Abstract
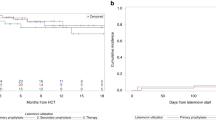
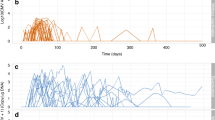
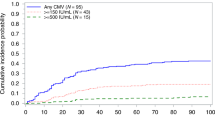
Letermovir (LMV) is licensed for prophylaxis of CMV infection in allogeneic hematopoietic cell transplant adult CMV-seropositive patients. Due to its favorable safety profile, LMV brings potential for use in other clinical situations, outside the approved indication. The objective of the study was to analyze the efficacy and safety of the use of LMV in off-label indications in EBMT centers. A total of 49 patients were reported including 44 adults and 5 children. LMV was administered for: secondary prophylaxis (37 adults, 3 children), primary prophylaxis (2 children), pre-emptive treatment (5 adults), and therapy of CMV disease (2 adults; pneumonia, colitis). Cyclosporine was concomitantly used in 26 patients. Overall, LMV was used for a median 112 days (range: 10–473). Cumulative incidence of breakthrough infections during secondary prophylaxis was 10.1% (95% CI = 3.1–21.9). Prophylactic treatment with LMV resulted in 94.9% (95% CI = 81.0–98.7), and 81.9% (95% CI = 65.7–90.9) probability of, respectively, 60 and 120-day survival without CMV infection in patients receiving secondary prophylaxis. During therapy of CMV infection/disease, probability of 60 and 120-day overall survival was 100% and 71.4% (95% CI = 25.8–92.0), respectively. No breakthrough infection occurred in children on LMV prophylaxis. Adverse events were reported in 15/49 (30.4%) patients: the most common being nausea/vomiting (22.4%). In conclusion, the efficacy of the use of LMV as secondary prophylaxis was high, and the preliminary experience with the use of LMV for the treatment of patients with refractory CMV infection/disease was positive. Our data showed that higher dose or prolonged therapy did not result in increased rate of adverse events.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Green ML, Leisenring W, Xie H, Mast TC, Cui Y, Sandmaier BM, et al. Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol. 2016;3:e119–127. https://doi.org/10.1016/S2352-3026(15)00289-6.
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J, et al. CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood. 2013;122:3359–64. https://doi.org/10.1182/blood-2013-05-499830.
Ljungman P, Brand R, Hoek J, de la Camara R, Cordonnier C, Einsele H, et al. Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis. 2014;59:473–81. https://doi.org/10.1093/cid/ciu364.
Garcia-Vidal C, Upton A, Kirby KA, Marr KA. Epidemiology of invasive mold infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation. Clin Infect Dis. 2008;47:1041–50. https://doi.org/10.1086/591969.
Yong MK, Slavin MA, Kontoyiannis DP. Invasive fungal disease and cytomegalovirus infection: is there an association? Curr Opin Infect Dis. 2018;31:481–9. https://doi.org/10.1097/QCO.0000000000000502.
Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017;64:87–91. https://doi.org/10.1093/cid/ciw668.
Styczynski J. ABC of viral infections in hematology: focus on herpesviruses. Acta Haematol Pol. 2019;50:159–66. https://doi.org/10.2478/ahp-2019-0026.
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF, et al. Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N. Engl J Med. 2017;377:2433–44. https://doi.org/10.1056/NEJMoa1706640.
Styczynski J. Prophylaxis vs preemptive therapy in prevention of CMV infection: new insight on prophylactic strategy after allogeneic hematopoietic cell transplantation. Acta Haematol Pol. 2020;51:17–23. https://doi.org/10.2478/ahp-2020-0005.
Ljungman P, Schmitt M, Marty FM, Maertens J, Chemaly RF, Kartsonis NA, et al. A mortality analysis of letermovir prophylaxis for cytomegalovirus (cmv) in cmv-seropositive recipients of allogeneic hematopoietic-cell transplantation. Clin Infect Dis. 2020;70:1525–33. https://doi.org/10.1093/cid/ciz490.
Marty FM, Ljungman PT, Chemaly RF, Wan H, Teal VL, Butterton JR, et al. Outcomes of patients with detectable CMV DNA at randomization in the phase III trial of letermovir for the prevention of CMV infection in allogeneic hematopoietic cell transplantation. Am J Transpl. 2020;20:1703–11. https://doi.org/10.1111/ajt.15764.
Chong PP, Teiber D, Prokesch BC, Arasaratnam RJ, Peltz M, Drazner MH, et al. Letermovir successfully used for secondary prophylaxis in a heart transplant recipient with ganciclovir-resistant cytomegalovirus syndrome (UL97 mutation). Transpl Infect Dis. 2018;20:e12965. https://doi.org/10.1111/tid.12965.
Jung S, Michel M, Stamminger T, Michel D. Fast breakthrough of resistant cytomegalovirus during secondary letermovir prophylaxis in a hematopoietic stem cell transplant recipient. BMC Infect Dis. 2019;19:388. https://doi.org/10.1186/s12879-019-4016-1.
Lin A, Maloy M, Su Y, Bhatt V, DeRespiris L, Griffin M, et al. Letermovir for primary and secondary cytomegalovirus prevention in allogeneic hematopoietic cell transplant recipients: real-world experience. Transpl Infect Dis. 2019;21:e13187. https://doi.org/10.1111/tid.13187.
Kilgore JT, Becken B, Varga MG, Parikh S, Prasad V, Lugo D, et al. Use of letermovir for salvage therapy for resistant cytomegalovirus in a pediatric hematopoietic stem cell transplant recipient. J Pediatr Infect Dis Soc. 2019. https://doi.org/10.1093/jpids/piz050.
Perez Marin M, Decosterd LA, Andre P, Buclin T, Mercier T, Murray K, et al. Compassionate use of letermovir in a 2-year-old immunocompromised child with resistant cytomegalovirus disease. J Pediatr Infect Dis Soc. 2020;9:96–99. https://doi.org/10.1093/jpids/piz033.
Chemaly RF, Chou S, Einsele H, Griffiths P, Avery R, Razonable RR, et al. Definitions of resistant and refractory cytomegalovirus infection and disease in transplant recipients for use in clinical trials. Clin Infect Dis. 2019;68:1420–6. https://doi.org/10.1093/cid/ciy696.
Nagler A, Shimoni A. Conditioning. In: Carreras E, Dufour C, Mohty M, Kroger N, editors. The EBMT handbook: hematopoietic stem cell transplantation and cellular therapies. Springer Open. Cham (CH); 2019. pp. 99–107.
Robin C, Thiebaut A, Alain S, Sicre de Fontbrune F, Berceanu A, D’Aveni M, et al. Letermovir for secondary prophylaxis of cytomegalovirus infection and disease after allogeneic hematopoietic cell transplantation: results from the french compassionate program. Biol Blood Marrow Transpl. 2020;26:978–84. https://doi.org/10.1016/j.bbmt.2020.01.027.
Styczynski J. Who is the patient at risk of CMV recurrence: a review of the current scientific evidence with a focus on hematopoietic cell transplantation. Infect Dis Ther. 2018;7:1–16. https://doi.org/10.1007/s40121-017-0180-z.
Acknowledgements
Patients were reported from the following centers: Department of Pediatric Hematology and Oncology, Collegium Medicum, Bydgoszcz, Poland (n = 1); Hospital St. Louis, Paris, France (n = 18); Klinik für Innere Medizin/Hämatologie, Universitätsspital Basel, Switzerland (n = 5); Department for Cellular Therapy and Allogeneic Stem Cell Transplantation, Stockholm, Karolinska University Hospital Huddinge, Sweden (n = 2); Division of Pediatric Hematology, Oncology and Stem Cell Transplantation, Helsinki University Hospital, Helsinki, Finland (n = 1); Department of Hematology, Radboud University Center Nijmegen, The Netherlands (n = 1); Hospital U. Marqués de Valdecilla, Santander, Spain (n = 4); Hospital Clínico Universitario-INCLIVA. University of Valencia, Spain (n = 2); Birmingham Heartlands Hospital, Birmingham, UK (n = 1); Division of Pediatric Hematology, Oncology and Stem Cell Transplantation, University of Padova, Padova, Italy (n = 2); Infectious Disease Research Program, Center for Bone Marrow Transplantation and Department of Pediatric Hematology and Oncology, University Children’s Hospital Muenster, Germany (n = 2); Universitaet Rostock, Rostock, Germany (n = 1); Attikon University General Hospital, Athens, Greece (n = 2); Techniciens d’Etude Clinique suivi de patients greffes, Strasbourg, France (n = 1); Charles University Hospital, Pilsen, Czech Republic (n = 1); University Regensburg, Regensburg, Germany (n = 4); IRRCS Ospedale Pediatrico Bambino Gesù, Sapienza, University of Rome, Rome, Italy (n = 1); Onco-Ematologia Pediatrica, Torino, Italy (n = 1).
Author information
Authors and Affiliations
Contributions
Concept of the study: PL. Design of the study: PL, JS, MM, and RdlC. Analysis of data: all authors. Data check-up and coordination: NK and LW. Statistical analysis and figures: GT. Manuscript writing: JS, LG, and PL. Critical revision: all authors. Final approval: all authors.
Corresponding author
Ethics declarations
Conflict of interest
JS, LG, PL—Lecture fees from MSD. PL—advisory board participation MSD. Other authors have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Styczyński, J., Tridello, G., Xhaard, A. et al. Use of letermovir in off-label indications: Infectious Diseases Working Party of European Society of Blood and Marrow Transplantation retrospective study. Bone Marrow Transplant 56, 1171–1179 (2021). https://doi.org/10.1038/s41409-020-01166-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01166-w
This article is cited by
-
Letermovir for Cytomegalovirus infection in pediatric patients undergoing allogenic hematopoietic stem cell transplantation: a real-life study by the Infectious Diseases Working Group of Italian Association of Pediatric Hematology-Oncology (AIEOP)
Bone Marrow Transplantation (2024)
-
Letermovir for CMV Prophylaxis in Very High-Risk Pediatric Hematopoietic Stem Cell Transplantation Recipients for Inborn Errors of Immunity
Journal of Clinical Immunology (2024)
-
Letermovir for Prophylaxis and Pre-emptive Therapy of Cytomegalovirus Infection in Paediatric Allogeneic Haematopoietic Cell Transplant Patients
Pediatric Drugs (2023)
-
Acute kidney injury within 100 days post allogeneic hematopoietic cell transplantation is associated with increased risk of post-transplant complications and poor transplant outcomes
Bone Marrow Transplantation (2022)
-
Risk factors for late cytomegalovirus infection after completing letermovir prophylaxis
International Journal of Hematology (2022)