Abstract
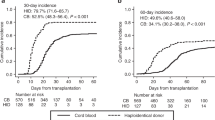
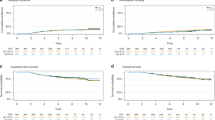
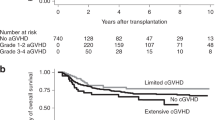
Graft failure (GF) is a life-threatening complication after allogeneic stem cell transplantation. Although salvage cord blood transplantation (CBT) is a curative therapy for GF, the optimal immunosuppression after salvage CBT remains unknown. Using nationwide registration data, we compared the transplant outcomes of patients who developed GF and underwent salvage CBT using immunosuppressants, including calcineurin (CNI) alone (n = 177); CNI plus methotrexate (CNI+MTX, n = 150); and CNI plus mycophenolate mofetil (CNI+MMF, n = 161). The CNI+MMF group, in comparison with the CNI+MTX and CNI alone groups, demonstrated better neutrophil recovery at 30 days (62.7 vs. 42.7 vs. 53.1%, P < 0.001); better overall survival (OS) at 12 months (48.4 vs. 33.5 vs. 28.3%, P < 0.001); and lower non-relapse mortality (NRM) at 12 months (35.2 vs. 53.9 vs. 56.5%, P < 0.001). On multivariate analysis, CNI+MMF had the best neutrophil recovery (hazard ratio (HR), 1.71; P < 0.001) and OS (HR, 0.64; P = 0.002) and the lowest NRM (HR, 0.53; P < 0.001). Hemorrhage was relatively less frequent in the CNI+MMF group. CNI+MMF can be a promising immunosuppressant regimen after salvage CBT for GF, with better engraftment and survival outcomes, compared with CNI alone and CNI+MTX.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, et al. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transpl. 2013;48:537–43.
Cluzeau T, Lambert J, Raus N, Dessaux K, Absi L, Delbos F, et al. Risk factors and outcome of graft failure after HLA matched and mismatched unrelated donor hematopoietic stem cell transplantation: a study on behalf of SFGM-TC and SFHI. Bone Marrow Transplant. 2016;51:687–91.
Narimatsu H, Kami M, Miyakoshi S, Murashige N, Yuji K, Hamaki T, et al. Graft failure following reduced-intensity cord blood transplantation for adult patients. Br J Haematol. 2006;132:36–41.
Wobma H, Jin Z, Moscoso S, Bhatia M, Broglie L, George D, et al. Risk factors, clinical outcomes, and cost-of-care related to graft failure in pediatric allogeneic hematopoietic cell transplant recipients. Biol Blood Marrow Transplant. 2020;S1083-8791:30146–4.
Kawashima N, Terakura S, Nishiwaki S, Koyama D, Ozawa Y, Ito M, et al. Increase of bone marrow macrophages and CD8+ T lymphocytes predict graft failure after allogeneic bone marrow or cord blood transplantation. Bone Marrow Transplant. 2017;52:1164–70.
Ciurea SO, Thall PF, Milton DR, Barnes TH, Kongtim P, Carmazzi Y, et al. Complement-binding donor-specific anti-HLA antibodies and risk of primary graft failure in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2015;21:1392–8.
Kongtim P, Cao K, Ciurea SO. Donor specific anti-HLA antibody and risk of graft failure in haploidentical stem cell transplantation. Adv Hematol. 2016;2016:4025073.
Martin PJ. Prevention of allogeneic marrow graft rejection by donor T cells that do not recognize recipient alloantigens: potential role of a veto mechanism. Blood. 1996;88:962–9.
Kong Y, Wang YT, Hu Y, Han W, Chang YJ, Zhang XH, et al. The bone marrow microenvironment is similarly impaired in allogeneic hematopoietic stem cell transplantation patients with early and late poor graft function. Bone Marrow Transplant. 2016;51:249–55.
Selleri C, Sato T, Anderson S, Young NS, Maciejewski JP. Interferon-gamma and tumor necrosis factor-alpha suppress both early and late stages of hematopoiesis and induce programmed cell death. J Cell Physiol. 1995;165:538–46.
Alcazer V, Conrad A, Valour F, Bachy E, Salles G, Huynh A, et al. Early-onset severe infections in allogeneic hematopoietic stem cell transplantation recipients with graft failure. Am J Hematol. 2019;94:E109–11.
Masouridi-Levrat S, Simonetta F, Chalandon Y. Immunological basis of bone marrow failure after allogeneic hematopoietic stem cell transplantation. Front Immunol. 2016;7:362.
Ozdemir ZN, Civriz Bozdağ S. Graft failure after allogeneic hematopoietic stem cell transplantation. Transfus Apher Sci. 2018;57:163–7.
Sun YQ, He GL, Chang YJ, Xu LP, Zhang XH, Han W, et al. The incidence, risk factors, and outcomes of primary poor graft function after unmanipulated haploidentical stem cell transplantation. Ann Hematol. 2015;94:1699–705.
Shimada K, Narimatsu H, Morishita Y, Kohno A, Saito S, Kato Y. Severe regimen-related toxicity of second transplantation for graft failure following reduced-intensity cord blood transplantation in an adult patient. Bone Marrow Transplant. 2006;37:787–8.
Schriber J, Agovi MA, Ho V, Ballen KK, Bacigalupo A, Lazarus HM, et al. Second unrelated donor hematopoietic cell transplantation for primary graft failure. Biol Blood Marrow Transplant. 2010;16:1099–106.
Fuji S, Nakamura F, Hatanaka K, Taniguchi S, Sato M, Mori S, et al. Peripheral blood as a preferable source of stem cells for salvage transplantation in patients with graft failure after cord blood transplantation: a retrospective analysis of the registry data of the Japanese Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2012;18:1407–14.
Waki F, Masuoka K, Fukuda T, Kanda Y, Nakamae M, Yakushijin K, et al. Feasibility of reduced-intensity cord blood transplantation as salvage therapy for graft failure: results of a nationwide survey of adult patients. Biol Blood Marrow Transplant. 2011;17:841–51.
Lund TC, Liegel J, Bejanyan N, Orchard PJ, Cao Q, Tolar J, et al. Second allogeneic hematopoietic cell transplantation for graft failure: poor outcomes for neutropenic graft failure. Am J Hematol. 2015;90:892–6.
Onishi Y, Mori T, Kako S, Koh H, Uchida N, Kondo T, et al. Outcome of second transplantation using umbilical cord blood for graft failure after allogeneic hematopoietic stem cell transplantation for aplastic anemia. Biol Blood Marrow Transplant. 2017;23:2137–42.
Harada K, Fuji S, Seo S, Kanda J, Ueki T, Kimura F, et al. Comparison of the outcomes after haploidentical and cord blood salvage transplantations for graft failure following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020. https://doi.org/10.1038/s41409-020-0821-9.
Singh H, Nikiforow S, Li S, Ballen KK, Spitzer TR, Soiffer R, et al. Outcomes and management strategies for graft failure after umbilical cord blood transplantation. Am J Hematol. 2014;89:1097–101.
Tang BL, Zhu XY, Zheng CC, Liu HL, Geng LQ, Wang XB, et al. Successful early unmanipulated haploidentical transplantation with reduced-intensity conditioning for primary graft failure after cord blood transplantation in hematologic malignancy patients. Bone Marrow Transplant. 2015;50:248–52.
Prata PH, Resche-Rigon M, Blaise D, Socié G, Rohrlich PS, Milpied N, et al. Outcomes of salvage haploidentical transplant with post-transplant cyclophosphamide for rescuing graft failure patients: a report on behalf of the Francophone Society of Bone Marrow Transplantation and Cellular Therapy. Biol Blood Marrow Transplant. 2019;25:1798–802.
Hoshino T, Takada S, Hatsumi N, Sakura T. Feasibility of salvage cord blood transplantation using a fludarabine, melphalan, and low-dose anti-thymocyte globulin conditioning regimen. Int J Hematol. 2019;109:463–9.
Kato M, Matsumoto K, Suzuki R, Yabe H, Inoue M, Kigasawa H, et al. Salvage allogeneic hematopoietic SCT for primary graft failure in children. Bone Marrow Transplant. 2013;48:1173–8.
Terakura S, Wake A, Inamoto Y, Murata M, Sakai R, Yamaguchi T, et al. Exploratory research for optimal GvHD prophylaxis after single unit CBT in adults: short-term methotrexate reduced the incidence of severe GvHD more than mycophenolate mofetil. Bone Marrow Transplant. 2017;52:423–30.
Terakura S, Kuwatsuka Y, Yamasaki S, Wake A, Kanda J, Inamoto Y, et al. GvHD prophylaxis after single-unit reduced intensity conditioning cord blood transplantation in adults with acute leukemia. Bone Marrow Transplant. 2017;52:1261–7.
Kharfan-Dabaja M, Mhaskar R, Reljic T, Pidala J, Perkins JB, Djulbegovic B, et al. Mycophenolate mofetil versus methotrexate for prevention of graft-versus-host disease in people receiving allogeneic hematopoietic stem cell transplantation. Cochrane Database Syst Rev. 2014;7:CD010280.
Atsuta Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Kanda J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol. 2016;103:11–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Murata M, Nakasone H, Kanda J, Nakane T, Furukawa T, Fukuda T, et al. Clinical factors predicting the response of acute graft-versus-host disease to corticosteroid therapy: an analysis from the GVHD Working Group of the Japan Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2013;19:1183–9.
Pascal L, Tucunduva L, Ruggeri A, Blaise D, Ceballos P, Chevallier P, et al. Impact of ATG-containing reduced-intensity conditioning after single- or double-unit allogeneic cord blood transplantation. Blood. 2015;126:1027–32.
Yanada M, Konuma T, Kuwatsuka Y, Kondo T, Kawata T, Takahashi S, et al. Unit selection for umbilical cord blood transplantation for adults with acute myeloid leukemia in complete remission: a Japanese experience. Bone Marrow Transplant. 2019;54:1789–98.
Konuma T, Kato S, Oiwa-Monna M, Tanoue S, Ogawa M, Isobe M, et al. Cryopreserved CD34+ cell dose, but not total nucleated cell dose, influences hematopoietic recovery and extensive chronic graft-versus-host disease after single-unit cord blood transplantation in adult patients. Biol Blood Marrow Transplant. 2017;23:1142–50.
Fuji S, Tada Y, Nakata R, Nakata K, Koike M, Kida S, et al. GVHD prophylaxis by tacrolimus and mini-MTX in single-unit CBT: a single institute experience. Int J Hematol. 2020;111:278–83.
Fuji S, Oshima K, Ohashi K, Sawa M, Saito T, Eto T, et al. Impact of pretransplant donor-specific anti-HLA antibodies on cord blood transplantation on behalf of the Transplant Complications Working Group of Japan Society for Hematopoietic Cell Transplantation. Bone Marrow Transplant. 2019. https://doi.org/10.1038/s41409-019-0712-0.
Acknowledgements
We thank all the physicians and staff at the transplant centers who provided the clinical data to the Transplant Registry Unified Management Program of the Japan Society of Hematopoietic Cell Transplantation. This work was supported in part by the Practical Research Project for Allergic Diseases and Immunology (Research Technology of Medical Transplantation) from the Japan Agency for Medical Research and Development, AMED under Grant Number 18ek0510023h0002.
Transplant Complications Working Group of the Japan Society for Hematopoietic Cell Transplantation
Kaito Harada1, Shigeo Fuji2, Sachiko Seo3, Makoto Onizuka1, Hideki Nakasone17
GVHD Working Group of the Japan Society for Hematopoietic Cell Transplantation
Naoyuki Uchida4, Shingo Yano6, Sachiko Seo3, Hideki Nakasone17, Seitaro Terakura16
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the Transplant Complications Working Group of the Japan Society for Hematopoietic Cell Transplantation and GVHD Working Group of the Japan Society for Hematopoietic Cell Transplantation are listed below Acknowledgements
Supplementary information
Rights and permissions
About this article
Cite this article
Harada, K., Fuji, S., Seo, S. et al. Comparison of immunosuppressant regimens in salvage cord blood transplantation for graft failure after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 56, 400–410 (2021). https://doi.org/10.1038/s41409-020-00999-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-00999-9
This article is cited by
-
Salvage single-unit unrelated cord blood transplantation for graft failure following initial allogeneic transplantation in adult acute myeloid leukemia: trends in outcomes over the past 20 years
Bone Marrow Transplantation (2022)
-
Outcomes of salvage haploidentical transplantation using posttransplant cyclophosphamide for graft failure following allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2022)
-
Prognostic factors in salvage transplantation for graft failure following allogeneic hematopoietic stem cell transplantation
Bone Marrow Transplantation (2021)