Abstract
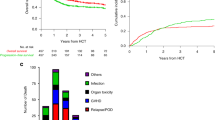
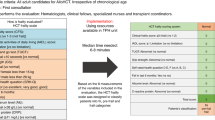
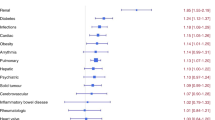
Nowadays, the evaluation of elderly patients' eligibility for allogeneic stem cell transplantation (allo-SCT) is crucial. We evaluated the feasibility and efficacy of a multidimensional geriatric assessment, the Fondazione Italiana Linfomi (FIL) score, on a cohort of 228 patients older than 60 years submitted to allo-SCT in Italy and France from 2008 to 2018. Based on FIL score, available in 215 patients, 125 (58%) patients were classified as “fit” and 90 as “unfit/frail.” The hematopoietic cell transplantation-specific comorbidity index (HCT-CI) was measured in 222 patients (97%); 71 (32%) patients had HCT-CI 0, 75 (34%) patients scored 1–2, and 76 (34%) ≥3. A total of 121 (53%) patients died after a median follow-up of 36 months. FIL score was found to highly predict survival, due to an excess of NRM in unfit/frail group, and confirmed its independent prognostic role on OS (HR: 0.37; 95% CI: 0.25–0.55; p < 0.0001). On the contrary, the HCI-CI failed in allo-SCT outcome prediction (HR: 1.06; 95% CI: 0.96–1.16; p = 0.27). In summary, a comprehensive geriatric assessment with FIL score seems to add significant prognostic information in elderly patients submitted to allo-SCT. The pretransplant adoption of this easy-to-use tool could help the patients’ selection and management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Passweg JR, Baldomero H, Basak GW, Chabannon C, Corbacioglu S, Duarte R, et al. The EBMT activity survey report 2017: a focus on allogeneic HCT for nonmalignant indications and on the use of non-HCT cell therapies. Bone Marrow Transplant. 2019;54:1575–85. https://doi.org/10.1038/s41409-019-0465-9.
Ringden O, Boumendil A, Labopin M, Canaani J, Beelen D, Ehninger G, et al. Outcome of allogeneic hematopoietic stem cell transplantation in patients age >69 years with acute myelogenous leukemia: on behalf of the acute leukemia working party of the european society for blood and marrow transplantation. Biol Blood Marrow Transplant. 2019;25:1975–83. https://doi.org/10.1016/j.bbmt.2019.05.037.
Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky Performance Status. Cancer. 1980;45:2220–4. 10.1002/1097-0142(19800415)45:8<2220::aid-cncr2820450835>3.0.co;2-q.
Sorror M, Storer B, Sandmaier BM, Maloney DG, Chauncey TR, Langston A, et al. Hematopoietic cell transplantation-comorbidity index and Karnofsky Performance Status are independent predictors of morbidity and mortality after allogeneic nonmyeloablative hematopoietic cell transplantation. Cancer. 2008;112:1992–2001. https://doi.org/10.1002/cncr.23375.
Artz AS, Pollyea DA, Kocherginsky M, Stock W, Rich E, Odenike O, et al. Performance status and comorbidity predict transplant-related mortality after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2006;12:954–64. https://doi.org/10.1016/j.bbmt.2006.05.015.
Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. https://doi.org/10.2190/UURL-2RYU-WRYD-EY3K.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86.
Muffly LS, Kocherginsky M, Stock W, Chu Q, Bishop MR, Godley LA, et al. Geriatric assessment to predict survival in older allogeneic hematopoietic cell transplantation recipients. Haematologica. 2014;99:1373–9. https://doi.org/10.3324/haematol.2014.103655.
Artz AS. Biologic vs physiologic age in the transplant candidate. Hematol Am Soc Hematol Educ Program. 2016;2016:99–105. https://doi.org/10.1182/asheducation-2016.1.99.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9. https://doi.org/10.1182/blood-2005-05-2004.
Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–48. https://doi.org/10.1016/0165-1781(92)90005-n.
Muffly LS, Boulukos M, Swanson K, Kocherginsky M, Cerro PD, Schroeder L, et al. Pilot study of comprehensive geriatric assessment (CGA) in allogeneic transplant: CGA captures a high prevalence of vulnerabilities in older transplant recipients. Biol Blood Marrow Transplant. 2013;19:429–34. https://doi.org/10.1016/j.bbmt.2012.11.006.
Liu JJ, Extermann M. Comprehensive geriatric assessment and its clinical impact in oncology. Clin Geriatr Med. 2012;28:19–31. https://doi.org/10.1016/j.cger.2011.10.001.
Abel GA, Klepin HD. Frailty and the management of hematologic malignancies. Blood. 2018;131:515–24. https://doi.org/10.1182/blood-2017-09-746420.
Tucci A, Martelli M, Rigacci L, Riccomagno P, Cabras MG, Salvi F, et al. Comprehensive geriatric assessment is an essential tool to support treatment decisions in elderly patients with diffuse large B-cell lymphoma: a prospective multicenter evaluation in 173 patients by the Lymphoma Italian Foundation (FIL). Leuk Lymphoma. 2015;56:921–6. https://doi.org/10.3109/10428194.2014.953142.
Tucci A, Ferrari S, Bottelli C, Borlenghi E, Drera M, Rossi G. A comprehensive geriatric assessment is more effective than clinical judgment to identify elderly diffuse large cell lymphoma patients who benefit from aggressive therapy. Cancer. 2009;115:4547–53. https://doi.org/10.1002/cncr.24490.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71. https://doi.org/10.1182/blood-2014-01-552984.
Harris AC, Young R, Devine S, Hogan WJ, Ayuk F, Bunworasate U, et al. International, multicenter standardization of acute graft-versus-host disease clinical data collection: a report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transplant. 2016;22:4–10. https://doi.org/10.1016/j.bbmt.2015.09.001.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21:389–401 e381. https://doi.org/10.1016/j.bbmt.2014.12.001.
McGee S. Simplifying likelihood ratios. J Gen Intern Med. 2002;17:646–9. https://doi.org/10.1046/j.1525-1497.2002.10750.x.
Harrell FE Jr, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modelling strategies for improved prognostic prediction. Stat Med. 1984;3:143–52. https://doi.org/10.1002/sim.4780030207.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Muffly L, Pasquini MC, Martens M, Brazauskas R, Zhu X, Adekola K, et al. Increasing use of allogeneic hematopoietic cell transplantation in patients aged 70 years and older in the United States. Blood. 2017;130:1156–64. https://doi.org/10.1182/blood-2017-03-772368.
Passweg JR, Baldomero H, Bader P, Basak GW, Bonini C, Duarte R, et al. Is the use of unrelated donor transplantation leveling off in Europe? The 2016 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transplant. 2018;53:1139–48. https://doi.org/10.1038/s41409-018-0153-1.
Raimondi R, Tosetto A, Oneto R, Cavazzina R, Rodeghiero F, Bacigalupo A, et al. Validation of the hematopoietic cell transplantation-specific comorbidity index: a prospective, multicenter GITMO study. Blood. 2012;120:1327–33. https://doi.org/10.1182/blood-2012-03-414573.
Sorror ML, Logan BR, Zhu X, Rizzo JD, Cooke KR, McCarthy PL, et al. Prospective validation of the predictive power of the hematopoietic cell transplantation comorbidity index: a Center for International Blood and Marrow Transplant Research Study. Biol Blood Marrow Transplant. 2015;21:1479–87. https://doi.org/10.1016/j.bbmt.2015.04.004.
Nakaya A, Mori T, Tanaka M, Tomita N, Nakaseko C, Yano S, et al. Does the hematopoietic cell transplantation specific comorbidity index (HCT-CI) predict transplantation outcomes? A prospective multicenter validation study of the Kanto Study Group for Cell Therapy. Biol Blood Marrow Transplant. 2014;20:1553–9. https://doi.org/10.1016/j.bbmt.2014.06.005.
Mohile SG, Dale W, Somerfield MR, Hurria A. Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO Guideline for Geriatric Oncology Summary. J Oncol Pract. 2018;14:442–6. https://doi.org/10.1200/JOP.18.00180.
Pamukcuoglu M, Bhatia S, Weisdorf DJ, DeFor TE, Ustun C, Nayar M, et al. Hematopoietic cell transplant-related toxicities and mortality in frail recipients. Biol Blood Marrow Transplant. 2019;25:2454–60. https://doi.org/10.1016/j.bbmt.2019.07.030.
Lin RJ, Elko TA, Devlin SM, Shahrokni A, Jakubowski AA, Dahi PB, et al. Impact of geriatric vulnerabilities on allogeneic hematopoietic cell transplantation outcomes in older patients with hematologic malignancies. Bone Marrow Transplant. 2019. https://doi.org/10.1038/s41409-019-0654-6.
Deschler B, Ihorst G, Schnitzler S, Bertz H, Finke J. Geriatric assessment and quality of life in older patients considered for allogeneic hematopoietic cell transplantation: a prospective risk factor and serial assessment analysis. Bone Marrow Transplant. 2018;53:565–75. https://doi.org/10.1038/s41409-017-0021-4.
Turner A, Hochschild A, Burnett J, Zulfiqar A, Dyer CB. High prevalence of medication non-adherence in a sample of community-dwelling older adults with adult protective services-validated self-neglect. Drugs Aging. 2012;29:741–9. https://doi.org/10.1007/s40266-012-0007-2.
Mizokami F, Mase H, Kinoshita T, Kumagai T, Furuta K, Ito K. Adherence to medication regimens is an effective indicator of cognitive dysfunction in elderly individuals. Am J Alzheimers Dis Other Demen. 2016;31:132–6. https://doi.org/10.1177/1533317515598859.
Beaudart C, Zaaria M, Pasleau F, Reginster JY, Bruyere O. Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS ONE. 2017;12:e0169548. https://doi.org/10.1371/journal.pone.0169548.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Polverelli, N., Tura, P., Battipaglia, G. et al. Multidimensional geriatric assessment for elderly hematological patients (≥60 years) submitted to allogeneic stem cell transplantation. A French–Italian 10-year experience on 228 patients. Bone Marrow Transplant 55, 2224–2233 (2020). https://doi.org/10.1038/s41409-020-0934-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0934-1
This article is cited by
-
Transplantation and Cellular Therapy for Older Adults—The MSK Approach
Current Hematologic Malignancy Reports (2024)
-
Impact of hematopoietic cell transplant frailty scale on transplant outcome in adults
Bone Marrow Transplantation (2023)
-
Age is no barrier for adults undergoing HCT for AML in CR1: contemporary CIBMTR analysis
Bone Marrow Transplantation (2022)
-
Feasibility of geriatric assessment before transplant conditioning regimen in older HCT recipients
Bone Marrow Transplantation (2021)
-
Physically “fit” for allogeneic stem cell transplant?
Bone Marrow Transplantation (2021)