Abstract
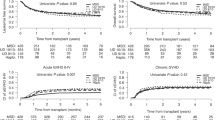
We compared transplant outcomes of 708 acute myeloid leukemia (AML) patients receiving haploidentical allogeneic hematopoietic-cell transplantation using thiotepa/busulfan/fludarabine (TBF) conditioning with posttransplant cyclophosphamide (ptCy), to 2083 patients receiving matched unrelated donor (MUD) transplantation using fludarabine/busulfan (FB) conditioning and in vivo T-cell depletion. For intermediate cytogenetic risk AML transplanted in first complete remission (CR1), multivariate analysis revealed that haplo-TBF significantly increased nonrelapse mortality (NRM) (HR 2.1; p = 0.0006) but did not affect relapse incidence (RI), leukemia-free survival (LFS), overall survival (OS), or graft-versus-host disease-free, relapse-free survival (GRFS). For high cytogenetic risk AML transplanted in CR1, haplo-TBF significantly increased NRM (HR = 2.7; p = 0.02), decreased RI (HR = 0.45; p = 0.03) but had no influence on LFS, OS, or GRFS. For AML transplanted in CR2, haplo-TBF significantly increased NRM (HR = 2.36; p = 0.008), decreased RI (HR = 0.38; p = 0.005), but had no influence on LFS, OS, or GRFS. Finally, for AML patients transplanted with active disease, haplo-TBF had no influence on transplant outcomes. In conclusion, compared to MUD-FB, haplo-TBF increased NRM, reduced RI in high-risk AML in CR, resulting in similar LFS, OS, and GRFS. These results comparing two different approaches support the use of a haploidentical family donor for high-risk AML patients lacking a matched sibling donor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Gupta V, Tallman MS, He W, Logan BR, Copelan E, Gale RP, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010;116:1839–48.
Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the US registry. N Engl J Med. 2014;371:339–48.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50. https://doi.org/10.1016/j.bbmt.2008.03.005.
Luznik L, Bolaños-Meade J, Zahurak M, Chen AR, Smith BD, Brodsky R, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115:3224–30.
Kanakry CG, Fuchs EJ, Luznik L. Modern approaches to HLA-haploidentical blood or marrow transplantation. Nat Rev Clin Oncol. 2016;13:10.
Kanakry JA, Luznik L. Might haplo “be the (better) match”? Blood. 2016;127:799–800.
Ciurea SO, Zhang M-J, Bacigalupo AA, Bashey A, Appelbaum FR, Aljitawi OS, et al. Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood. 2015;126:1033–40.
Lorentino F, Labopin M, Bernardi M, Ciceri F, Socié G, Cornelissen JJ, et al. Comparable outcomes of haploidentical, 10/10 and 9/10 unrelated donor transplantation in adverse karyotype AML in first complete remission. Am J Hematol. 2018;93:1236–44.
Pagliardini T, Harbi S, Fürst S, Castagna L, Legrand F, Faucher C, et al. Post-transplantation cyclophosphamide-based haploidentical versus Atg-based unrelated donor allogeneic stem cell transplantation for patients younger than 60 years with hematological malignancies: a single-center experience of 209 patients. Bone Marrow Transplant. 2019;54:1067–76.
Bazarbachi A, Boumendil A, Finel H, Castagna L, Dominietto A, Blaise D, et al. Influence of donor type, stem cell source and conditioning on outcomes after haploidentical transplant for lymphoma–a LWP‐EBMT study. Br J Haematol. 2019;188:745–56.
Gu B, Zhang X, Chen G, Wu X, Ma X, Chen S, et al. Efficacy of haploidentical hematopoietic stem cell transplantation compared to HLA-matched transplantation for primary refractory acute myeloid leukemia. Ann Hematol. 2018;97:2185–94.
Gagelmann N, Bacigalupo A, Rambaldi A, Hoelzer D, Halter J, Sanz J, et al. Haploidentical stem cell transplantation with posttransplant cyclophosphamide therapy vs other donor transplantations in adults with hematologic cancers: a systematic review and meta-analysis. JAMA Oncol. 2019;5:1739–48.
Arcuri LJ, Aguiar MTM, Ribeiro AAF, Pacheco AGF. Haploidentical transplantation with post-transplant cyclophosphamide versus unrelated donor hematopoietic stem cell transplantation: a systematic review and meta-analysis. Biol Blood Marrow Transplant. 2019;25:2422–30.
Yang B, Yu R, Cai L, Guo B, Chen H, Zhang H, et al. Haploidentical versus matched donor stem cell transplantation for patients with hematological malignancies: a systemic review and meta-analysis. Bone Marrow Transplant. 2019;54:99–122.
Passweg J, Baldomero H, Bader P, Bonini C, Duarte R, Dufour C, et al. Use of haploidentical stem cell transplantation continues to increase: the 2015 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transplant. 2017;52:811–7.
Perales M-A, Tomlinson B, Zhang M-J, Martin AS, Beitinjaneh A, Gibson J, et al. Alternative donor transplantation for acute myeloid leukemia in patients aged ≥50 years: young HLA-matched unrelated or haploidentical donor? Haematologica. 2020;105:407–13.
Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, et al. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical versus matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103:1317–28.
Solomon SR, St. Martin A, Shah NN, Fatobene G, Al Malki MM, Ballen KK, et al. Myeloablative vs reduced intensity T-cell–replete haploidentical transplantation for hematologic malignancy. Blood Adv. 2019;3:2836–44.
Kasamon YL, Bolaños-Meade J, Prince GT, Tsai H-L, McCurdy SR, Kanakry JA, et al. Outcomes of nonmyeloablative HLA-haploidentical blood or marrow transplantation with high-dose post-transplantation cyclophosphamide in older adults. J Clin Oncol. 2015;33:3152.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant. 2013;19:117–22.
Bacigalupo A, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and post-transplant cyclophosphamide for hematologic malignanices following a myeloablative conditioning: an update. Bone Marrow Transplant. 2015;50:S37–9.
Pagliardini T, Castagna L, Harbi S, Della Porta M, Rey J, Fürst S, et al. Thiotepa, fludarabine, and busulfan conditioning regimen before T cell-replete haploidentical transplantation with post-transplant cyclophosphamide for acute myeloid leukemia: a bicentric experience of 100 patients. Biol Blood Marrow Transplant. 2019;25:1803–9.
Duléry R, Bastos J, Paviglianiti A, Malard F, Brissot E, Battipaglia G, et al. Thiotepa, busulfan, and fludarabine conditioning regimen in T cell-replete HLA-haploidentical hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2019;25:1407–15.
Rambaldi A, Grassi A, Masciulli A, Boschini C, Micò MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16:1525–36.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304. https://doi.org/10.1097/00007890-197410000-00001.
Terwey TH, Vega-Ruiz A, Hemmati PG, Martus P, Dietz E, le Coutre P, et al. NIH-defined graft-versus-host disease after reduced intensity or myeloablative conditioning in patients with acute myeloid leukemia. Leukemia. 2012;26:536–42. https://doi.org/10.1038/leu.2011.230.
R Core Team. R: a language for statistical computing. 2014. Vienna, Austria: R Foundation for Statistical Computing. 2018.
Salas MQ, Law AD, Lam W, Al-Shaibani Z, Loach D, Michelis FV, et al. Safety and efficacy of haploidentical peripheral blood stem cell transplantation for myeloid malignancies using post-transplantation cyclophosphamide and anti-thymocyte globulin as graft-versus-host disease prophylaxis. Clin Hematol Int. 2019;1:105–13.
Saraceni F, Labopin M, Hamladji R-M, Mufti G, Socié G, Shimoni A, et al. Thiotepa-busulfan-fludarabine compared to busulfan-fludarabine for sibling and unrelated donor transplant in acute myeloid leukemia in first remission. Oncotarget. 2018;9:3379.
El-Cheikh J, Labopin M, Al-Chami F, Bazarbachi A, Angelucci E, Santarone S, et al. Effect of the thiotepa dose in the TBF conditioning regimen in patients undergoing allogeneic stem cell transplantation for acute myeloid leukemia in complete remission: a report From the EBMT Acute Leukemia Working Party. Clin Lymphoma Myeloma Leuk. 2020;20:296–304.
Shimoni A, Labopin M, Finke J, Ciceri F, Deconinck E, Kröger N, et al. Donor selection for a second allogeneic stem cell transplantation in AML patients relapsing after a first transplant: a study of the Acute Leukemia Working Party of EBMT. Blood Cancer J. 2019;9:1–9.
Roy DC, Walker I, Maertens J, Lewalle P, Olavarria E, Selleslag D, et al. ATIR101 administered after T-cell-depleted haploidentical HSCT reduces NRM and improves overall survival in acute leukemia. Leukemia. 2020;34:1–17.
Acknowledgements
AB and MM proposed the study, interpreted the data, and wrote the manuscript. ML helped with the design and was responsible for statistical analysis. All other authors reported updated patient data and read and commented on the manuscript. All authors proofread the manuscript and agreed on the data presented.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
AB received honorarium from Jazz, Adienne, and Sanofi. MM received honorarium from Jazz, Riemser, and Sanofi. EA reports personal fees from Novartis, Jazz Pharmaceuticals, Bluebird Bio, Roche, Celgene, Vertex Pharmaceuticals, and CRISPR Therapeutics all outside the submitted work. All remaining authors do not have any conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bazarbachi, A., Labopin, M., Blaise, D. et al. Comparable outcomes of haploidentical transplant with TBF conditioning versus matched unrelated donor with fludarabine/busulfan conditioning for acute myeloid leukemia. Bone Marrow Transplant 56, 622–634 (2021). https://doi.org/10.1038/s41409-020-01074-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01074-z
This article is cited by
-
Reduced intensity versus non-myeloablative conditioning regimen for haploidentical transplantation and post-transplantation cyclophosphamide in complete remission acute myeloid leukemia: a study from the ALWP of the EBMT
Bone Marrow Transplantation (2022)
-
Post-transplant cyclophosphamide in one-antigen mismatched unrelated donor transplantation versus haploidentical transplantation in acute myeloid leukemia: a study from the Acute Leukemia Working Party of the EBMT
Bone Marrow Transplantation (2022)