Abstract
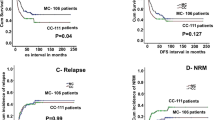
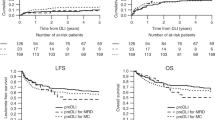
Compared to standard-conditioned regimens, reduced-intensity conditioning and T-cell depletion deliver lower transplant-related mortality and decreased graft-vs-host disease after allogeneic hematopoietic stem-cell transplantation. These advantages may however be mitigated by increased relapse rates and delays in achievement of full donor chimerism (FDC). Pre-emptive donor lymphocyte infusions (pDLI) facilitate the conversion of mixed (MDC) to FDC. However, there is a lack of published data on the risk/benefit analysis of this intervention. We performed a retrospective analysis of 119 patients who received 276 pDLI doses for falling CD3 chimerism, CD3 < 50% or mixed XX/XY karyotype. 71/119(60%) Patients achieved FDC, with only one reverting to MDC. Cumulative incidence (CI) of relapse at 5 years was significantly lower in the FDC group (16.0 vs 41.4%, p < 0.001). Those patients who achieved FDC had improved EFS (p < 0.001) and OS (p < 0.001). Interestingly, patients with FDC who developed DLI-induced graft-vs-host disease (GvHD) showed a similar outcome to those with MDC. The majority of patients who receive pDLI convert to FDC and retain that status. Achievement of FDC after pDLI impacts on survival, and those patients who achieve FDC without GvHD, experience maximum clinical benefit. Strategies to minimise DLI-induced GvHD should be considered to maximise the therapeutic potential of this intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Apperley J, Carreras E, Gluckman E, Masszi T. Haematopoietic stem cell transplantation. The EBMT Handbook, 6th ed; Paris: European School of Hematology; 2012.
Giralt S, Estey E, Albitar M, van Besien K, Rondón G, Anderlini P, et al. Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy. Blood. 1997;89:4531–6.
Parker JE, Shafi T, Pagliuca A, Mijovic A, Devereux S, Potter M, et al. Allogeneic stem cell transplantation in the myelodysplastic syndromes: interim results of outcome following reduced intensity conditioning compared with standard preparative regimens. Br J Haematol. 2002;119:144–54.
Wong R, Giralt SA, Martin T, Couriel DR, Anagnostopoulus A, Hosing C, et al. Reduced-intensity conditioning for unrelated donor hematopoietic stem cell transplantation as treatment for myeloid malignancies in patients older than 55 years. Blood. 2003;102:3052–9.
Tauro S, Graddock C, Peggs K, Begum G, Mahendra P, Cook G, et al. Allogeneic stem-cell transplantation using a reduced-intensity conditioning regimen has the capacity to produce durable remissions and long-term disease-free survival in patients with high-risk acute myeloid leukemia and myelodysplasia. J Clin Oncol. 2005;23:9387–93.
Blaise D, Farnault L, Faucher C, Marchetti N, Fürst S, El Cheikh J, et al. Reduced-intensity conditioning with Fludarabin, oral Busulfan, and thymoglobulin allows long-term disease control and low transplant-related mortality in patients with hematological malignancies. Exp Hematol. 2010;38:1241–50.
Ho AY, Pagliuca A, Kenyon M, Parker JE, Mijovic A, Devereux S, et al. Reduced-intensity allogeneic hematopoietic stem-cell transplantation for myelodysplastic syndrome and acute myeloid leukemia with multilineage dysplasia using fludarabine, busulphan and alemtuzumab (FBC) conditioning. Blood. 2004;104:1616–23.
van Besien K, Artz A, Smith S, Cao D, Rich S, Godley L, et al. Fludarabine, melphalan, and alemtuzumab in adults with standard-risk advanced acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5728–38.
Childs R, Clave E, Contentin N, Jayasekera D, Hensel N, Leitman S, et al. Engraftment kinetics after nonmyeloablative allogeneic peripheral blood stem cell transplantation: full donor T-cell chimerism precedes alloimmune responses. Blood. 1999;94:3234–41.
Busca A, Locatelli F, Flonta SE, Ciccone G, Baldi I, D’Ardia S, et al. In vivo T-cell depletion with pretransplant low-dose antithymocyte globulin is associated with reduced transplant-related mortality and improved clinical outcome in patients receiving allogeneic hematopoietic stem cell transplantation from unrelated and partially matched related donors. Am J Hematol. 2011;86:214–7.
Mackinnon S, Barnett L, Heller G, O’Reilly RJ. Minimal residual disease is more common in patients who have mixed T-cell chimerism after bone marrow transplantation for chronic myelogenous leukemia. Blood. 1994;83:3409–16.
Chang YJ, Huang XJ. Donor lymphocyte infusions for relapse after allogeneic transplantation: when, if and for whom? Blood Rev. 2013;27:55–62.
Schaap N, Schattenberg A, Mensink E, Preijers F, Hillegers M, Knops R, et al. Long-term follow-up of persisting mixed chimerism after partially T cell-depleted allogeneic stem cell transplantation. Leukemia. 2011;16:13–21.
Roddie C, Peggs KS. Donor lymphocyte infusion following allogeneic hematopoietic stem cell transplantation. Expert Opin Biol Ther. 2011;11:473–87.
Marks DI, Lush R, Cavenagh J, Milligan DW, Schey S, Parker A, et al. The toxicity and efficacy of donor lymphocyte infusions given after reduced-intensity conditioning allogeneic stem cell transplantation. Blood. 2002;100:3108–14.
Dey BR, McAfee S, Colby C, Sackstein R, Saidman S, Tarbell N, et al. Impact of prophylactic donor leukocyte infusions on mixed chimerism, graft-versus-host disease, and antitumor response in patients with advanced hematologic malignancies treated with nonmyeloablative conditioning and allogeneic bone marrow transplantation. Biol Blood Marrow Transplant. 2003;9:320–9.
Shaw BE, Byrne JL, Das-Gupta E, Carter GI, Russell NH. The impact of chimerism patterns and predonor leukocyte infusion lymphopenia on survival following T cell-depleted reduced-intensity conditioned transplants. Biol Blood Marrow Transplant. 2007;13:550–9.
Lim ZY, Pearce L, Ho AY, Barber L, Ingram W, Usai M, et al. Delayed attainment of full donor chimerism following alemtuzumab-based reduced-intensity condi- tioning haematopoeitic stem cell transplantation for acute myeloid leukaemia and myelodysplastic syndromes is associated with improved outcomes. Br J Haematol. 2007;138:517–26.
Huang XJ, Wang Y, Liu DH, Xu LP, Liu KY, Chen YH, et al. Administration of short-term immunosuppressive agents after DLI reduces the incidence of DLI-associated acute GVHD without influencing the GVL effect. Bone Marrow Transplant. 2009;44:309–16.
Huang XJ, Liu DH, Xu LP, Chen H, Han W, Liu KY, et al. Prophylactic infusion of donor granulocyte colony stimulating factor mobilized peripheral blood progenitor cells after allogeneic hematological stem cell transplantation in patients with high-risk leukemia. Leukemia. 2006;20:365–8.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W. Donor lymphocyte infusion for the treatment of leukemia relapse after HLA-mismatched/haploidentical T-cell-replete hematopoietic stem cell transplantation. Haematologica. 2007;92:414–7.
Yan C, Xu L, Liu D, Chen H, Wang I, Liu K, et al. Immunosuppression for 6-8 weeks after modified donor lymphocyte infusion reduced graft-versus-host disease without influencing graft-versus-leukemia effect in haploidentical transplant. Chin Med J. 2014;127:3602–9.
Yan CH, Xu LP, Liu DH, Chen H, Wang Y, Wang JZ, et al. Low-dose methotrexate may preserve a stronger antileukemic effect than that of cyclosporine after modified donor lymphocyte infusion in unmanipulated haploidentical HSCT. Clin Transplant. 2015;29:594–605.
Peggs KS, Thomson K, Hart DP, Geary J, Morris EC, Yong K, et al. Dose-escalated donor lymphocyte infusions following reduced intensity transplantation: toxicity, chimerism, and disease responses. Blood. 2004;103:1548–56.
Krishnamurthy P, Potter VT, Barber LD, Kulasekararaj AG, Lim ZY, Pearce RM, et al. Outcome of donor lymphocyte infusion after T cell-depleted allogeneic hematopoietic stem cell transplantation for acute myelogenous leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant. 2013;19:562–8.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–56.
Rujkiyanont P, Morris C, Kang G, Gan K, Hartford C, Triplett B, et al. Risk-adapted donor lymphocyte infusion based on chimerism and donor source in pediatric leukemia. Blood Cancer J. 2013;3:e137.
Schmid C, Labopin M, Nagler A, Bornhäuser M, Finke J, Fassas A, et al. Donor lymphocyte infusion in the treatment of first hematological relapse after allogeneic stem-cell transplantation in adults with acute myeloid leukemia: a retrospective risk factors analysis and comparison with other strategies by the EBMT Acute Leukemia Working Party. J Clin Oncol. 2007;25:4938–45.
Mackinnon S, Papadopoulus EB, Carabasi MH, Reich L, Collins NH, Boulad F, et al. Adoptive immunotherapy evaluating escalating doses of donor leukocytes for relapse of chronic myeloid leukemia after bone marrow transplantation: separation of graft-versus-leukemia responses from graft-versus-host disease. Blood. 1995;86:1261–8.
Giralt S, Hester J, Huh Y, Hirsch-Ginsberg C, Rondón G, Seong D, et al. CD8-depleted donor lymphocyte infusion as treatment for relapsed chronic myelogenous leukemia after allogeneic bone marrow transplantation. Blood. 1995;86:4337–43.
Bonini C, Ferrari G, Verzeletti S, Servida P, Zappone E, Ruggieri L, et al. HCV-TK gene transfer into donor lymphocytes for control of allogeneic graft-versus-leukemia. Science. 1997;276:1719–24.
Alyea EP, Soiffer RJ, Canning C, Neuberg D, Schlossman R, Pickett C, et al. Toxicity and efficacy of defined doses of CD4(+) donor lymphocytes for treatment of relapse after allogeneic bone marrow transplant. Blood. 1998;91:3671–80.
Wehler TC, Nonn M, Brandt B, Britten CM, Gröne M, Todorova M, et al. Targeting the activation-induced antigen CD137 can selectively deplete alloreactive T cells from antileukemic and antitumor donor T-cell lines. Blood. 2007;109:367–73.
Porter DL, Levine BL, Bunin N, Stadtmauer EA, Luger SM, Goldstein S, et al. A phase 1 trial of donor lymphocyte infusions expanded and activated ex vivo via CD3/CD28 costimulation. Blood. 2006;107:1325–31.
Acknowledgements
The authors would like to thank the support from the Instituto de Salud Carlos III (Madrid, Spain) and to anonymous reviewers who gave valuable suggestion that has helped to improve the quality of the paper. We would also like to thank Diego Calavia for the statistics review of the paper.
Authors contributions
Conception and design: JF, VP, LB, AP, and GM. Provision of study materials or patients: JF, VP, FG, JC, LF, CS, GO, MK, HL, KR, DM. Collection and assembly of data: JF, VP, JC, LF, CS, GO, AAA, MK, and PK. Data analysis and interpretation: JF, VP, FG. Paper writing: All authors. Final approval of paper: All authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feliu, J., Potter, V., Grimaldi, F. et al. Full donor chimerism without graft-versus-host disease: the key factor for maximum benefit of pre-emptive donor lymphocyte infusions (pDLI). Bone Marrow Transplant 55, 562–569 (2020). https://doi.org/10.1038/s41409-019-0695-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0695-x