Abstract
The outcome of allogeneic hematopoietic stem cell transplantation (allo-HSCT) for adult T-cell leukemia/lymphoma (ATL) is still unsatisfactory. To illustrate the advantages and disadvantages of each donor source, we performed a nationwide retrospective study of graft-versus-host disease (GVHD)-free, relapse-free survival (GRFS) of patients with allo-HSCT-treated ATL. One-year GRFS did not significantly differ between patients who received related bone marrow transplantation (R-BMT; 26%, n = 117), related peripheral blood stem cell transplantation (R-PBSCT; 22%, n = 225), unrelated bone marrow transplantation (UR-BMT; 26%, n = 619), and cord blood transplantation (CBT; 21%, n = 359; p = 0.09). This was attributable to a low incidence of systemically-treated chronic GVHD after CBT (9% at 1 year) and reduced non-GVHD/relapse mortality after R-PBSCT (9% at 1 year). Among patients transplanted in complete remission (CR), 1-year overall survival after CBT (52%, n = 132) was not inferior to that after R-BMT (55%, n = 51), R-PBSCT (57%, n = 79), and UR-BMT (58%, n = 280; p = 0.15), and relapse rates were equivalent among the four sources (p = 0.19). Our results suggest that all donor sources are feasible for CR patients and that GRFS provides important clues toward optimizing allo-HSCT for ATL.
Similar content being viewed by others
Introduction
Adult T-cell leukemia/lymphoma (ATL) is an aggressive T-cell neoplasm caused by human T-lymphotropic virus type 1 [1] and has a poor prognosis [2,3,4]. Intensive chemotherapy and autologous stem cell transplantation have definite limitations [5,6,7,8,9]. Although allogeneic hematopoietic stem cell transplantation (allo-HSCT) may provide long-term remission [10,11,12,13], the 3-year survival rate after this procedure is only 33–36% in Japan [14, 15], and similar outcomes have been reported in Europe [16]. Given that grade I–II acute graft-versus-host disease (GVHD) is associated with better overall survival (OS) [17,18,19], graft-versus-leukemia (GVL) effects induced by donor lymphocytes are important in ATL [20, 21]. Mild to moderate GVHD is therefore likely to be beneficial in ATL; however, severe GVHD is associated with non-relapse mortality [17]. Thus, it is difficult to optimize the balance between GVHD and GVL effects while avoiding infection in patients who undergo allo-HSCT for ATL.
Efforts to reduce GVHD decreased transplant-related morbidity/mortality but increased risk of relapse, which may be attributable to diminished GVL effects [22]. On the other hand, efforts to reduce relapse-related mortality by delivering enhanced high-dose chemotherapy prior to allo-HSCT led to excess deaths due to organ damage, infections, and GVHD [23]. The final goal of allo-HSCT is to avoid relapse, severe GVHD, and other fatal complications. Therefore, GVHD-free, relapse-free survival (GRFS), defined as the absence of grade III–IV acute GVHD, chronic GVHD that requires systemic treatment, relapse, and death, has been proposed as a novel and clinically meaningful endpoint of allo-HSCT [24]. Cord blood transplantation (CBT) reportedly provides favorable GRFS compared with transplantation from other donor sources in some Japanese populations [25]. The median age of ATL patients is higher and the incidence of fatal opportunistic infection in ATL patients is higher than in patients with other hematologic malignancies [26]. Therefore, we hypothesized that GRFS of ATL patients may differ from that of patients with other hematologic malignancies.
As most ATL patients are over 60 years old, many will not have human leukocyte antigen (HLA)-matched healthy siblings of appropriate age to be eligible as donors. Therefore, alternative donor sources are often utilized in ATL. Among several donor sources, CBT is often performed, especially in patients with relapsing or refractory ATL [27]. This is because such cases require rapid transplantations and the availability of cord blood has recently improved in Japan [28]. HLA-haploidentical transplantation (haplo-HSCT) is also available. However, such transplants are associated with transplant-related mortality and limited quality of life (QOL) [29]. OS of ATL patients who underwent CBT between 1996 and 2005 was inferior to that of ATL patients who underwent transplantation from other donor sources [14]. Beneficial outcomes of CBT for chemotherapy-sensitive ATL are reported to be feasible [30, 31], although these findings should be verified in a larger study. Furthermore, CBT results in a low incidence of GVHD [32], which raises concerns about diminished GVL effects and higher relapse rates. Given that the outcome of CBT for other hematologic malignancies improved after 2006 [33], the limitations and advantages of CBT for ATL should be reevaluated.
Here, we conducted a nationwide retrospective study focusing on OS and GRFS of patients with allo-HSCT-treated ATL after 2006 and compared GRFS among patients who underwent transplantation from different donor sources. Our results illustrate several important advantages and disadvantages of transplantation from each donor source, which may help to improve the overall outcome of allo-HSCT for ATL.
Methods
Data collection
Data of 1363 patients with ATL who first underwent allo-HSCT between 2006 and 2015 in Japan were retrospectively analyzed. Allo-HSCT recipient clinical data were collected by the Japan Society for Hematopoietic Cell Transplantation (JSHCT) using the Transplant Registry Unified Management Program (TRUMP) [34, 35]. This analysis included the following clinical characteristics of the patients: age at transplantation, gender, disease status at transplantation, date of transplantation, duration from diagnosis to transplantation, and conditioning regimens. The numbers of HLA antigen mismatches in CBT, related bone marrow transplantation (R-BMT), and related peripheral blood stem cell transplantation (R-PBSCT) were counted with respect to HLA-A, -B, and -DRB1. Haplo-HSCT was defined as transplantation with two to three HLA mismatches in the graft-versus-host direction. The number of HLA allelic mismatches in unrelated bone marrow transplantation (UR-BMT) was counted with respect to HLA-A, -B, -C, and -DRB1. The present study was approved by the data management committees of the JSHCT as well as the Institutional Review Board of the Kyoto University Graduate School of Medicine. All patients provided consent to participate in the present study.
Definition of endpoints
OS was defined as the duration from transplantation to death, and the patients who remained alive at the final follow-up were censored. GRFS was defined as the duration from transplantation until death, relapse, development of grade III–IV acute GVHD, or development of chronic GVHD that required systemic treatment, and the patients without any of these events at the time of the final follow-up were censored. The relapse date of patients who did not achieve complete remission (CR) before and after transplantation was defined as day 0.1. Non-GVHD/relapse mortality (NGRM) was defined as the incidence of deaths without relapse, development of grade III–IV acute GVHD, or development of chronic GVHD that required systemic treatment. Patients were divided into two groups according to the conditioning regimens: myeloablative conditioning (MAC) and reduced intensity conditioning (RIC). MAC and RIC were defined according to the proposals of Giralt et al. [36] and Bacigalupo et al. [37] respectively.
Statistical analysis
Descriptive statistics were used to summarize variables related to the demographics and clinical characteristics of the patients. Groups were compared using Fisher’s exact test as appropriate for categorical variables and the Kruskal–Wallis test for continuous variables. The Mann–Whitney U test was used as a nonparametric test to compare two groups. The probabilities of OS and GRFS were estimated according to the Kaplan–Meier method, and univariable comparisons among the groups were performed using the log-rank test. The Cox proportional hazard model was used for multivariate analysis of OS and GRFS. The cumulative incidence rates of relapse and GVHD were estimated, and death without these events was considered as a competing factor. NGRM was also estimated, and its competing events were relapse, grade III–IV acute GVHD, and systemically-treated chronic GVHD. Results were expressed as hazard ratios and their 95% confidence intervals (CI). All tests were two-sided, and a p value of <0.05 was considered to indicate statistical significance. All statistical analyses were performed using Stata (version 13.0, Stata Corporation) and EZR (Saitama Medical Center, Jichi Medical University), a graphical user interface for R (The R Foundation for Statistical Computing, version 2.3.0) [38]. The shared scripts from the TRUMP data were used in the analyses [39].
Results
Characteristics of the patients
The median patient age was 57 years (range: 20–78 years) and the median observation period of survivors was 3.1 years (range: 0.0–10.5 years). The number of CBTs performed in 2011–2015 (n = 240) was double the number performed in 2006–2010 (n = 119, p < 0.001). The median age of patients who underwent CBT was 59 years, which was higher than that of patients who underwent the other types of transplantation (p < 0.001). The proportion of patients in CR at transplantation was lower among those who underwent haplo-HSCT (25%), CBT (37%), and R-PBSCT (35%) than among those who underwent R-BMT (44%) and UR-BMT (45%; p = 0.023). The duration from diagnosis to transplantation was longer for patients who underwent UR-BMT than for patients who underwent the other types of transplantation (p < 0.001). The percentage of HLA-mismatched transplantations was lower among patients who underwent R-BMT (15%) and higher among patients who underwent CBT (96%; p < 0.001). These characteristics are summarized in Table 1. Details of conditioning regimens are summarized in Supplementary Table 1. Of the patients who received MAC, 55% received cyclophosphamide and total body irradiation, and 13% received busulfan and cyclophosphamide. Of the patients who received RIC, 55% received melphalan-based conditioning and 39% received busulfan-based conditioning.
OS
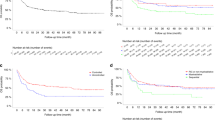
First, we compared R-BMT, R-PBSCT, UR-BMT, and CBT. In this analysis, we excluded patients who received haplo-HSCT as there were many fewer than those who received the other transplantation types. One-year OS was worse after CBT (38%, 95% CI: 32–43%) than after R-BMT (49%, 95% CI: 40–58%), R-PBSCT (52%, 95% CI: 45–58%), and UR-BMT (47%, 95% CI: 43–51%; p < 0.001; Fig. 1a). However, among patients in CR at transplantation, 1-year OS after CBT (52%, 95% CI: 43–60%, n = 132) was equivalent to that after R-BMT (55%, 95% CI: 41–68%, n = 51), R-PBSCT (57%, 95% CI: 45–67%, n = 79), and UR-BMT (58%, 95% CI: 52–63%, n = 280; p = 0.15; Fig. 1b). On the other hand, in the non-CR patients, 1-year OS after CBT (28%, 95% CI: 22–34%, n = 223) was inferior to that after R-BMT (45%, 95% CI: 33–57%, n = 63), R-PBSCT (49%, 95% CI: 41–57%, n = 147), and UR-BMT (39%, 95% CI: 34–44%, n = 337; p < 0.001; Fig. 1c).
Relapse
The 1-year cumulative incidence of relapse after CBT was 47% (95% CI: 42–52%), which was higher than that after R-BMT (40%, 95% CI: 31–49%), R-PBSCT (42%, 95% CI: 35–48%), and UR-BMT (35%, 95% CI: 31–39%; p = 0.003; Fig. 1d). Among patients in CR at transplantation, the 1-year cumulative incidence of relapse after CBT (26%, 95% CI: 19–34%) was not significantly different from that after R-BMT (31%, 95% CI: 18–44%), R-PBSCT (31%, 95% CI: 21–42%), and UR-BMT (21%, 95% CI: 16–26%; p = 0.19; Fig. 1e). On the other hand, among the patients in non-CR at transplantation, the 1-year cumulative incidence of relapse after CBT (60%, 95% CI: 53–66%) was higher than that after R-BMT (48%, 95% CI: 35–60%), R-PBSCT (47%, 95% CI: 39–55%), and UR-BMT (46%, 95% CI: 41–52%; p = 0.002; Fig. 1f).
GRFS
One-year GRFS did not significantly differ after CBT (21%, 95% CI: 17–26%), R-BMT (26%, 95% CI: 18–34%), R-PBSCT (22%, 95% CI: 16–27%), and UR-BMT (26%, 95% CI: 22–29%; p = 0.09; Fig. 2a). Among patients in CR at transplantation, GRFS did not differ among the four donor sources (CBT: 28%, 95% CI: 21–36%, R-BMT: 35%, 95% CI: 22–49%, R-PBSCT: 27%, 95% CI: 18–37%, and UR-BMT: 34%, 95% CI: 29–40% at 1 year; p = 0.49; Fig. 2b). Similarly, in the non-CR patients, GRFS did not differ among donor sources at 1 year (CBT: 16%, 95% CI: 12–22%, R-BMT: 19%, 95% CI: 11–30%, R-PBSCT: 18%, 95% CI: 13–25%, and UR-BMT: 19%, 95% CI: 15–23%; p = 0.25; Fig. 2c).
We also analyzed the first GRFS events in all the patients and those in CR at transplantation. The rate of NGRM after R-PBSCT (15%) was lower than that after the other transplantation types (26%) (p < 0.001), whereas the incidence of chronic GVHD that required systemic treatment after CBT (8%) was lower than that after the other transplantation types (19%, p < 0.001; Fig. 2d). Among patients in CR at transplantation, the proportion relapsing after CBT (29%) was similar to that after the other transplantation types (29%, p = 0.90), but CBT resulted in a higher rate of NGRM (41%) compared with the other transplantation types (28%, p = 0.014; Fig. 2e).
GVHD and NGRM
The 1-year cumulative incidence of grade III–IV acute GVHD after CBT was 11% (95% CI: 8–15%), which was lower than that after R-PBSCT (20%, 95% CI: 15–26%) and tended to be lower than that after R-BMT (17%, 95% CI: 10–24%) and UR-BMT (13%, 95% CI: 11–16%; p = 0.014; Fig. 3a). The percentage of patients with grade II acute GVHD after UR-BMT was 33%, which was higher than that after transplantation from the other donor sources (R-BMT: 23%, R-PBSCT: 24%, and CBT: 20%, p < 0.001). The percentage of patients with chronic GVHD that required systemic therapy at 1 year after CBT was 9% (95% CI: 6–12%), which was lower than that after transplantation from the other sources (R-BMT: 21%, 95% CI: 14–29%, R-PBSCT: 29%, 95% CI: 23–35%, and UR-BMT: 18%, 95% CI: 15–21%, p < 0.001; Fig. 3b). The 1-year NGRM after R-PBSCT was 9% (95% CI: 5–13%), which was lower than that after transplantation from the other sources (CBT: 20%, 95% CI: 16–24%, R-BMT: 12%, 95% CI: 7–19%, and UR-BMT: 16%, 95% CI: 13–19%; p < 0.001; Fig. 3c). Similar differences in the incidence of GVHD and NGRM were detected in both the CR and non-CR patients for each donor source.
Causes of NGRM are summarized in Table 2. The proportion of deaths caused by infection was significantly higher after CBT (50%) than after the other transplantation types (29%, p = 0.004). This result was associated with a higher incidence of graft failure after CBT (18%) than after the other transplantation types (7%, p < 0.001).
HLA matching status
Next, we compared the outcomes of HLA-matched transplantation with HLA-mismatched (including HLA-haploidentical) transplantation. OS, relapse, grade III–IV acute GVHD, chronic GVHD that required systemic treatment, NGRM, and GRFS did not significantly differ between patients who underwent HLA-matched BMT and those who underwent HLA-mismatched BMT (data not shown). PBSCT was divided into three groups: HLA 6/6-matched, 5/6-matched, and haploidentical in the graft-versus-host direction. The proportion of CR patients in each group was 35%, 29%, and 30%, respectively. For GVHD prophylaxis, 67% of the patients in the HLA 5/6-matched transplantation group received standard prophylaxis (calcineurin inhibitor plus methotrexate or mycophenolate mofetil), while 24% received anti-thymocyte globulin (ATG) and 4% posttransplant cyclophosphamide (PTCY), in addition to standard prophylaxis. In the haplo-HSCT group, 47% of patients received ATG, 25% PTCY, and 25% corticosteroids, in addition to standard prophylaxis. One-year OS after HLA-haploidentical PBSCT was 39% (95% CI: 23–55%), which tended to be inferior to that after HLA 6/6-matched (53%, 95% CI: 45–60%) and HLA 5/6-matched (49%, 95% CI: 33–62%) PBSCT (p = 0.11; Fig. 4a). GRFS did not significantly differ among these three groups (haploidentical: 22%, 95% CI: 10–36%, 6/6-matched: 20%, 95% CI: 15–26%, and 5/6-matched: 27%, 95% CI: 15–40% at 1 year; p = 0.69; Fig. 4b). There were no significant differences in the cumulative incidence of relapse after HLA 6/6-matched (40%, 95% CI: 32–47% at 1 year), HLA 5/6-matched (49%, 95% CI: 34–63%), and HLA-haploidentical (52%, 95% CI: 34–67%) PBSCT (p = 0.33; Fig. 4c). The cumulative incidences of grade III–IV acute GVHD, systemically-treated chronic GVHD, and NGRM did not differ among the groups (Fig. 4d–f).
Univariate and multivariate analysis of OS and GRFS
We performed univariate and multivariate analyses of OS and GRFS. In univariate analysis of OS, male sex, higher age (>50 years), worse performance status (PS >1), non-CR status at transplantation, and CBT were associated with lower OS (Table S2). Multivariate analysis revealed that male sex, higher age, worse PS, MAC, and non-CR status at transplantation were associated with lower OS, but CBT was not (Table S2). In univariate analysis of GRFS, male sex, higher age, worse PS, non-TBI conditioning, non-CR status at transplantation, and HLA mismatch were associated with lower GRFS (Table 3). Multivariate analysis revealed that male sex, higher age, worse PS, longer duration from diagnosis to transplantation (>180 days), and non-CR status at transplantation were associated with lower GRFS, whereas HLA mismatch was not (Table 3). Donor sources were not associated with GRFS, and the era of transplantation (2006–10 vs. 2011–15) was not associated with OS or GRFS (Table 3).
Discussion
The success of allo-HSCT is dependent on suppression of severe complications such as GVHD, relapse, infection, and vital organ failure. However, no one factor can predict long-term survival without ongoing morbidity. GRFS represents ideal recovery from allo-HSCT and is now recognized as an important treatment endpoint. Transplant-treated ATL patients often develop GVHD or other severe complications that lead to limited activity, and thus GRFS is also an important endpoint with respect to QOL. This is the first report of GRFS in ATL, and we have focused on differences in each component associated with GRFS among donor sources. We identified different advantages and disadvantages of each donor source, which provided clues to improve the outcome of allo-HSCT.
We made several important findings regarding CBT. Among patients in CR, OS and relapse rates after CBT were not inferior to those after transplantation from the other sources (Fig. 1b, d). GRFS did not significantly differ between patients who underwent CBT and those who underwent transplantation from the other donor sources (Fig. 2a–c). Whereas CBT was associated with a decrease in severe GVHD (Fig. 3a, b), relapse of CR patients after CBT was equivalent to that after transplantation from the other sources (Fig. 1c). These findings imply that the GVL effects of CBT are substantial for CR patients but may be limited in cases with a high tumor burden. On the other hand, the disadvantage of CBT was a high NGRM rate (Fig. 3c), which may be attributable to fatal opportunistic infections in many cases. This derives from delayed immune reconstitution after CBT, which should be further investigated.
In general, GRFS is shorter following PBSCT than BMT due to the higher incidence of chronic GVHD requiring systemic treatment [25]. In our study, however, the duration of GRFS was equivalent in PBSCT and BMT (Fig. 2a–c), due to the low NGRM rate after PBSCT. As described in Table 2, most of the NGRM derived from infectious complications. It is widely recognized that ATL patients often develop severe opportunistic infections [40]. In addition, infection-related mortality of transplant-treated ATL patients is higher than that of patients with other hematological malignancies [26]. PBSCT enables quick recovery of neutrophils and lymphocytes [41], which reduces severe infection. The benefits of reducing infection-related deaths following PBSCT in ATL may be greater than in other hematological malignances. In other words, quick immune reconstitution following PBSCT may be meaningful in ATL, although it remains to be verified in HLA-mismatched settings.
The cumulative incidence of severe GVHD tended to be higher after PBSCT (Fig. 3a, b); however, the relapse rate was not lower after PBSCT than after transplantation from the other donor sources (Fig. 1d, e). On the other hand, the incidence of grade II acute GVHD was higher and the cumulative incidence of relapse was lower after UR-BMT (Fig. 1d, e). These results suggest that moderate GVHD is associated with potent GVL effects and a reduced relapse rate, while severe GVHD is harmful and has no relapse suppression advantages. Many of the patients with severe GVHD possibly died of GVHD itself, infection, or organ failure before the appearance of GVL effects. These findings are compatible with those of another study, which looked at the impact of GVHD on outcomes after allo-HSCT for ATL [17].
In analysis of all hematological malignancies in Japan, GRFS was worse after HLA-mismatched transplantation than after HLA-matched transplantation. However, in the present study, HLA matching status did not influence GRFS in multivariate analysis (Table 3). Among patients who underwent PBSCT, the incidence of relapse tended to be higher after HLA-mismatched transplantation (Fig. 4c) and the incidence of grade III–IV acute GVHD tended to be lower after HLA 5/6-matched transplantation (Fig. 4d). This might be because patients who underwent HLA-mismatched transplantation received strong GVHD prophylaxis such as ATG, PTCY, and corticosteroids. These results suggest that adjusting the strength of GVHD prophylaxis may improve the outcome of HLA-mismatched transplantation in ATL. The relapse rate was not decreased following HLA-mismatched transplantation; therefore, we could not confirm the HLA-dependent GVL effects in ATL, which should be further explored. On the other hand, the relapse rate tended to be lower after unrelated transplantation (UR-BMT and CBT) than after related transplantation among patients in CR (Fig. 1e). GVL effects may be more potent after unrelated transplantation due to a mechanism other than HLA mismatch, such as mismatch of killer immunoglobulin-like receptor or its ligand polymorphisms [42].
Multivariate analysis revealed that male sex, higher age (>50 years), worse PS (>1), longer duration from diagnosis to transplantation (>180 days), and non-CR status at transplantation were associated with lower GRFS, which is consistent with the survey of GRFS in all hematological malignancies [25] and the report concerning early donor application for ATL patients [43]. Only 5% of the patients received ATG; therefore, a larger amount of data must be analyzed to clarify the association between ATG and GRFS in ATL. The outcome of allo-HSCT for non-CR ATL is still unsatisfactory. Many aspects of ATL therapy including conventional chemotherapy, conditioning regimens, GVHD prophylaxis, and maintenance therapies should be further optimized.
This study has inherent limitations that are common among observational studies. Eligibility for transplantation, as well as the choice of transplantation protocol including the selection of graft source, was determined by the treating physicians at each institution. The confounding effect of some variables, such as disease subtype, could not be evaluated because of missing data. Moreover, the data analyzed did not include information regarding the use of mogamulizumab or lenalidomide, which have both been shown to increase fatal GVHD [44,45,46,47].
The present study revealed that transplant from all donor sources is feasible for those patients in CR and that each source can be selected depending on the clinical characteristics of patients. Great efforts should be made to improve or avoid the shortcomings of alternative donor sources, which should ultimately improve the outcome of ATL.
Change history
09 February 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41409-020-01037-4
References
Uchiyama T, Yodoi J, Sagawa K, Takatsuki K, Uchino H. Adult T-cell leukemia: clinical and hematologic features of 16 cases. Blood. 1977;50:481–92.
Cook LB, Fuji S, Hermine O, Bazarbachi A, Ramos JC, Ratner L, et al. Revised adult T-cell leukemia-lymphoma international consensus meeting report. J Clin Oncol. 2019;37:677–87. https://doi.org/10.1200/JCO.18.00501.
Tsukasaki K, Fukushima T. JSH practical guidelines for hematological malignancies, 2018: II. lymphoma-8. adult T-cell leukemia-lymphoma. Int J Hematol. 2019;109:249–59. https://doi.org/10.1007/s12185-018-02588-5.
Ishitsuka K, Tamura K. Human T-cell leukaemia virus type I and adult T-cell leukaemia-lymphoma. Lancet Oncol. 2014;15:e517–26.
Tsukasaki K, Utsunomiya A, Fukuda H, Shibata T, Fukushima T, Takatsuka Y, et al. VCAP-AMP-VECP compared with biweekly CHOP for adult T-cell leukemia-lymphoma: Japan Clinical Oncology Group Study JCOG9801. J Clin Oncol. 2007;25:5458–64. https://doi.org/10.1200/JCO.2007.11.9958.
Tsukasaki K, Maeda T, Arimura K, Taguchi J, Fukushima T, Miyazaki Y, et al. Poor outcome of autologous stem cell transplantation for adult T cell leukemia/lymphoma: a case report and review of the literature. Bone Marrow Transplant. 1999;23:87–9. https://doi.org/10.1038/sj.bmt.1701533.
Phillips AA, Willim RD, Savage DG, Horwitz SM, Isola L, Zain JM, et al. A multi-institutional experience of autologous stem cell transplantation in North American patients with human T-cell lymphotropic virus type-1 adult T-cell leukemia/lymphoma suggests ineffective salvage of relapsed patients. Leuk Lymphoma. 2009;50:1039–42. https://doi.org/10.1080/10428190902887571.
Ratner L, Rauch D, Abel H, Caruso B, Noy A, Barta SK, et al. Dose-adjusted EPOCH chemotherapy with bortezomib and raltegravir for human T-cell leukemia virus-associated adult T-cell leukemia lymphoma. Blood Cancer J. 2016;6:e408. https://doi.org/10.1038/bcj.2016.21.
Ishida T, Jo T, Takemoto S, Suzushima H, Uozumi K, Yamamoto K, et al. Dose-intensified chemotherapy alone or in combination with mogamulizumab in newly diagnosed aggressive adult T-cell leukaemia-lymphoma: a randomized phase II study. Br J Haematol. 2015;169:672–82. https://doi.org/10.1111/bjh.13338.
Choi I, Tanosaki R, Uike N, Utsunomiya A, Tomonaga M, Harada M, et al. Long-term outcomes after hematopoietic SCT for adult T-cell leukemia/lymphoma: results of prospective trials. Bone Marrow Transplant. 2011;46:116–8. https://doi.org/10.1038/bmt.2010.92.
Fukushima T, Miyazaki Y, Honda S, Kawano F, Moriuchi Y, Masuda M, et al. Allogeneic hematopoietic stem cell transplantation provides sustained long-term survival for patients with adult T-cell leukemia/lymphoma. Leukemia. 2005;19:829–34.
Kami M, Hamaki T, Miyakoshi S, Murashige N, Kanda Y, Tanosaki R, et al. Allogeneic haematopoietic stem cell transplantation for the treatment of adult T-cell leukaemia/lymphoma. Br J Haematol. 2003;120:304–9.
Utsunomiya A, Miyazaki Y, Takatsuka Y, Hanada S, Uozumi K, Yashiki S, et al. Improved outcome of adult T cell leukemia/lymphoma with allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;27:15–20. https://doi.org/10.1038/sj.bmt.1702731.
Hishizawa M, Kanda J, Utsunomiya A, Taniguchi S, Eto T, Moriuchi Y, et al. Transplantation of allogeneic hematopoietic stem cells for adult T-cell leukemia: a nationwide retrospective study. Blood. 2010;116:1369–76. https://doi.org/10.1182/blood-2009-10-247510.
Ishida T, Hishizawa M, Kato K, Tanosaki R, Fukuda T, Taniguchi S, et al. Allogeneic hematopoietic stem cell transplantation for adult T-cell leukemia-lymphoma with special emphasis on preconditioning regimen: a nationwide retrospective study. Blood. 2012;120:1734–41. https://doi.org/10.1182/blood-2012-03-414490.
Bazarbachi A, Cwynarski K, Boumendil A, Finel H, Fields P, Raj K, et al. Outcome of patients with HTLV-1-associated adult T-cell leukemia/lymphoma after SCT: a retrospective study by the EBMT LWP. Bone Marrow Transplant. 2014;49:1266–8. https://doi.org/10.1038/bmt.2014.143.
Kanda J, Hishizawa M, Utsunomiya A, Taniguchi S, Eto T, Moriuchi Y, et al. Impact of graft-versus-host disease on outcomes after allogeneic hematopoietic cell transplantation for adult T-cell leukemia: a retrospective cohort study. Blood. 2012;119:2141–8. https://doi.org/10.1182/blood-2011-07-368233.
Ishida T, Hishizawa M, Kato K, Tanosaki R, Fukuda T, Takatsuka Y, et al. Impact of graft-versus-host disease on allogeneic hematopoietic cell transplantation for adult T cell leukemia-lymphoma focusing on preconditioning regimens: nationwide retrospective study. Biol Blood Marrow Transplant. 2013;19:1731–9. https://doi.org/10.1016/j.bbmt.2013.09.014.
Kato K, Choi I, Wake A, Uike N, Taniguchi S, Moriuchi Y, et al. Treatment of patients with adult T cell leukemia/lymphoma with cord blood transplantation: a Japanese nationwide retrospective survey. Biol Blood Marrow Transplant. 2014;20:1968–74. https://doi.org/10.1016/j.bbmt.2014.08.012.
Yonekura K, Utsunomiya A, Takatsuka Y, Takeuchi S, Tashiro Y, Kanzaki T, et al. Graft-versus-adult T-cell leukemia/lymphoma effect following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41:1029–35. https://doi.org/10.1038/bmt.2008.39.
Harashima N, Kurihara K, Utsunomiya A, Tanosaki R, Hanabuchi S, Masuda M, et al. Graft-versus-Tax response in adult T-cell leukemia patients after hematopoietic stem cell transplantation. Cancer Res. 2004;64:391–9.
Sehn LH, Alyea EP, Weller E, Canning C, Lee S, Ritz J, et al. Comparative outcomes of T-cell-depleted and non-T-cell-depleted allogeneic bone marrow transplantation for chronic myelogenous leukemia: impact of donor lymphocyte infusion. J Clin Oncol. 1999;17:561–8. https://doi.org/10.1200/JCO.1999.17.2.561.
Alyea E, Neuberg D, Mauch P, Marcus K, Freedman A, Webb I, et al. Effect of total body irradiation dose escalation on outcome following T-cell-depleted allogeneic bone marrow transplantation. Biol Blood Marrow Transplant. 2002;8:139–44.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8. https://doi.org/10.1182/blood-2014-10-609032.
Inamoto Y, Kimura F, Kanda J, Sugita J, Ikegame K, Nakasone H, et al. Comparison of graft-versus-host disease-free, relapse-free survival according to a variety of graft sources: antithymocyte globulin and single cord blood provide favorable outcomes in some subgroups. Haematologica. 2016;101:1592–602. https://doi.org/10.3324/haematol.2016.149427.
Itonaga H, Taguchi J, Fukushima T, Tsushima H, Sato S, Ando K, et al. Distinct clinical features of infectious complications in adult T cell leukemia/lymphoma patients after allogeneic hematopoietic stem cell transplantation: a retrospective analysis in the Nagasaki transplant group. Biol Blood Marrow Transplant. 2013;19:607–15. https://doi.org/10.1016/j.bbmt.2013.01.011.
Fujiwara H, Fuji S, Wake A, Kato K, Takatsuka Y, Fukuda T, et al. Dismal outcome of allogeneic hematopoietic stem cell transplantation for relapsed adult T-cell leukemia/lymphoma, a Japanese nation-wide study. Bone Marrow Transplant. 2017;52:484–8. https://doi.org/10.1038/bmt.2016.313.
Uchida N. Cord blood transplantation in Japan. Rinsho Ketsueki. 2016;57:531–6. https://doi.org/10.11406/rinketsu.57.531.
Yoshimitsu M, Utsunomiya A, Fuji S, Fujiwara H, Fukuda T, Ogawa H, et al. A retrospective analysis of haplo-identical HLA-mismatch hematopoietic transplantation without posttransplantation cyclophosphamide for GVHD prophylaxis in patients with adult T-cell leukemia-lymphoma. Bone Marrow Transplant. 2018. https://doi.org/10.1038/s41409-018-0400-5.
Fukushima T, Itonaga H, Moriuchi Y, Yoshida S, Taguchi J, Imaizumi Y, et al. Feasibility of cord blood transplantation in chemosensitive adult T-cell leukemia/lymphoma: a retrospective analysis of the Nagasaki Transplantation Network. Int J Hematol. 2013;97:485–90. https://doi.org/10.1007/s12185-013-1307-y.
Nakamura T, Oku E, Nomura K, Morishige S, Takata Y, Seki R, et al. Unrelated cord blood transplantation for patients with adult T-cell leukemia/lymphoma: experience at a single institute. Int J Hematol. 2012;96:657–63. https://doi.org/10.1007/s12185-012-1177-8.
Atsuta Y, Suzuki R, Nagamura-Inoue T, Taniguchi S, Takahashi S, Kai S, et al. Disease-specific analyses of unrelated cord blood transplantation compared with unrelated bone marrow transplantation in adult patients with acute leukemia. Blood. 2009;113:1631–8. https://doi.org/10.1182/blood-2008-03-147041.
Ballen KK, Gluckman E, Broxmeyer HE. Umbilical cord blood transplantation: the first 25 years and beyond. Blood. 2013;122:491–8. https://doi.org/10.1182/blood-2013-02-453175.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–74. https://doi.org/10.1532/IJH97.06239.
Atsuta Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10. https://doi.org/10.1007/s12185-015-1894-x.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33. https://doi.org/10.1016/j.bbmt.2009.07.004.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244.
Kanda J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol. 2016;103:11–9. https://doi.org/10.1007/s12185-015-1907-9.
Shimoyama M. Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984-87). Br J Haematol. 1991;79:428–37. https://doi.org/10.1111/j.1365-2141.1991.tb08051.x.
Pavletic ZS, Joshi SS, Pirruccello SJ, Tarantolo SR, Kollath J, Reed EC, et al. Lymphocyte reconstitution after allogeneic blood stem cell transplantation for hematologic malignancies. Bone Marrow Transplant. 1998;21:33–41. https://doi.org/10.1038/sj.bmt.1701037.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295:2097–100. https://doi.org/10.1126/science.1068440.
Fuji S, Fujiwara H, Nakano N, Wake A, Inoue Y, Fukuda T, et al. Early application of related SCT might improve clinical outcome in adult T-cell leukemia/lymphoma. Bone Marrow Transplant. 2016;51:205–11. https://doi.org/10.1038/bmt.2015.265.
Fuji S, Inoue Y, Utsunomiya A, Moriuchi Y, Uchimaru K, Choi I, et al. Pretransplantation anti-CCR4 antibody mogamulizumab against adult T-cell leukemia/lymphoma is associated with significantly increased risks of severe and corticosteroid-refractory graft-versus-host disease, nonrelapse mortality, and overall mortality. J Clin Oncol. 2016;34:3426–33. https://doi.org/10.1200/JCO.2016.67.8250.
Fuji S, Shindo T. Friend or foe? Mogamulizumab in allogeneic hematopoietic stem cell transplantation for adult T-cell leukemia/lymphoma. Stem Cell Investig. 2016;3:70. https://doi.org/10.21037/sci.2016.09.13.
Kneppers E, van der Holt B, Kersten MJ, Zweegman S, Meijer E, Huls G, et al. Lenalidomide maintenance after nonmyeloablative allogeneic stem cell transplantation in multiple myeloma is not feasible: results of the HOVON 76 Trial. Blood. 2011;118:2413–9. https://doi.org/10.1182/blood-2011-04-348292.
Coman T, Bachy E, Michallet M, Socié G, Uzunov M, Bourhis JH, et al. Lenalidomide as salvage treatment for multiple myeloma relapsing after allogeneic hematopoietic stem cell transplantation: a report from the French Society of Bone Marrow and Cellular Therapy. Haematologica. 2013;98:776–83. https://doi.org/10.3324/haematol.2012.069328.
Acknowledgements
We thank all the physicians and data managers at the participating institutions who contributed valuable data on transplantation for ATL to the JSHCT. We also thank the members of the data management committees of the JSHCT and the ATL working group for their assistance. The members of the ATL working group are listed below. This work was supported in part by the Practical Research Project for Allergic Diseases and Immunology (Research Technology of Medical Transplantation) from AMED, the Japan Agency for Medical Research and Development (grant number 19ek0510023h0002). This work was presented as an abstract at the 62nd annual meeting of the American Society of Hematology, Orlando, FL, December 7th, 2019.
The ATL Working Group of the Japanese Society for Hematopoietic Cell Transplantation
Makoto Yoshimitsu15, Takashi Ishida16, Atae Utsunomiya2, Koji Kato7, Junji Suzumiya17, Tomomi Tobai18, Koichi Nakase19, Yuichiro Nawa19, Masakatsu Hishizawa1, Takuya Fukushima20, Atsushi Wake3, Ilseung Choi6, Yoshitaka Asakura21, Nobuaki Nakano2, Hiroshi Fujiwara22, Shinichiro Machida23, Yasushi Sawayama24, Yoshitaka Inoue25, Kazunori Imada26, Isao Yoshida27, Shigeo Fuji28, Takahiro Fukuda11, Takero Shindo1, Masahito Tokunaga2, Hiroyuki Muranushi1, Satoko Morishima20, Shohei Tomori29, Tomoki Iemura1, Takuya Shimizu1, Mari Morita-Fujita1.
Author information
Authors and Affiliations
Consortia
Contributions
HM, TS, and KK designed and organized the project, and wrote the paper. HM performed statistical analysis. M Hishizawa, MT, AW, and KK helped to write the paper. NN, TE, M Hidaka, IC, TM, NU, Y Moriuchi, Y Miyazaki, TF, TI, and YA contributed to data gathering. All the authors contributed to the final version of the paper and approved it for publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the ATL Working Group of the Japanese Society for Hematopoietic Cell Transplantation are listed below Acknowledgements
Supplementary information
Rights and permissions
About this article
Cite this article
Muranushi, H., Shindo, T., Hishizawa, M. et al. GVHD-free, relapse-free survival provides novel clues for optimizing allogeneic-HSCT for adult T-cell leukemia/lymphoma. Bone Marrow Transplant 56, 155–166 (2021). https://doi.org/10.1038/s41409-020-00996-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-00996-y
This article is cited by
-
A comparison of long-term outcomes by donor type in the era of post-transplantation cyclophosphamide for aggressive adult T-cell leukemia/lymphoma
Bone Marrow Transplantation (2024)
-
Selective histone deacetylase inhibitor after allo-HCT for T-cell acute lymphoblastic leukemia or T-cell lymphoma
Bone Marrow Transplantation (2024)