Abstract
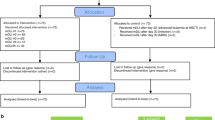
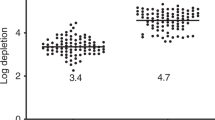
Recovery of immunity is delayed in recipients of T-depleted grafts. Adoptive transfer of memory T-cells may improve immune response to common pathogens. A cohort of 53 patients with malignant (n = 36) and non-malignant conditions (n = 17) received TCR alpha/beta depleted grafts from haploidentical (n = 25) or MUD (n = 28) donors. Donor lymphocytes were depleted of CD45RA-positive cells. At a median of 48 days after transplantation, patients received DLI at 25 × 103/kg CD3 cells from haploidentical or 100 × 103/kg CD3 from MUD donors. Up to 3 doses of donor lymphocytes were administered at monthly intervals, escalating to 100 × 103/kg in haploidentical transplants and 300 × 103/kg in MUD transplants. At a median follow-up of 23 months, the cumulative incidence of de novo acute GVHD after DLI is 2% (1 of 43), while the rate of reactivation of preexisting aGVHD was 50% (5 of 10). The transplant-related mortality is 6%. The overall survival rates are 80% and 88% in malignant and non-malignant conditions, respectively. Among patients with absent CMV-specific immune reactivity at baseline (n = 31) expansion of CMV-specific T-cells was demonstrated in 20 (64.5%) within 100 days. Infusions of low dose donor memory T-lymphocytes are safe and constitute a simple measure to prevent infections in the setting of alpha/beta T cell-depleted transplantation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chaleff S, Otto M, Barfield RC, Leimig T, Iyengar R, Martin J, et al. A large-scale method for the selective depletion of alphabeta T lymphocytes from PBSC for allogeneic transplantation. Cytotherapy. 2007;9:746–54. https://doi.org/10.1080/14653240701644000.
Handgretinger R. Negative depletion of CD3(+) and TcRalphabeta(+) T cells. Curr Opin Hematol. 2012;19:434–9. https://doi.org/10.1097/MOH.0b013e3283582340.
Schumm M, Lang P, Bethge W, Faul C, Feuchtinger T, Pfeiffer M, et al. Depletion of T-cell receptor alpha/beta and CD19 positive cells from apheresis products with the CliniMACS device. Cytotherapy. 2013;15:1253–8. https://doi.org/10.1016/j.jcyt.2013.05.014.
Bertaina A, Merli P, Rutella S, Pagliara D, Bernardo ME, Masetti R, et al. HLA-haploidentical stem cell transplantation after removal of alphabeta+ T and B cells in children with nonmalignant disorders. Blood. 2014;124:822–6. https://doi.org/10.1182/blood-2014-03-563817.
Balashov D, Shcherbina A, Maschan M, Trakhtman P, Skvortsova Y, Shelikhova L, et al. Single-center experience of unrelated and haploidentical stem cell transplantation with TCRalphabeta and CD19 depletion in children with primary immunodeficiency syndromes. Biol Blood Marrow Transplant. 2015;21:1955–62. https://doi.org/10.1016/j.bbmt.2015.07.008.
Maschan M, Shelikhova L, Ilushina M, Kurnikova E, Boyakova E, Balashov D, et al. TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia. Bone Marrow Transplant. 2016;51:668–74. https://doi.org/10.1038/bmt.2015.343.
Zvyagin IV, Mamedov IZ, Komech EA, Kurnikova EE, Boyakova EV, et al. Tracking T-cell immune reconstitution after TCRalphabeta/CD19-depleted hematopoietic cells transplantation in children. Leukemia. 2016;31:1145–53. https://doi.org/10.1038/leu.2016.321.
Laberko A, Bogoyavlenskaya A, Shelikhova L, Shekhovtsova Z, Balashov D, Voronin K, et al. Risk factors for and the clinical impact of cytomegalovirus and Epstein–Barr virus infections in pediatric recipients of TCR-alpha/beta- and CD19-depleted grafts. Biol Blood Marrow Transplant. 2016;23:489–90. https://doi.org/10.1016/j.bbmt.2016.12.635.
Heslop HE, Ng CY, Li C, Smith CA, Loftin SK, Krance RA, et al. Long-term restoration of immunity against Epstein–Barr virus infection by adoptive transfer of gene-modified virus-specific T lymphocytes. Nat Med. 1996;2:551–5.
Papadopoulou A, Gerdemann U, Katari UL, Tzannou I, Liu H, Martinez C, et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med. 2014;6:242ra283. https://doi.org/10.1126/scitranslmed.3008825.
Peggs KS, Verfuerth S, Pizzey A, Khan N, Guiver M, Moss PA, et al. Adoptive cellular therapy for early cytomegalovirus infection after allogeneic stem-cell transplantation with virus-specific T-cell lines. Lancet. 2003;362:1375–7. https://doi.org/10.1016/S0140-6736(03)14634-X.
Schmitt A, Tonn T, Busch DH, Grigoleit GU, Einsele H, Odendahl M, et al. Adoptive transfer and selective reconstitution of streptamer-selected cytomegalovirus-specific CD8+ T cells leads to virus clearance in patients after allogeneic peripheral blood stem cell transplantation. Transfusion. 2011;51:591–9. https://doi.org/10.1111/j.1537-2995.2010.02940.x.
Bleakley M, Heimfeld S, Loeb KR, Jones LA, Chaney C, Seropian S, et al. Outcomes of acute leukemia patients transplanted with naive T cell-depleted stem cell grafts. J Clin Invest. 2015;125:2677–89. https://doi.org/10.1172/JCI81229.
Shook DR, Triplett BM, Eldridge PW, Kang G, Srinivasan A, Leung W. Haploidentical stem cell transplantation augmented by CD45RA negative lymphocytes provides rapid engraftment and excellent tolerability. Pediatr Blood Cancer. 2015;62:666–73. https://doi.org/10.1002/pbc.25352.
Teschner D, Distler E, Wehler D, Frey M, Marandiuc D, Langeveld K, et al. Depletion of naive T cells using clinical grade magnetic CD45RA beads: a new approach for GVHD prophylaxis. Bone Marrow Transplant. 2014;49:138–44. https://doi.org/10.1038/bmt.2013.114.
Touzot F, Neven B, Dal-Cortivo L, Gabrion A, Moshous D, Cros G, et al. CD45RA depletion in HLA-mismatched allogeneic hematopoietic stem cell transplantation for primary combined immunodeficiency: a preliminary study. J Allergy Clin Immunol. 2015;135:1303–9. e1301-1303. https://doi.org/10.1016/j.jaci.2014.08.019.
Bleakley M, Heimfeld S, Jones LA, Turtle C, Krause D, Riddell SR, et al. Engineering human peripheral blood stem cell grafts that are depleted of naive T cells and retain functional pathogen-specific memory T cells. Biol Blood Marrow Transplant. 2014;20:705–16. https://doi.org/10.1016/j.bbmt.2014.01.032.
Brodszki N, Turkiewicz D, Toporski J, Truedsson L, Dykes J. Novel treatment of severe combined immunodeficiency utilizing ex-vivo T-cell depleted haploidentical hematopoietic stem cell transplantation and CD45RA+ depleted donor lymphocyte infusions. Orphanet J Rare Dis. 2016;11:5. https://doi.org/10.1186/s13023-016-0385-3.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Melenhorst JJ, Leen AM, Bollard CM, Quigley MF, Price DA, Rooney CM, et al. Allogeneic virus-specific T cells with HLA alloreactivity do not produce GVHD in human subjects. Blood. 2010;116:4700–2. https://doi.org/10.1182/blood-2010-06-289991.
Melenhorst JJ, Scheinberg P, Williams A, Ambrozak DR, Keyvanfar K, Smith M, et al. Alloreactivity across HLA barriers is mediated by both naive and antigen-experienced T cells. Biol Blood Marrow Transplant. 2011;17:800–9. https://doi.org/10.1016/j.bbmt.2010.12.711.
D’Orsogna LJ, Roelen DL, Doxiadis II, Claas FH. Alloreactivity from human viral specific memory T-cells. Transpl Immunol. 2010;23:149–55. https://doi.org/10.1016/j.trim.2010.06.008.
D’Orsogna LJ, van der Meer-Prins EM, Zoet YM, Roelen DL, Doxiadis II, Claas FH. Detection of allo-HLA cross-reactivity by virus-specific memory T-cell clones using single HLA-transfected K562 cells. Methods Mol Biol. 2012;882:339–49. https://doi.org/10.1007/978-1-61779-842-9_19.
Triplett BM, Shook DR, Eldridge P, Li Y, Kang G, Dallas M, et al. Rapid memory T-cell reconstitution recapitulating CD45RA-depleted haploidentical transplant graft content in patients with hematologic malignancies. Bone Marrow Transplant. 2015;50:968–77. https://doi.org/10.1038/bmt.2014.324.
Jain NA, Lu K, Ito S, Muranski P, Hourigan CS, Haggerty J, et al. The clinical and financial burden of pre-emptive management of cytomegalovirus disease after allogeneic stem cell transplantation-implications for preventative treatment approaches. Cytotherapy. 2014;16:927–33. https://doi.org/10.1016/j.jcyt.2014.02.010.
Acknowledgements
The authors thank the physicians and nursing staff of the Hematopoietic stem cell transplantation Units 1 and 2 for outstanding patient care, the staff of Molecular biology, Microbiology and Transplant biology laboratories for excellent service, Marina Persiantseva and Susanne Morsch for unrelated donor search, Dmitriy Pershin and Victoria Kiseleva for technical assistance. We are grateful to the “Podari Zhizn” foundation for continued support of the care of the patients and research in the field of hematopoietic stem cell transplantation.
Author contributions
MM planned the study, performed the analysis and wrote the manuscript. SB collected the data and wrote the manuscript. LS, AM, DB, and GN planned the study, analyzed the data and reviewed the manuscript. JS established the database. EK, YM, AK and PT performed graft and cell therapy product processing and formulation. EB, EO, NK and VZ performed immunomonitoring and cell therapy product quality control and contributed to the Methods section.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MM delivered lectures at Miltenyi Biotec satellite symposia at EBMT 2013 and EBMT 2016 annual meetings. Rest of the authors declare to have no conflict of interest.
Additional information
Ethics committee
The study was approved by Ethics committee of the Dmitriy Rogachev Federal Center of pediatric hematology, oncology and immunology.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Maschan, M., Blagov, S., Shelikhova, L. et al. Low-dose donor memory T-cell infusion after TCR alpha/beta depleted unrelated and haploidentical transplantation: results of a pilot trial. Bone Marrow Transplant 53, 264–273 (2018). https://doi.org/10.1038/s41409-017-0035-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-017-0035-y
This article is cited by
-
Automatic generation of alloreactivity-reduced donor lymphocytes and hematopoietic stem cells from the same mobilized apheresis product
Journal of Translational Medicine (2023)
-
A phase I/II dose-escalation multi-center study to evaluate the safety of infusion of natural killer cells or memory T cells as adoptive therapy in coronavirus pneumonia and/or lymphopenia: RELEASE study protocol
Trials (2021)
-
Improved survival and graft function in ex vivo T-cell depleted haploidentical hematopoietic cell transplantation for primary immunodeficiency
Bone Marrow Transplantation (2021)
-
T-cell tracking, safety, and effect of low-dose donor memory T-cell infusions after αβ T cell-depleted hematopoietic stem cell transplantation
Bone Marrow Transplantation (2021)
-
Selective T-cell depletion targeting CD45RA as a novel approach for HLA-mismatched hematopoietic stem cell transplantation in pediatric nonmalignant hematological diseases
International Journal of Hematology (2021)