reddy P, Ayuk F, Holler E, et al. MAGIC biomarkers predict long-term outcomes for steroid-resistant acute GVHD. Blood. 2018;131:2846–55.
Garnett C, Apperley JF, Pavlu J. Treatment and management of graft-versus-host disease: improving response and survival. Ther Adv Hematol. 2013;4:366–78.
Flowers ME, Storer B, Carpenter P, Rezvani AR, Vigorito AC, Campregher PV, et al. Treatment change as a predictor of outcome among patients with classic chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2008;14:1380–4.
Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, et al. Ruxolitinib for glucocorticoid-refractory acute graft-versus-host disease. N Engl J Med. 2020;382:1800–10.
Zeiser R, Polverelli N, Ram R, Hashmi SK, Chakraverty R, Middeke JM, et al. Ruxolitinib for glucocorticoid-refractory chronic graft-versus-host disease. N Engl J Med. 2021;385:228–38.
JAKAFI® (ruxolitinib). Full Prescribing Information. Wilmington, DE, USA: Incyte Corporation; 2021.
MacMillan ML, DeFor TE, Weisdorf DJ. What predicts high risk acute graft-versus-host disease (GVHD) at onset?: Identification of those at highest risk by a novel acute GVHD risk score. Br J Haematol. 2012;157:732–41.
Jagasia M, Perales MA, Schroeder MA, Ali H, Shah NN, Chen YB, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135:1739–49.
Harrison C, Kiladjian J-J, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366:787–98.
Acknowledgements
Support for this study was provided by Incyte Corporation (Wilmington, DE, USA). Writing assistance was provided by Jane Kovalevich, Ph.D., an employee of ICON (Blue Bell, PA, USA), and was funded by Incyte Corporation.
Author information
Authors and Affiliations
Contributions
MAS contributed to data acquisition, data interpretation, and paper writing. PNH contributed to data acquisition, data interpretation, and paper writing. AB contributed to study conceptualization, data management, and paper writing. DP contributed to study conceptualization, statistical analyses, data interpretation, and paper writing. VB contributed to study conceptualization, data interpretation, and paper writing. JFD contributed to data acquisition, data interpretation, and paper writing. All authors approved the final submitted version of the paper.
Corresponding author
Ethics declarations
Competing interests
MAS has served on advisory boards and received honoraria or consultancy fees unrelated to the present work from CareDx, Incyte Corporation, and Sanofi Genzyme. PNH has received consulting fees from Amgen, BMS, GSK, Incyte Corporation, Janssen, Karyopharm, and Takeda. AB, DP, and VB are employees and shareholders of Incyte Corporation. JFD served on advisory boards for Arch, Bioline, Incyte Corporation, Macrogenics, and Rivervest and is a cofounder of Magenta Therapeutics and WUGEN.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Schroeder, M.A., Hari, P.N., Blithe, A. et al. Safety analysis of patients who received ruxolitinib for steroid-refractory acute or chronic graft-versus-host disease in an expanded access program. Bone Marrow Transplant 57, 975–981 (2022). https://doi.org/10.1038/s41409-022-01673-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01673-y
This article is cited by
-
Ruxolitinib in patients with graft versus host disease (GvHD): findings from a compassionate use program
Bone Marrow Transplantation (2024)
-
Ruxolitinib for GVHD: no unexpected serious AEs in EAP
Reactions Weekly (2022)