Abstract
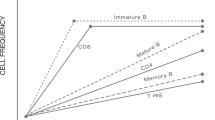
In the months that follow autologous hematopoietic stem cell transplantation (AHSCT), lymphopenia drives homeostatic proliferation, leading to oligoclonal expansion of residual cells. Here we evaluated how replicative senescent and exhausted cells associated with clinical outcomes of 25 systemic sclerosis (SSc) patients who underwent AHSCT. Patients were clinically monitored for skin (modified Rodnan’s skin score, mRSS) and internal organ involvement and had blood samples collected before and semiannually, until 3 years post-AHSCT, for quantification of telomere length, CD8+CD28− and PD-1+ cells, and serum cytokines. Patients were retrospectively classified as responders (n = 19) and non-responders (n = 6), according to clinical outcomes. At 6 months post-AHSCT, mRSS decreased (P < 0.001) and the pulmonary function stabilized, when compared with pre-transplant measures. In parallel, inflammatory cytokine (IL-6 and IL-1β) levels and telomere lengths decreased, whereas PD-1 expression on T-cells and the number of CD8+CD28− cells expressing CD57 and FoxP3 increased. After AHSCT, responder patients presented higher PD-1 expression on T- (P < 0.05) and B- (P < 0.01) cells, and lower TGF-β, IL-6, G-CSF (P < 0.01), and IL-1β, IL-17A, MIP-1α, and IL-12 (P < 0.05) levels than non-responders. Homeostatic proliferation after AHSCT results in transient telomere attrition and increased numbers of senescent and exhausted cells. High PD-1 expression is associated with better clinical outcomes after AHSCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Denton CP, Khanna D. Systemic sclerosis. Lancet. 2017;S0140-6736:30933–9.
Farge D, Labopin M, Tyndall A, Fassas A, Mancardi GL, Laar Van J, et al. Autologous hematopoietic stem cell transplantation for autoimmune diseases: an observational study on 12 years’ experience from the European Group for Blood and Marrow Transplantation Working Party on Autoimmune Diseases. Haematologica. 2010;95:284–92.
van Laar JM, Farge D, Sont JK, Naraghi K, Marjanovic Z, Larghero J, et al. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis. JAMA. 2014;311:2490–8.
Del Papa N, Onida F, Zaccara E, Saporiti G, Maglione W, Tagliaferri E, et al. Autologous hematopoietic stem cell transplantation has better outcomes than conventional therapies in patients with rapidly progressive systemic sclerosis. Bone Marrow Transplant. 2016;52:53–58.
Muraro Pa, Douek DC, Packer A, Chung K, Guenaga FJ, Cassiani-Ingoni R, et al. Thymic output generates a new and diverse TCR repertoire after autologous stem cell transplantation in multiple sclerosis patients. J Exp Med. 2005;201:805–16.
Delemarre EM, Van Den Broek T, Mijnheer G, Meerding J, Wehrens EJ, Olek S, et al. Autologous stem cell transplantation aids autoimmune patients by functional renewal and TCR diversification of regulatory T cells. Blood. 2016;127:91–101.
Abrahamsson SV, Angelini DF, Dubinsky AN, Morel E, Oh U, Jones JL, et al. Non-myeloablative autologous haematopoietic stem cell transplantation expands regulatory cells and depletes IL-17 producing mucosal-associated invariant T cells in multiple sclerosis. Brain. 2013;136:2888–903.
Farge D, Henegar C, Carmagnat M, Daneshpouy M, Marjanovic Z, Rabian C, et al. Analysis of immune reconstitution after autologous bone marrow transplantation in systemic sclerosis. Arthritis Rheum. 2005;52:1555–63.
Farge D, Arruda LCM, Brigant F, Clave E, Douay C, Marjanovic Z, et al. Long-term immune reconstitution and T cell repertoire analysis after autologous hematopoietic stem cell transplantation in systemic sclerosis patients. J Hematol Oncol. 2017;10:21.
Alexander T, Thiel A, Rosen O, Massenkeil G, Sattler A, Kohler S, et al. Depletion of autoreactive immunologic memory followed by autologous hematopoietic stem cell transplantation in patients with refractory SLE induces long-term remission through de novo generation of a juvenile and tolerant immune system. Blood. 2009;113:214–23.
Lucas C. M. Arruda, Kelen C. R. Malmegrim, João R. Lima-Júnior, Emmanuel Clave, Juliana B. E. Dias, Daniela A. Moraes, Corinne Douay, Isabelle Fournier, Hélène Moins-Teisserenc, Antônio José Alberdi, Dimas T. Covas, Belinda P. Simões, Pauline Lansiaux, Antoine Toubert, Maria Carolina Oliveira, (2018) Immune rebound associates with a favorable clinical response to autologous HSCT in systemic sclerosis patients. Blood Advances 2 (2):126–141
Arruda LCM, Lorenzi JCC, Sousa APA, Zanette DL, Palma PVB, Panepucci RA, et al. Autologous hematopoietic SCT normalizes miR-16, -155 and -142-3p expression in multiple sclerosis patients. Bone Marrow Transplant. 2015;50:380–9.
Arruda LCM, de Azevedo JTC, de Oliveira GLV, Scortegagna GT, Rodrigues ES, Palma PVB, et al. Immunological correlates of favorable long-term clinical outcome in multiple sclerosis patients after autologous hematopoietic stem cell transplantation. Clin Immunol. 2016;169:47–57.
Wu Z, Bensinger SJ, Zhang J, Chen C, Yuan X, Huang X, et al. Homeostatic proliferation is a barrier to transplantation tolerance. Nat Med. 2004;10:87–92.
Muraro PA, Robins H, Malhotra S, Howell M, Phippard D, Desmarais C, et al. T cell repertoire following autologous stem cell transplantation for multiple sclerosis. J Clin Invest. 2014;124:1168–72.
O’Donovan A, Pantell MS, Puterman E, Dhabhar FS, Blackburn EH, Yaffe K, et al. Cumulative inflammatory load is associated with short leukocyte telomere length in the Health, Aging and Body Composition Study. PLoS ONE. 2011;6:e19687.
Calado RT, Young NS. Telomere diseases. N Engl J Med. 2009;361:2353–65.
Akiyama M, Asai O, Kuraishi Y, Urashima M, Hoshi Y, Sakamaki H, et al. Shortening of telomeres in recipients of both autologous and allogeneic hematopoietic stem cell transplantation. Bone Marrow Transpl. 2000;25:441–7.
Rufer N, Brümmendorf TH, Chapuis B, Helg C, Lansdorp PM, Roosnek E. Accelerated telomere shortening in hematological lineages is limited to the first year following stem cell transplantation. Blood. 2001;97:575–7.
Robertson J, Testa N, Russell N, Jackson G, Parker A, Milligan D, et al. Telomere length Accelerated telomere shortening following allogeneic transplantation is independent of the cell source and occurs within the first year post transplant. Bone Marrow Transplant. 2001;27:1283–6.
Peffault de Latour R, Calado RT, Busson M, Abrams J, Adoui N, Robin M, et al. Age-adjusted recipient pre-transplant telomere length and treatment-related mortality after hematopoietic stem cell transplantation. Blood. 2012;120:3353–9.
Van Den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Arthritis Rheum. 2013;65:2737–47.
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA, et al. Scleroderma (systemic sclerosis): Classification, subsets and pathogenesis. J Rheumatol. 1988;15:202–5.
Burt RK, Oliveira MC, Shah SJ, Moraes DA, Simoes B, Gheorghiade M, et al. Cardiac involvement and treatment-related mortality after non-myeloablative haemopoietic stem-cell transplantation with unselected autologous peripheral blood for patients with systemic sclerosis: a retrospective analysis. Lancet. 2013;381:1116–24.
Malmegrim KCR, de Azevedo JTC, Arruda LCM, Abreu JRF, Couri CEB, de Oliveira GLV, et al. Immunological balance is associated with clinical outcome after autologous hematopoietic stem cell transplantation in type 1 diabetes. Front Immunol. 2017;8:167.
Cawthon RM. Telomere length measurement by a novel monochrome multiplex quantitative PCR method. Nucleic Acids Res. 2009;37:e21.
Ruijter JM, Ramakers C, Hoogaars WMH, Karlen Y, Bakker O, van den Hoff MJB, et al. Amplification efficiency: linking baseline and bias in the analysis of quantitative PCR data. Nucleic Acids Res. 2009;37:e45–e45.
Frisullo G, Nociti V, Iorio R, Plantone D, Patanella AK, Tonali PA, et al. CD8+Foxp3+T cells in peripheral blood of relapsing-remitting multiple sclerosis patients. Hum Immunol. 2010;71:437–41.
Beres AJ, Haribhai D, Chadwick AC, Gonyo PJ, Williams CB, Drobyski WR. CD8+Foxp3+regulatory T cells are induced during graft-versus-host disease and mitigate disease severity. J Immunol. 2012;189:464–74.
Sun W, Popat U, Hutton G, Zang YCQ, Krance R, Carrum G, et al. Characteristics of T-cell receptor repertoire and myelin-reactive T cells reconstituted from autologous haematopoietic stem-cell grafts in multiple sclerosis. Brain. 2004;127:996–1008.
Darlington PJ, Touil T, Doucet JS, Gaucher D, Zeidan J, Gauchat D, et al. Diminished Th17 (not Th1) responses underlie multiple sclerosis disease abrogation after hematopoietic stem cell transplantation. Ann Neurol. 2013;73:341–54.
De Kleer I, Vastert B, Klein M, Teklenburg G, Arkesteijn G, Yung GP, et al. Autologous stem cell transplantation for autoimmunity induces immunologic self-tolerance by reprogramming autoreactive T cells and restoring the CD4+CD25+immune regulatory network. Blood. 2006;107:1696–702.
Muraro PA, Douek DC. Renewing the T cell repertoire to arrest autoimmune aggression. Trends Immunol. 2006;27:61–67.
Arruda LCM, Clave E, Moins-Teisserenc H, Douay C, Farge D, Toubert A. Resetting the immune response after autologous hematopoietic stem cell transplantation for autoimmune diseases. Curr Res Transl Med. 2016;64:107–13.
MacIntyre A, Brouilette SW, Lamb K, Radhakrishnan K, McGlynn L, Chee MM, et al. Association of increased telomere lengths in limited scleroderma, with a lack of age-related telomere erosion. Ann Rheum Dis. 2008;67:1780–2.
Tarhan F, Vural F, Kosova B, Aksu K, Cogulu O, Keser G, et al. Telomerase activity in connective tissue diseases: elevated in rheumatoid arthritis, but markedly decreased in systemic sclerosis. Rheumatol Int. 2008;28:579–83.
Roelofs H, De Pauw ESD, Zwinderman AH, Opdam SM, Willemze R, Tanke HJ, et al. Homeostasis of telomere length rather than telomere shortening after allogeneic peripheral blood stem cell transplantation. Blood. 2003;101:358–62.
Monteiro J, Batliwalla F, Ostrer H, Gregersen PK. Shortened telomeres in clonally expanded CD28−CD8+T cells imply a replicative history that is distinct from their CD28+CD8+counterparts. J Immunol. 1996;156:3587–90.
Effros RB, Allsopp R, Chiu CP, Hausner MA, Hirji K, Wang L, et al. Shortened telomeres in the expanded CD28−CD8+cell subset in HIV disease implicate replicative senescence in HIV pathogenesis. AIDS. 1996;10:F17–22.
Vuddamalay Y, van Meerwijk JPM. CD28− and CD28lowCD8+regulatory T cells: of mice and men. Front Immunol. 2017;8:31.
Mollet L, Sadat-Sowti B, Duntze J, Leblond V, Bergeron F, Calvez V, et al. CD8hi+CD57+T lymphocytes are enriched in antigen-specific T cells capable of down-modulating cytotoxic activity. Int Immunol. 1998;10:311–23.
Autran B, Leblond V, Sadat-Sowti B, Lefranc E, Got P, Sutton L, et al. A soluble factor released by CD8+CD57+lymphocytes from bone marrow transplanted patients inhibits cell-mediated cytolysis. Blood. 1991;77:2237–41.
Mikulkova Z, Praksova P, Stourac P, Bednarik J, Strajtova L, Pacasova R, et al. Numerical defects in CD8+CD28− T-suppressor lymphocyte population in patients with type 1 diabetes mellitus and multiple sclerosis. Cell Immunol. 2010;262:75–9.
McKinney EF, Lee JC, Jayne DR, Lyons PA, Smith KG. T-cell exhaustion, co-stimulation and clinical outcome in autoimmunity and infection. Nature. 2015;523:612–6.
Wherry EJ. T cell exhaustion. Nat Immunol. 2011;12:492–9.
Thangavelu G, Parkman JC, Ewen CL, Uwiera RRE, Baldwin TA, Anderson CC. Programmed death-1 is required for systemic self-tolerance in newly generated T cells during the establishment of immune homeostasis. J Autoimmun. 2011;36:301–12.
Le Campion A, Gagnerault MC, Auffray C, Bécourt C, Poitrasson-Rivière M, Lallemand E, et al. Lymphopenia-induced spontaneous T-cell proliferation as a cofactor for autoimmune disease development. Blood. 2009;114:1784–93.
de Oliveira GLV, Malmegrim KCR, Ferreira AF, Tognon R, Kashima S, Couri CEB, et al. Up-regulation of fas and fasL pro-apoptotic genes expression in type 1 diabetes patients after autologous haematopoietic stem cell transplantation. Clin Exp Immunol. 2012;168:291–302.
de Oliveira GLV, Ferreira AF, Gasparotto EPL, Kashima S, Covas DT, Guerreiro CT, et al. Defective expression of apoptosis-related molecules in multiple sclerosis patients is normalized early after autologous haematopoietic stem cell transplantation. Clin Exp Immunol. 2017;187:383–98.
Larbi A, Fulop T. From ‘truly naïve’ to ‘exhausted senescent’ T cells: when markers predict functionality. Cytom Part A. 2014;85:25–35.
Acknowledgements
This work was supported by the financial research agencies CNPq, INSERM, and FAPESP (Scholarship numbers: 2013/18678-3, 2014/20922-2; Center for Cell-Based Therapy, CEPID-FAPESP, grant number 2013/08135-2).
Author contributions
MCO and KCRM are the principal investigators and take primary responsibility for the paper. LCMA, KCRM, AT, and MCO designed the study. LCMA, JRL-J, CD, IF, and EC performed the experiments. LCMA, JRL-J, DAM, BPS, and HM-T collected the data and performed data analysis. DTC provided essential funding to the development of this work. LCMA, KCRM, AT, EC, and MCO wrote the final report. All authors contributed to the editing of the final report. All authors agree on all of the content of the submitted manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
These authors share senior authorship: Kelen C. R. Malmegrim, Maria Carolina Oliveira.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Arruda, L.C.M., Lima-Júnior, J.R., Clave, E. et al. Homeostatic proliferation leads to telomere attrition and increased PD-1 expression after autologous hematopoietic SCT for systemic sclerosis. Bone Marrow Transplant 53, 1319–1327 (2018). https://doi.org/10.1038/s41409-018-0162-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-018-0162-0
This article is cited by
-
Tolerance regeneration by T regulatory cells in autologous haematopoietic stem cell transplantation for autoimmune diseases
Bone Marrow Transplantation (2020)
-
Autologe hämatopoetische Stammzelltransplantation bei Autoimmunerkrankungen
Zeitschrift für Rheumatologie (2020)