Abstract
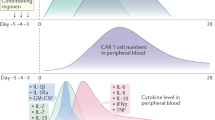
Adoptive immunotherapy with CD19-targeted chimeric antigen receptor (CAR)-T cells has been successful in producing durable remissions in some patients with relapsed or refractory B cell malignancies. Despite the efficacy of CAR-T cell therapy, significant toxicities can occur. Cytokine release syndrome (CRS) and neurotoxicity are the most common toxicities and can range from self-limited fever to life threatening organ damage and death. Understanding the mechanisms underlying these toxicities can help guide and improve outcomes. In this review we describe CRS and neurotoxicity in patients with B cell malignancies treated with CD19 CAR-T cells in pivotal trials, and also provide insight into potential mechanisms associated with these toxicities based on studies conducted in a phase 1/2 clinical trial at the Fred Hutchinson Cancer Research Center.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hay KA, Hanafi LA, Li D, Gust J, Liles WC, Wurfel MM, et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor-modified T-cell therapy. Blood. 2017;130:2295–306.
Gust J, Hay KA, Hanafi LA, Li D, Myerson D, Gonzalez-Cuyar LF, et al. Endothelial activation and blood-brain barrier disruption in neurotoxicity after adoptive immunotherapy with CD19 CAR-T cells. Cancer Discov. 2017;7:1404–19.
Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood Am Soc Hematol. 2014;124:188–95.
Turtle CJ, Hanafi L-A, Berger C, Hudecek M, Pender B, Robinson E, et al. Immunotherapy of non-Hodgkin’s lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells. Sci Transl Med Am Assoc Adv Sci. 2016;8:355ra116.
Turtle CJ, Hanafi L-A, Berger C, Gooley TA, Cherian S, Hudecek M, et al. CD19 CAR–T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J Clin Invest Am Soc Clin Investig. 2016;126:2123–38.
Gardner RA, Finney O, Annesley C, Brakke H, Summers C, Leger K, et al. Intent to treat leukemia remission by CD19CAR T cells of defined formulation and dose in children and young adults. Blood. 2017. https://doi.org/10.1182/blood-2017-02-769208
Porter D, Frey N, Wood PA, Weng Y, Grupp SA. Grading of cytokine release syndrome associated with the CAR T cell therapy tisagenlecleucel. J Hematol Oncol. 2018;11:35. https://jhoonline.biomedcentral.com/articles/ https://doi.org/10.1186/s13045-018-0571-y
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med Mass Med Soc. 2017;377:2531–44.
Yescarta. Package Insert. Kite Pharma Inc. Santa Monica, CA. 2018. https://www.fda.gov/downloads/UCM581226.pdf. Accessed 28 Aug 2018.
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378:439–48.
Kymriah. Package Insert. Novartis Pharmaceuticals Corporation, East Hanover, New Jersey. https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM573941.pdf. Accessed 28 Aug 2018.
Gragnano F, Sperlongano S, Golia E, Natale F, Bianchi R, Crisci M, et al. The role of von willebrand factor in vascular inflammation: from pathogenesis to targeted therapy. Mediat Inflamm. 2017;2017:5620314.
Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, et al. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med. 2006;12:235–9.
Augustin HG, Koh GY, Thurston G, Alitalo K. Control of vascular morphogenesis and homeostasis through the angiopoietin-Tie system. Nat Rev Mol Cell Biol. 2009;10:165–77.
Santomasso BD, Park JH, Salloum D, Riviere I, Flynn J, Mead E, et al. Clinical and biological correlates of neurotoxicity associated with CAR T-cell therapy in patients with B-cell acute lymphoblastic leukemia. Cancer Discov. 2018;8:958–71.
Torre M, Solomon IH, Sutherland CL, Nikiforow S, DeAngelo DJ, Stone RM, et al. Neuropathology of a case with fatal CAR T-cell-associated cerebral edema. J Neuropathol Exp Neurol. 2018;77:877–82.
Smyth LCD, Rustenhoven J, Park TIH, Schweder P, Jansson D, Heppner PA, et al. Unique and shared inflammatory profiles of human brain endothelia and pericytes. J Neuroinflammation. 2018;15:1–18.
Rustenhoven J, Jansson D, Smyth LC, Dragunow M. Brain pericytes as mediators of neuroinflammation. Trends Pharm Sci. 2017;38:291–304.
Taraseviciute A, Tkachev V, Ponce R, Turtle CJ, Snyder JM, Liggitt HD, et al. Chimeric antigen receptor T cell–mediated neurotoxicity in nonhuman primates. Cancer Discov. 2018;8:750–63.
Norelli M, Camisa B, Barbiera G, Falcone L, Purevdorj A, Genua M, et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat Med. 2018;24:739–48.
Giavridis T, van der Stegen SJC, Eyquem J, Hamieh M, Piersigilli A, Sadelain M. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat Med. 2018;24:731–8.
Acknowledgements
We thank the FHCRC Cell Processing Facility and Seattle Cancer Care Alliance (SCCA) Cell Therapy Laboratory, and the staff of the Program in Immunology and SCCA Immunotherapy Clinic.
Funding
Funding for this work was provided by: Bezos Family Foundation. Publication of this supplement was sponsored by Gilead Sciences Europe Ltd, Cell Source, Inc., The Chorafas Institute for Scientific Exchange of the Weizmann Institute of Science, Kiadis Pharma, Miltenyi Biotec, Celgene, Centro Servizi Congressuali, Almog Diagnostic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CKC declared no competing interests. CJT received consulting fees from Juno Therapeutics, Celgene, Nektar Therapeutics, Precision Biosciences, Eureka Therapeutics, Caribou Biosciences, Gilead, Bluebird, Adaptive Biotechnologies, Aptevo, research funding from Juno Therapeutics, Celgene, Nektar Therapeutics and holds patents licensed to cover technology related to cellular therapies with Juno/Celgene.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chou, C.K., Turtle, C.J. Insight into mechanisms associated with cytokine release syndrome and neurotoxicity after CD19 CAR-T cell immunotherapy. Bone Marrow Transplant 54 (Suppl 2), 780–784 (2019). https://doi.org/10.1038/s41409-019-0602-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-019-0602-5