Abstract
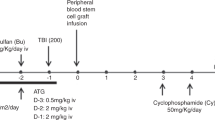
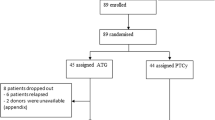
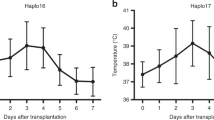
We report results of a thiotepa-based conditioning in haploidentical stem cell transplantation (haplo-SCT) with posttransplant cyclophosphamide (PT-CY) and antithymocyte globulin (ATG), for unmanipulated peripheral blood stem cell (PBSC) transplants, in 80 patients with hematological malignancies. Patients in complete remission (CR) received a thiotepa–busulfan–fludarabine (TBF) regimen, while patients with relapsed/refractory (R/R) malignancies received a sequential regimen consisting of thiotepa–etoposide–cyclophosphamide (TEC) and reduced-intensity conditioning (RIC). The median age was 52 (range, 17–72) years, 44% patients had R/R disease at transplant, and the median follow-up was 417 (range, 180–1595) days. The median days to neutrophil engraftment was 17 (range, 12–34). The cumulative incidences (CI) of acute graft-versus-host disease (GVHD) grade III to IV, severe chronic GVHD, nonrelapse mortality (NRM), and relapse were 16%, 16%, 26, and 26%, respectively. The 2-year overall survival (OS) and disease-free survival (DFS) were 53% and 47%, respectively. There were no significant differences between the patients in CR and R/R patients in terms of engraftment, GVHD, NRM, relapse, OS, or DFS. We conclude that thiotepa-based regimen with PT-CY can be modified with PBSC and ATG, still providing low toxicity, protection against GVHD, and low relapse incidence. Particularly encouraging are the results with the modification to sequential regimen in R/R patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Blood and Marrow Transplant Clinical Trials Network. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118:282–8.
McCurdy SR, Kanakry JA, Showel MM, Tsai HL, Bolanos-Meade J, Rosner GL, et al. Risk-stratified outcomes of nonmyeloablative HLA-haploidentical BMT with high-dose posttransplantation cyclophosphamide. Blood. 2015;125:3024–31.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant. 2013;19:117–22.
Bacigalupo A, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and post-transplant cyclophosphamide for hematologic malignancies following a myeloablative conditioning: an update. Bone Marrow Transpl. 2015;50:S37–39.
Bregante S, Dominietto A, Ghiso A, Raiola AM, Gualandi F, Varaldo R, et al. Improved outcome of alternative donor transplantations in patients with myelofibrosis: from unrelated to haploidentical family donors. Biol Blood Marrow Transplant. 2016;22:324–9.
Di Bartolomeo P, Santarone S, De Angelis G, Picardi A, Cudillo L, Cerretti R, et al. Haploidentical, unmanipulated, G-CSF-primed bone marrow transplantation for patients with high-risk hematologic malignancies. Blood. 2013;121:849–57.
Arcese W, Picardi A, Santarone S, De Angelis G, Cerretti R, Cudillo L, et al. Haploidentical, G-CSF-primed, unmanipulated bone marrow transplantation for patients with high-risk hematological malignancies: an update. Bone Marrow Transplant. 2015;50:S24–30.
Cutler C, Giri S, Jeyapalan S, Paniagua D, Viswanathan A, Antin JH. Acute and chronic graft-versus-host disease after allogeneic peripheral-blood stem cell and bone marrow transplantation: a meta-analysis. J Clin Oncol. 2001;19:3685–91.
Flowers ME, Parker PM, Johnston LJ, Matos AV, Storer B, Bensinger WI, et al. Comparison of chronic graft versus host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow up of a randomized trial. Blood. 2002;100:415–9.
Eapen M, Logan B, Confer DL, Haagenson M, Wagner JE, Weisdorf DJ, et al. Peripheral blood grafts from unrelated donors are associated with increased acute and chronic graft versus host disease without improved survival. Biol Blood Marrow Transplant. 2007;13:1461–8.
Anasetti C, Logan B, Lee S, Waller EK, Weisdorf DJ, Wingard JR, et al. Peripheral blood stem cells versus bone marrow from unrelated donors. New Engl J Med. 2012;367:1487–96.
Mohty M, Labopin M, Balère ML, Socie G, Milpied N, Tabrizi R, et al. Antithymocyte globulins and chronic graft-vs-host disease after myeloablative allogeneic stem cell transplantation from HLA-matched unrelated donors: a report from the Sociéte Française de Greffe de Moelle et de Thérapie Cellulaire. Leukemia. 2010;24:1867–74.
Bacigalupo A, Lamparelli T, Barisione G, Bruzzi P, Guidi S, Alessandrino PE, et al. Thymoglobulin prevents chronic graft-versus-host disease, chronic lung dysfunction, and late transplant-related mortality: long-term follow-up of a randomized trial in patients undergoing unrelated donor transplantation. Biol Blood Marrow Transplant. 2006;12:560–5.
Duléry R, Mohty M, Duhamel A, Robin M, Beguin Y, Michallet M, et al. Antithymocyte globulin before allogeneic stem cell transplantation for progressive myelodysplastic syndrome: a study from the French Society of Bone Marrow Transplantation and Cellular Therapy. Biol Blood Marrow Transplant. 2014;20:646–54.
Blaise D, Vey N, Faucher C, Mohty M. Current status of reduced-intensity-conditioning allogeneic stem cell transplantation for acute myeloid leukemia. Haematologica. 2007;92:533–41.
Khouri IF. Reduced-intensity regimens in allogeneic stem-cell transplantation for non-hodgkin lymphoma and chronic lymphocytic leukemia. Hematol Am Soc Hematol Educ Program. 2006;1:390–7.
Aoudjhane M, Labopin M, Gorin NC, Shimoni A, Ruutu T, Kolb HJ, et al. Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey from the Acute Leukemia Working Party (ALWP) of the European group for Blood and Marrow Transplantation (EBMT). Leukemia. 2005;19:2304–12.
Schmid C, Schleuning M, Schwerdtfeger R, Hertenstein B, Mischak-Weissinger E, Bunjes D, et al. Long-term survival in refractory acute myeloid leukemia after sequential treatment with chemotherapy and reduced-intensity conditioning for allogeneic stem cell transplantation. Blood. 2006;108:1092–9.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb H-J. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87.
Dulery R, Menard AL, Chantepie S, El-Cheikh J, Francois S, Delage J, et al. Sequential conditioning with thiotepa in T-cell replete hematopoietic stem cell transplantation for the treatment of refractory hematological malignancies: comparison with matched related, haplo-mismatched and unrelated donors. Biol Blood Marrow Transplant. 2018;24:1013–21.
Nguyen S, Chalandon Y, Lemarie C, Simon S, Masson D, Dhedin N, et al. Haploidentical hematopoietic stem cell transplantation: guidelines from the Francophone society of marrow transplantation and cellular therapy (SFGM-TC). Bull Cancer. 2016;103:S229–S242.
Hiddemann W, Martin WR, Sauerland CM, Heinecke A, Büchner T. Definition of refractoriness against conventional chemotherapy in acute myeloid leukemia: a proposal based on the results of retreatment by thioguanine, cytosine arabinoside, and daunorubicin (TAD 9) in 150 patients with relapse after standardized first line therapy. Leukemia. 1990;4:184–8.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol. 2003;21:4642–9.
Mohty M, Malard F, Blaise D, Milpied N, Socie G, Huynh A, et al. Sequential regimen of clofarabine, cytosine arabinoside and reduced intensity transplantation for primary refractory acute myeloid leukemia. Haematologica. 2016;102:184–91.
Stocker N, Duléry R, Battipaglia G, Brissot E, Médiavilla C, Sestili S, et al. Impact of cyclosporine A concentration on acute graft-vs-host disease incidence after haploidentical hematopoietic cell transplantation. Eur J Haematol. 2019;103:10–17.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. Consensus conference on acute GVHD grading. Bone Marrow Transpl. 1994;1995:825–8.
Jagasia MH, Greinix HT, Arora M, Wiliams KM, Wolff D, Cowen EW, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21:389–401.
De Vos J, Baudoux E, Bay J-O, Calmels B, Cras A, El Cheikh J, et al. Injections de lymphocytes du donneur (DLI)- recommandations de la Societe francophone de greffe de moelle et de therapie cellulaire (SGFM-TC). Bull Cancer. 2019;106:35–39.
Aversa F, Tabilio A, Velardi A, Cunningham I, Terenzi A, Falzetti F, et al. Treatment of high- risk acute leukemia with T-cell-depleted stem cells from related donors with one fully mismatched HLA haplotype. N Engl J Med. 1998;339:1186–93.
Rosales F, Naparstek E, Varadi G, Or R, Slavin S, Nagler A. The role of thiotepa in allogeneic stem cell transplantation in patients with leukemia. Leuk Res. 1999;23:947–52.
Eder S, Labopin M, Finke J, Bunjes D, Olivieri A, Santarone S, et al. Safety and efficacy of thiotepa-based conditioning for allogeneic transplantation in AML: a survey from the ALWP of the EBMT. Bone Marrow Transpl. 2017;52:238–44.
Saraceni M, Labopin M, Hamladji RM, Mufti G, Socie G, Shimoni A, et al. Thiotepa-busulfan-fludarabine compared to busulfan- fludarabine for sibling and unrelated donor transplant in acute myeloid leukemia in first remission. Oncotarget. 2018;9:3379–93.
Chiusolo P, Bug G, Olivieri A, Brune M, Mordini N, Alessandrino PE, et al. A modified post-transplant cyclophosphamide regimen, for unmanipulated haploidentical marrow transplantation, in acute myeloid leukemia: a multicenter study. Biol Blood Marrow Transplant. 2018;24:1243–9.
Berger M, Figari O, Bruno B, Raiola A, Dominietto A, Fiorone M, et al. Lymphocyte subsets recovery following allogeneic bone marrow transplantation (BMT): CD4þ cell count and transplant-related mortality. Bone Marrow Transpl. 2008;41:55–62.
Jaspers A, Baron F, Willems E, Seidel L, Hafraoui K, Vanstraelen G, et al. Erythropoietin therapy after allogeneic hematopoietic cell transplantation: a prospective, randomized trial. Blood. 2014;3:33–41.
Battipaglia G, Ruggeri A, Brissot E, Mamez AC, Malard F, Belhocine R, et al. Safety and feasibility of romiplostim treatment for patients with persistent thrombocytopenia after allogeneic stem cell transplantation. Bone Marrow Transpl. 2015;50:1574–7.
Castagna L, Bramanti S, Furst S, Giordano L, Crocchiolo R, Sarina B, et al. Nonmyeloablative conditioning, unmanipulated haploidentical SCT and post-infusion CY for advanced lymphomas. Bone Marrow Transpl. 2014;49:1475–80.
Raiola A, Dominietto A, Varaldo R, Ghiso A, Galaverna F, Bramanti S, et al. Unmanipulated haploidentical BMT following non- myeloablative conditioning and post-transplantation CY for advanced Hodgkin’s lymphoma. Bone Marrow Transpl. 2014;49:190–4.
Ruggeri A, Labopin M, Sanz G, Piemontese S, Arcese W, Bacigalupo A, et al. Comparison of outcomes after unrelated cord blood and unmanipulated haploidentical stem cell transplantation in adults with acute leukemia. Leukemia. 2015;29:1891–1900.
Ciurea SO, Mulanovich V, Saliba RM, Bayraktar UD, Jiang Y, Bassett R, et al. Improved early outcomes using a T cell replete graft compared with T cell depleted haploidentical hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:1835–44.
Bashey A, Zhang X, Jackson K, Brown S, Ridgeway M, Solh M, et al. Comparison of outcomes of hematopoietic cell transplants from T-replete haploidentical donors using post-transplantation cyclophosphamide with 10 of 10 HLA-A, -B, -C, -DRB1, and -DQB1 allele-matched unrelated donors and HLA-identical sibling donors: a multivariable analysis including disease risk index. Biol Blood Marrow Transplant. 2016;22:125–33.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6.
Raj K, Pagliuca A, Bradstock K, Noriega V, Potter V, Streetly M, et al. Peripheral blood hematopoietic stem cells for transplantation of hematological diseases from related, haploidentical donors after reduced-intensity conditioning. Biol Blood Marrow Transplant. 2014;20:881–903.
Oyekunle AA, Kröger N, Zabelina T, Ayuk F, Schieder H, Renges H, et al. Allogeneic stem-cell transplantation in patients with refractory acute leukemia: a long-term follow-up. Bone Marrow Transpl. 2006;37:45–50.
Singhal S, Powles R, Henslee-Downey PJ, Chiang KJ, Treleaven J, Godder K, et al. Allogeneic transplantation from HLA-matched sibling or partially HLA-mismatched related donors for primary refractory acute leukemia. Bone Marrow Transpl. 2002;29:291–5.
Mohty M, Malard F, Blaise D, Milpied N, Socie G, Huynh A, et al. Sequential regimen of clofarabine, cytosine arabinoside and reduced intensity transplantation for primary refractory acute myeloid leukemia. Haematologica. 2017;102:184–91.
Fraccaroli A, Prevalsek D, Fritsch S, Haebe S, Bucklein V, Schulz C, et al. Sequential HLA-haploidentical transplantation utilizing post-transplantation cyclophosphamide for GvHD prophylaxis inhigh-risk and relapsed/refractory AML/MDS. Am J Hematol. 2018;93:1524–31.
Goodyear OC, Dennis M, Jilani NY, Loke J, Siddique S, Ryan G, et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood. 2012;119:3361–9.
Guillame T, Malard F, Magro L, Labopin M, Tabrizi R, Borel C, et al. Prospective phase II study of prophylactic low-dose azacitidine and donor lymphocyte infusions following allogeneic hematopoietic stem cell transplantation for high-risk acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2019. https://doi.org/10.1038/s41409-019-0536-y. [Epub ahead of print].
Schiller GJ, Tuttle P, Desai P. Allogeneic hematopoietic stem cell transplantation in FLT3-ITD-positive acute myelogenous leukemia: the role for FLT3 tyrosine kinase inhibitors post-transplantation. Biol Blood Marrow Transplant. 2016;22:982–90.
Antar A, Otrock ZK, El-Cheikh J, Kharfan-Dabaja MA, Battipaglia G, Mahfouz R, et al. Inhibition of FLT3 in AML: a focus on sorafenib. Bone Marrow Transpl. 2017;52:344–51.
Battipaglia G, Ruggeri A, Massoud R, El-Cheikh J, Jestin M, Antar A, et al. Efficacy and feasibility of sorafenib as a maintenance agent after allogeneic hematopoietic stem cell transplantation for Fms-like tyrosine kinase 3-mutated acute myeloid leukemia. Cancer. 2017;123:2867–74.
Acknowledgements
We thank the nursing staff for providing excellent care for our patients.
Funding
This study was supported by the Association for Training, Education, and Research in Hematology, Immunology, and Transplantation. All authors declare no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Contributions
ZP collected, assembled, and analyzed data, performed statistical analysis, and wrote the first version of the manuscript. MM designed the study, supervised research, analyzed data, and helped writing the manuscript. RD and RM collected and assembled data. All other co-authors collected, assembled, and analyzed data; recruited patients; and helped write the manuscript. ML helped analyze data and commented on the manuscript. All authors approved submission of the manuscript for publication purposes.
Corresponding author
Ethics declarations
Conflict of interest
MM, RD, FM, and MTR have received honoraria for lectures from Keocyt, whose drug was included in this study. MM received honoraria for lectures from Sanofi, whose drug was included in this study. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Peric, Z., Mohty, R., Bastos, J. et al. Thiotepa and antithymocyte globulin-based conditioning prior to haploidentical transplantation with posttransplant cyclophosphamide in high-risk hematological malignancies. Bone Marrow Transplant 55, 763–772 (2020). https://doi.org/10.1038/s41409-019-0726-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0726-7
This article is cited by
-
Reduced post-transplant cyclophosphamide dose with antithymocyte globulin in peripheral blood stem cell haploidentical transplantation
Bone Marrow Transplantation (2023)
-
Reduced post-transplant cyclophosphamide doses in haploidentical hematopoietic cell transplantation for elderly patients with hematological malignancies
Bone Marrow Transplantation (2023)