Abstract
Phase 3 trials Viale-A and Viale-C evaluated health-related quality of life (HRQoL) in patients with AML unfit for intensive chemotherapy who received venetoclax (VEN) + (AZA) (Viale-A) or low-dose cytarabine (LDAC) (Viale-C) or placebo (PBO) + AZA or LDAC. Patient-reported outcomes included: EORTC QLQ-C30 global health status (GHS/QoL) and physical functioning (PF), PROMIS Cancer Fatigue Short Form 7a (Fatigue), and EQ-5D-5L health status visual analog scale (HS-VAS). Time to deterioration (TTD), defined as worsening from baseline in meaningful change thresholds (MCT) of ≥10, 5, or 7 points for GHS/QoL or PF, fatigue, and HS-VAS, respectively, was assessed; differences between groups were analyzed using Kaplan-Meier and unadjusted log-rank analyses. VEN + AZA vs PBO + AZA patients had longer TTD in GHS/QoL (P = 0.066) and fatigue (P = 0.189), and significantly longer TTD in PF (P = 0.028) and HS-VAS (P < 0.001). VEN + LDAC vs PBO + LDAC patients had significantly longer TTD in GHS/QoL (P = 0.011), PF (P = 0.020), and fatigue (P = 0.004), and a trend in HS-VAS (P = 0.057). Approximately 43%, 35%, 32%, and 18% of patients treated with VEN + AZA, AZA + PBO, VEN + LDAC, or LDAC + PBO, respectively, saw improvements >MCT in GHS/QoL. Overall, VEN may positively impact HRQoL in patients with AML ineligible for intensive chemotherapy, leading to longer preservation of functioning and overall health status.
Similar content being viewed by others
Introduction
Acute myeloid leukemia (AML) is an aggressive myeloid neoplasm that has a poor prognosis, with a reported 5-year overall survival rate estimated at 29% in recent historical series, and less than 10% in series of older adults [1]. The standard-of-care first-line treatment for patients with AML is intensive chemotherapy including cytarabine and an anthracycline [2]. Recent advances in intensive therapy include the use of midostaurin and gemtuzumab ozogamicin in association with induction chemotherapy in specific subsets of patients [3, 4]. Many patients in older age groups may not be eligible for intensive chemotherapy, however, due to factors such as age, comorbidities, or unfavorable genomic features [2, 5, 6]. Such patients often have poorer prognoses [7], and are commonly treated with less intensive regimens, which may include hypomethylating agents (ie, azacitidine or decitabine) and low-dose cytarabine (LDAC) [8,9,10,11,12]. The Food and Drug Administration (FDA) recently approved venetoclax in combination with azacitidine, decitabine, or LDAC for the treatment of newly diagnosed patients with AML who are ineligible for intensive chemotherapy, with these regimens representing new standards of care, due to improvements in response rates and overall survival [13, 14].
An important goal of treatment in all patients is to prolong health-related quality of life (HRQoL). Venetoclax in combination with azacitidine or LDAC for patients who are ineligible for intensive chemotherapy has been shown to be effective in increasing both complete remission rate and overall survival [15,16,17,18,19,20], and yet the impact of venetoclax as a combination therapy on the HRQoL of patients is not well known. Patients with AML have reduced QoL, including reductions in physical functioning (PF), increased fatigue, and decreased ability to maintain social and daily activities [21,22,23], with fatigue reported as the most burdensome symptom irrespective of treatment status [24]. At baseline, patients with AML who are ineligible for intensive chemotherapy had poor HRQoL scores, particularly in EORTC global health status (GHS) (median score of 50) and fatigue (median score of 53–66) on a 0–100 scale [25,26,27]. Furthermore, baseline impairments in role and physical domains, health status, and fatigue are lower than those observed in the general population, and QoL tends to deteriorate quickly at the time of diagnosis and treatment initiation [22, 24]. The impact of treatment on patient-reported outcomes (PROs) in patients with AML or other leukemias is increasingly appreciated as an important clinical outcome when treatment benefits are evaluated [24, 28], and thus can aid patients and providers in clinical decision making [29, 30].
Treatment of AML, even in unfit patients receiving less aggressive therapies, is associated with events that may negatively impact HRQoL including infection-related complications, high transfusion needs, and hospitalization [24]. The importance of capturing potential treatment benefits and outcomes from the patient perspective is further highlighted by an observed discordance between how patients and physicians perceive the patients’ HRQoL [31]. This study aimed to comprehensively characterize HRQoL outcomes of newly diagnosed patients with AML, and particularly potential delay in deterioration of HRQoL, for patients treated with venetoclax or placebo in the Viale-A and Viale-C clinical trials.
Materials and methods
Study design and patients
Full details on study design and eligibility criteria for the Viale-A (NCT02993523) and Viale-C (NCT03069352) Phase 3 clinical trials have been previously published [15, 18]. This secondary analysis utilized PRO data collected from these studies. Briefly, Viale-A and Viale-C are randomized, double-blind, placebo controlled, multicenter trials in patients ≥18 years of age with a confirmed diagnosis of untreated AML who were ineligible for intensive chemotherapy due to age or pre-defined comorbidities.
As previously described, patients in Viale-A were randomized 2:1 to receive venetoclax 400 mg orally once daily (QD) or placebo for 28 days, in combination with azacitidine 75 mg/m2 subcutaneous (SC) or intravenous (IV) for 7 days [15]. Patients in Viale-C were randomized 2:1 to receive venetoclax 600 mg orally QD or placebo for 28 days, in combination with LDAC 20 mg/m2 SC QD for 10 days [18]. Patients continued their assigned treatments in 28-day cycles, until documented disease progression per investigator assessment, unacceptable toxicity, withdrawal of consent, or other protocol criteria for discontinuation (whichever occurred first).
Ethics
For both trials, local ethics committee approvals were obtained, and patients included in the trials provided written informed consent. The studies were conducted in accordance with the International Conference on Harmonisation, Good Clinical Practice guidelines, and the Declaration of Helsinki.
Patient-reported outcomes
Patients with AML may experience deteriorations in HRQoL over time for multiple causes, including treatment-related complications or disease progression; this analysis assessed whether the addition of venetoclax to either azacitidine or LDAC would prolong the time to such deterioration. Several validated PRO instruments were utilized in the Viale-A and Viale-C trials to capture the patients’ experience regarding treatment benefits across various key HRQoL domains important to this patient population; instruments used included the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core [EORTC QLQ-C30] global health status (GHS/QoL) and PF scales, the Patient Reported Outcomes Measurement Information System, the Cancer Fatigue Short Form SF 7a (PROMIS Fatigue SF 7A), and the EuroQoL 5 Dimension 5 level (EQ-5D-5L) visual analog scale (health status VAS) [32,33,34,35,36].
The EORTC QLQ-C30 comprises 30 items addressing 15 HRQoL domains, including five multi-item functional scales (physical, emotional, cognitive, social, and role functioning), three multi-item symptom scales (fatigue, nausea and vomiting, and pain), six single-item symptom scales (dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial difficulties) and a GHS/QoL scale. All scales are scored on a 0–100 metric. For GHS/QoL and functional scales, a high score represents higher/better level of functioning and for symptom scales a higher score indicates worse symptom severity. The recall period for EORTC QLQ-C30 is the past week. The PROMIS Fatigue SF 7a or fatigue has been developed for use in oncology and other chronic disease populations [33] and consists of a seven-item questionnaire assessing the impact and experience of fatigue over the past 7 days with higher scores representing worse fatigue. The EQ-5D-5L VAS or health status VAS, which measures current overall health status, is scored on a scale of 0–100 where 100 represents “the best health you can imagine,” and 0 indicates “the worst health you can imagine.”
All PRO questionnaires were collected on Cycle 1 Day 1, and then on Day 1 of every other cycle throughout both trials, including the final visit. The primary outcome of this analysis was to compare the delay in time to deterioration for each PRO measure, for patients randomized to venetoclax in combination with azacitidine or LDAC to those treated with azacitidine or LDAC. Deterioration in HRQoL was defined as the worsening from baseline in PRO-specific meaningful change thresholds (MCTs). Time to deterioration was assessed overall and for patients in key subgroups. Subgroups analyzed included patients with complete remission + complete remission and incomplete blood cell recovery (CR + CRi), ages <75 or ≥75 years, defined by postbaseline transfusion independence (TI) status (RBC or platelets), or with baseline ECOG score >2. An additional analysis was conducted to compare the proportions of patients in each treatment group who reported improvements from baseline in at least one MCT for each PRO measure. MCTs were defined based upon published thresholds of change of ≥10, and 7 points for GHS/QoL and PF [37], and health status VAS [38], respectively. In this study, MCT was defined as a change of ≥5 points for fatigue.
Statistical analysis
Time to deterioration was summarized as the median and 95% confidence interval (CI) for each treatment group. Kaplan-Meier curves were calculated, as well as the unadjusted log-rank P-value for the difference between treatment arms. Cox proportional hazards regression models adjusted for key covariates (age, baseline Eastern Cooperative Oncology Group and PRO scores, AML type, and cytogenetic risk category); hazard ratios (HR) and their corresponding 95% CIs comparing the treatment groups are reported. The proportion of patients who reported improvements ≥ MCTs for a specified PRO at any point post-baseline was reported as numbers and percentages. Improvement in HRQoL was defined as an improvement in score from baseline of at least one PRO-specific MCT at any time. Improvements in HRQoL were assessed overall and for patients who achieved CR + CRi.
Time to deterioration was calculated as the number of days from baseline to the date of the first observed deterioration event, defined as a decline from baseline score of at least one MCT for each PRO at a post-baseline assessment among patients with available data on the PRO measure at baseline. Patients without a baseline PRO measure were excluded from analysis. Deterioration events were based on the change from the baseline score only; therefore, any deterioration of PRO scores between follow-up visits (i.e, improvement and then worsening) was not captured in this analysis even if this decline was ≥1 MCT between visits. If a specified deterioration event did not occur, patients were censored at the last observed post-baseline PRO assessment. If the post-baseline PRO measure was not available, then the patient was censored a day after the baseline PRO assessment date (censored at baseline + 1 day). Analyses were based upon the longitudinal analysis population, comprising all patients in the full analysis dataset (intention-to-treat population) who survived up to a given assessment and had available data on at least one PRO measure at baseline and for that assessment. The number of patients available for analysis is reflected in the Kaplan Meier plots as the N number of patients at risk at month 0.
Sensitivity analysis
A sensitivity analysis was utilized to assess time to deterioration from baseline PRO assessment to a composite endpoint of progressive disease, death, or symptom worsening, defined as a change in score of at least one MCT in a relevant PRO measure. Deterioration was determined by the first occurrence of any one of these events and if none of the specified events occurred, or if patients did not have any post-baseline PRO assessments, their data were censored at the last observed disease assessment date (same censoring date for event-free survival). Patients without a baseline PRO assessment were excluded from the sensitivity analysis.
Results
Baseline demographics and clinical characteristics
Viale-A included 431 pts (venetoclax + azacitidine: 286, placebo + azacitidine: 145) and Viale-C included 211 pts (venetoclax + LDAC: 143, placebo + LDAC: 68). In both studies and in all treatment groups, the median age was 76 years and nearly 60% patients were male. In Viale-A, secondary AML has reported in 25% and 24% and poor cytogenetic risk in 36% and 39% of patients in the venetoclax + azacitidine and placebo + azacitidine groups, respectively. In Viale-C, secondary AML was reported in 41% and 34% and poor cytogenetic risk in 29% and 33% of patients in the venetoclax + LDAC and placebo + LDAC groups, respectively (Supplemental Table 1).
Viale-A time to deterioration in HRQoL
Compared with placebo + azacitidine patients, venetoclax + azacitidine patients showed a trend towards longer time to deterioration in GHS/QoL (median in months: 16.5 vs. 9.3, P = 0.066) and fatigue (9.3 vs. 8.6, P = 0.189) (Fig. 1; Table 1). Venetoclax + azacitidine patients had a significantly longer time to deterioration in PF (9.7 vs. 6.2, P = 0.028) and health status VAS (10.7 vs. 3.9, P < 0.001) than did patients treated with placebo + azacitidine (Fig. 1; Table 1).
Time to deterioration in EORTC GHS/QoL (A), PROMIS Fatigue (B), EORTC PF (C), and Health Status (EQ-5D-5L) VAS (D), VEN + AZA versus PBO + AZA. Time to deterioration thresholds for EORTC-QLQ-C30, EQ-5D-5L VAS, and PROMIS Fatigue are ≥10, 7, or 5 points, respectively. Time to deterioration analyses were conducted for all patients in the full dataset with available data on ≥1 PRO measures from baseline to the given assessment (N = VEN + AZA 262, 264, 262, and 260, and PBO + AZA 130, 132, 130, and 130 for EORTC GHS/QoL, fatigue, PF, and health status VAS, respectively). AZA azacitidine, CI confidence interval, EORTC QLQ-C30 European Organization for Research and Treatment of Cancer quality of life questionnaire, EQ-5D-5L EuroQoL 5-Dimension 5-Level, GHS global health status, NE not estimable, PBO placebo, PF physical functioning, PROMIS Patient-Reported Outcomes Measurement Information System, QoL quality of life, VAS visual analog scale, VEN venetoclax.
Viale-C time to deterioration in HRQoL
Compared with those in the placebo + LDAC group, venetoclax + LDAC patients experienced a significantly longer time to deterioration in GHS/QoL (11.3 vs. 2.6, P = 0.011), PF (5.8 vs. 2.9, P = 0.020), and fatigue (8.1 vs. 2.6, P = 0.004), and a trend towards longer time to deterioration in health status VAS (4.9 vs. 2.5, P = 0.057) (Fig. 2; Table 1).
Time to deterioration in EORTC GHS/QoL (A), PROMIS Fatigue (B), EORTC PF (C), and Health Status (EQ-5D-5L) VAS (D), VEN + LDAC versus PBO + LDAC. Time to deterioration thresholds for EORTC-QLQ-C30, EQ-5D-5L VAS, and PROMIS Fatigue are ≥10, 7, or 5 points, respectively. Time to deterioration analyses were conducted for all patients in the full dataset with available data on ≥1 PRO measures from baseline to the given assessment (N = VEN + LDAC: 127, 127, 127, and 127; and PBO + LDAC: 59, 60, 59, and 59 for EORTC GHS/QoL, fatigue, PF, and health status VAS, respectively). CI confidence interval, EORTC QLQ-C30 European Organization for Research and Treatment of Cancer quality of life questionnaire, EQ-5D-5L EuroQoL 5-Dimension 5-Level, GHS global health status, LDAC low-dose cytarabine, NE not estimable, PBO placebo, PF physical functioning, PROMIS Patient-Reported Outcomes Measurement Information System, QoL quality of life, VAS visual analog scale, VEN venetoclax.
Cox regression model
Cox proportional hazards models demonstrated consistently longer time to deterioration in all PRO-assessed measures for patients treated with venetoclax as compared with placebo in both trials, with significant differences for PF and health status VAS in Viale-A, and for all measures in Viale-C (P ≤ 0.01) (Table 1).
Subgroup analyses
There was a trend towards longer time to deterioration in the venetoclax + azacitidine group versus the placebo + azacitidine group for all subgroups for GHS/QoL and in health status VAS for the CR + CRi subgroup (Supplemental Fig. 1–6). Similar results were observed in the Viale-C trial for all subgroups except for CR + Cri, where the sample size of patients attaining CR + CRi was too small in the control patient population to allow robust between treatment group statistical analysis. There was a trend towards longer time to deterioration in GHS/QoL observed in venetoclax treated patients in the subgroup of patients <75 years of age, which was significant in patients treated in Viale-A (Table 2); notably, in patients >75 years of age, there was a similar time to deterioration between the treatment groups.
Percent improvements in HRQoL
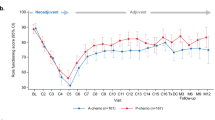
Across all PROs, numerically greater proportions of patients treated with venetoclax + azacitidine or LDAC versus placebo + azacitidine or LDAC reported improvements at any time post-baseline (Table 3). Specifically, 43% versus 35% of patients treated with venetoclax + azacitidine versus placebo + azacitidine and 32% versus 18% of patients treated with venetoclax + LDAC versus placebo + LDAC reported improvements in GHS/QoL. Compared with placebo + azacitidine, greater proportions of patients treated with venetoclax + azacitidine reported improvements in PF (29% vs. 26%), fatigue (39% vs. 32%), and health status VAS (43% vs. 27%). Compared with placebo + LDAC, greater proportions of patients treated with venetoclax + LDAC reported improvements in PF (32% vs. 16%), fatigue (38% vs. 18%), and health status VAS (33% vs. 22%). Of the total patients who reported improvements, ≥65% reported improvements by cycle 4 for all PROs regardless of treatment group.
Similar findings were observed among patients who achieved CR + CRi (Table 3). Additionally, greater proportions of patients achieving versus not achieving CR + CRi reported improvements across all PROs among patients who received venetoclax in combination with azacitidine or LDAC.
Sensitivity analyses
The sensitivity analyses demonstrated that in both Viale-A and Viale-C, the median time to deterioration was significantly longer for patients in the venetoclax + azacitidine or LDAC treatment groups for all instruments and subscales trials (Supplemental Figures 7, 8) than it was for patients receiving placebo + azacitidine or LDAC. However, the inclusion of progression and death in the definition of deterioration contributed to shorter median times to deterioration for all treatment groups in both studies.
Discussion
Understanding HRQoL from the patient perspective is important in evaluating treatment efficacy, particularly for oncology patients for whom survival may be limited and quality of life during the remaining lifespan is of primary importance to patients, and thus is crucial in treatment decision making, in addition to more standard response-based endpoints [39]. Our study is one of the few to assess longitudinal changes in HRQoL in patients with AML ineligible for intensive chemotherapy within a clinical trial population [10, 26, 40,41,42]. In our study, significantly longer time to deterioration for patients receiving combination venetoclax compared with placebo + azacitidine or LDAC was observed for all PRO measures, including general QoL and health status, PF, and fatigue in Viale-C, and for PF and health status VAS scores in Viale-A. Interestingly, in Viale-A, the time to deterioration in fatigue was similar in both treatment groups, compared with Viale-C, where patients in the venetoclax + LDAC group experienced a significantly longer time to deterioration compared with the placebo + LDAC group. One interpretation could be that azacitidine may cause treatment-related fatigue that is not ameliorated in these patients. Furthermore, numerically greater proportions of patients receiving combination venetoclax compared with placebo + azacitidine or LDAC reported improvements in GHS/QoL and health status VAS in Viale-A, and GHS/QoL and fatigue in Viale-C. Although the venetoclax combination groups represent a more intensive combination therapy, in this study there was no increased worsening of HRQoL among patients treated with venetoclax + azacitidine or LDAC compared to azacitidine or LDAC alone.
While the effects of non-intensive chemotherapy-based AML therapies on clinical endpoints such as overall survival and relapse-free survival are known [12], their effects on HRQoL remain largely undefined [26]. Key aspects of patient HRQoL impacted by AML include fatigue, PF, anxiety/mental health, and ability to maintain social and role functioning [21, 23]. Patient characteristics may influence HRQoL and treatment-related outcomes, especially among older patients. However, data regarding HRQoL in such patients are limited, and more studies are needed that not only incorporate PROs in older patients, but also track changes in their symptoms and functioning over time [43]. In the current study, patients treated with venetoclax experienced significantly longer time to deterioration compared with those in the placebo group in several HRQoL domains, including overall health status/QoL, PF, and fatigue. These results were largely confirmed in the sensitivity analyses that expanded the definition to include progression, death, and relapse following remission. In this composite analysis, significantly longer time to deterioration was observed in both venetoclax combination groups versus the placebo + azacitidine or LDAC groups across all HRQoL measures, although the inclusion of progression and death in the definition of deterioration contributed to shorter median time to deterioration for all treatment groups in both studies. Overall, the addition of venetoclax trended towards a longer preservation of HRQoL across various measures. In addition to preservation of HRQoL, there were greater proportions of patients reporting improvements in PRO measures of at least one MCT in both venetoclax combination groups versus the placebo + azacitidine or LDAC groups across all HRQoL measures. In a previous analysis, by cycle 2 the percent change from baseline in EORTC QLQ 30 GHS/QoL went up by approximately 30% among patients treated with decitabine versus best supportive care; this change was carried through cycle 4 [44]. Furthermore, in a previously published study, the mean change from baseline in EORTC QLQ 30 GHS/QoL and fatigue scores demonstrated improvements by cycle 3 that were sustained by cycle 9 among patients who received venetoclax + LDAC [18]. Similarly in our study, most patients who reported any improvements in measures of HRQoL from baseline reported them by cycle 4. That HRQoL is not worsened by the addition of venetoclax to a less aggressive strategy such as azacitidine or LDAC alone, may be an added value of combination therapy from the patients’ perspective in treatment decision making, which is further supported by the greater proportions of patients receiving venetoclax combinations versus azacitidine or LDAC alone reporting improvements in HRQoL.
While subgroup analyses were often limited by small sample sizes, which impact the statistical robustness of the results, especially in the control groups and also for later study visits, a subgroup analysis demonstrated consistent prolongation of time to deterioration in the venetoclax combination groups versus placebo groups across various subsets of patients. In the previous clinical efficacy reports, more patients achieved CR/CRi with venetoclax combination treatment compared with the placebo treatment groups [15, 18]. Among patients who were clinical responders (CR + CRi) in the current study, a trend towards longer time to deterioration in GHS/QoL and health status VAS was observed in the venetoclax + azacitidine versus placebo + azacitidine groups in Viale-A. The median time to deterioration was 16.5 months overall and 21.3 months in the CR + CRi subgroup in the venetoclax + azacitidine treatment group. These findings support the longer duration of CR + CRi clinical response observed in the venetoclax + azacitidine (17.5 months) versus placebo + azacitidine (13.4 months) groups in Viale-A [15]. Furthermore, the proportions of patients who reported improvements in HRQoL at any time was numerically higher across all PROs among those who achieved remission versus those who did not in the venetoclax combination arms. These analyses demonstrated that patients achieving remission/response had a similar QoL, suggesting that their HRQoL overall was not compromised by the addition of venetoclax. Previous studies have shown that achievement and durability of remission are factors that may have a role in the extent to which improvements are observed among patients with AML [45, 46]. In Viale-C, distinct separation of KM curves demonstrate a trend of longer time to deterioration in GHS/QoL with the addition of venetoclax versus LDAC alone among patients with post-baseline TI (RBC and platelet); similar results were observed in Viale-A among patients with post-baseline platelet TI. This demonstrates the potential durability of the TI response, which is an indirect measure of QoL as patients may see the reduction in need for transfusions and reduced anemia symptoms as an improvement in their HRQoL. Among patients with baseline ECOG scores >2, there was a trend of longer time to deterioration in general QoL in both venetoclax combination arms versus placebo + azacitidine or LDAC. In younger patients (<75 years) treated with combination venetoclax versus azacitidine, there was a significantly longer time to deterioration in general QoL. In contrast, the time to deterioration was similar between treatment groups in older patients (≥75 years) with a slight trend towards prolongation of HRQoL with venetoclax combination therapy; this finding is important as elderly patients tend to have worse clinical outcomes and HRQoL [7, 43]. A longitudinal study among individuals with AML > 60 years found that QoL improved but remained on similar trajectories with no significant difference in QoL measures observed between those who received intensive or non-intensive treatments, suggesting that similar improvements and/or stability of QoL may be expected regardless of treatment type among older patients [47]. Future studies analyzing the HRQoL during treatment among individuals >75 may be useful to identify areas where combination therapy may impact their HRQoL as part of the treatment plan.
Although the PROs used in this study are validated and commonly used in oncology, there are some limitations to their use [34, 37, 38]. For example, EORTC QLQ-C30 GHS/QoL and EQ-5D-5L health status VAS are generic health measurements not specific to AML. The EORTC QLQ-C30 has been used extensively across multiple types of cancer and has supported labeling claims in the US and Europe [32, 48,49,50]. Despite this limitation, the PRO measures utilized in this study do contain key aspects that overlap with key domains of HRQoL that were identified as important to patients with AML including fatigue, PF, anxiety, and reductions in the ability to maintain social functioning [21, 23, 51]. However, the lack of distinct separation between the treatment groups observed in this study may suggest that AML-specific measures may be better reflective of the HRQoL of these patients. AML-specific QoL measures are in development and their use in future clinical trials may identify the most appropriate outcomes to measure, leading to a better understanding of the impact of the disease and treatment on patients with AML [51, 52].
One other limitation to the reporting of these data in leukemia is that the primary analysis did not assess improvement of HRQoL from baseline. While the time to deterioration curves did not directly capture improvements, patients who maintained their HRQoL or improved are reflected here indirectly by a longer time to deterioration.
One of the challenges of the PROMIS Fatigue PRO is that patients in all treatment groups in this study received a drug with fatigue as a known side effect. In the Viale-A and Viale-C primary studies, 17–21% and <20% of patients experienced fatigue as an adverse event, respectively [15, 18]. Fatigue is considered a highly burdensome symptom among patients with AML [24], therefore, determining the relevance of PROMIS Fatigue data as compared with adverse event reporting of fatigue is important to address the challenge of separating treatment-related versus disease-related fatigue. PROMIS Fatigue data may be more relevant as the data are patient-reported, providing patients with the opportunity to report their perceived burden of fatigue on their daily activities.
Another limitation is the small sample size beyond the early treatment cycles; however, the early separation of the time to deterioration curves with the initial larger sample size suggests that these results are not due to chance variability and are statistically valid. The small sample sizes in the subgroup analyses limited the interpretation of those results.
In summary, compared with standard chemotherapy alone, venetoclax appears to have a positive impact on the HRQoL, or at least did not significantly worsen it, in patients with AML who are ineligible for intensive chemotherapy, leading to a longer preservation of functioning and overall health status. Between 29% and 43% of patients treated with venetoclax combination therapy saw improvements in their HRQoL, most of these patients reported better scores in their overall health status, physical function, and fatigue by cycle 4. Understanding treatment efficacy from the patient perspective may influence treatment decisions and allow for identification of specific aspects of HRQoL impacted by AML for which strategies may be developed to provide relief. Future studies may utilize AML-specific measurements to further quantify the impact of treatment with venetoclax on PROs.
Supplementary information is available at Blood Cancer Journal’s website.
Data availability
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research, and will be provided following review and approval of a research proposal and Statistical Analysis Plan (SAP)and execution of a Data Sharing Agreement (DSA). Data requests can be submitted at any time and the data will be accessible for12 months, with possible extensions considered. For more information on the process, or to submit a request, visit the following link: https://www.abbvie.com/our-science/clinical-trials/clinical-trials-data-and-information-sharing/data-and-information-sharing-with-qualified-researchers.html.
References
Howlader N, Noone A, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, based on November 2019 SEER data submission, posted to the SEER website, April 2020 [Available from: https://seer.cancer.gov/archive/csr/1975_2017/.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017;129:424–47.
Levis M. Midostaurin approved for FLT3-mutated AML. Blood 2017;129:3403–06.
Yu B, Liu D. Gemtuzumab ozogamicin and novel antibody-drug conjugates in clinical trials for acute myeloid leukemia. Biomark Res. 2019;7:24.
Ossenkoppele G, Löwenberg B. How I treat the older patient with acute myeloid leukemia. Blood 2015;125:767–74.
Song X, Peng Y, Wang X, Chen Y, Jin L, Yang T, et al. Incidence, survival, and risk factors for adults with acute myeloid leukemia not otherwise specified and acute myeloid leukemia with recurrent genetic abnormalities: analysis of the surveillance, epidemiology, and end results (SEER) database, 2001–2013. Acta Haematologica. 2018;139:115–27.
Thein MS, Ershler WB, Jemal A, Yates JW, Baer MR. Outcome of older patients with acute myeloid leukemia: an analysis of SEER data over 3 decades. Cancer 2013;119:2720–7.
Amadori S, Suciu S, Selleslag D, Aversa F, Gaidano G, Musso M, et al. Gemtuzumab ozogamicin versus best supportive care in older patients with newly diagnosed acute myeloid leukemia unsuitable for intensive chemotherapy: results of the randomized phase III EORTC-GIMEMA AML-19 Trial. J Clin Oncol. 2016;34:972–9.
Burnett AK, Milligan D, Prentice AG, Goldstone AH, McMullin MF, Hills RK, et al. A comparison of low-dose cytarabine and hydroxyurea with or without all-trans retinoic acid for acute myeloid leukemia and high-risk myelodysplastic syndrome in patients not considered fit for intensive treatment. Cancer 2007;109:1114–24.
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH, et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood 2015;126:291–99.
Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J, et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol. 2012;30:2670–7.
Stein EM, DiNardo CD, Pollyea DA, Schuh AC. Response kinetics and clinical benefits of nonintensive AML therapies in the absence of morphologic response. Clin Lymphoma Myeloma Leuk. 2020;20:e66–e75.
AbbVie. VENCLEXTA [Prescribing information] Available from: https://www.rxabbvie.com/pdf/venclexta.pdf.
US Food Drug Administration. FDA approves venetoclax in combination for AML in adults [Available from: https://www.fda.gov/drugs/fda-approves-venetoclax-combination-aml-adults.
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N. Engl J Med. 2020;383:617–29.
DiNardo CD, Pratz K, Pullarkat V, Jonas BA, Arellano M, Becker PS, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 2019;133:7–17.
Richard-Carpentier G, DiNardo CD. Venetoclax for the treatment of newly diagnosed acute myeloid leukemia in patients who are ineligible for intensive chemotherapy. Ther Adv Hematol. 2019;10:2040620719882822.
Wei AH, Montesinos P, Ivanov V, DiNardo CD, Novak J, Laribi K, et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood 2020;135:2137–45.
Wei AH, Strickland SA Jr., Hou JZ, Fiedler W, Lin TL, Walter RB, et al. Venetoclax combined with low-dose cytarabine for previously untreated patients with acute myeloid leukemia: Results from a phase Ib/II study. J Clin Oncol. 2019;37:1277–84.
Winters AC, Gutman JA, Purev E, Nakic M, Tobin J, Chase S, et al. Real-world experience of venetoclax with azacitidine for untreated patients with acute myeloid leukemia. Blood Adv. 2019;3:2911–19.
Buckley SA, Jimenez-Sahagun D, Othus M, Walter RB, Lee SJ. Quality of life from the perspective of the patient with acute myeloid leukemia. Cancer 2018;124:145–52.
Mamolo CM, Cappelleri JC, Hoang CJ, Kim R, Hadfield A, Middleton C, et al. A real-world, cross-sectional, community survey of symptoms and health-related quality of life of adults with acute myeloid leukemia. Future Oncol. 2019;15:1895–909.
Tomaszewski EL, Fickley CE, Maddux L, Krupnick R, Bahceci E, Paty J, et al. The patient perspective on living with acute myeloid leukemia. Oncol Ther. 2016;4:225–38.
Korol EE, Wang S, Johnston K, Ravandi-Kashani F, Levis M, van Nooten F. Health-related quality of life of patients with acute myeloid leukemia: a systematic literature review. Oncol Ther. 2017;5:1–16.
Deschler B, Ihorst G, Platzbecker U, Germing U, März E, de Figuerido M, et al. Parameters detected by geriatric and quality of life assessment in 195 older patients with myelodysplastic syndromes and acute myeloid leukemia are highly predictive for outcome. Haematologica 2013;98:208–16.
Forsythe A, Kwon CS, Bell T, Smith TA, Arondekar B. Health-related quality of life in acute myeloid leukemia patients not eligible for intensive chemotherapy: results of a systematic literature review. Clinicoecon Outcomes Res. 2019;11:87–98.
Oliva EN, Nobile F, Alimena G, Ronco F, Specchia G, Impera S, et al. Quality of life in elderly patients with acute myeloid leukemia: patients may be more accurate than physicians. Haematologica 2011;96:696–702.
Stauder R, Lambert J, Desruol-Allardin S, Savre I, Gaugler L, Stojkov I, et al. Patient-reported outcome measures in studies of myelodysplastic syndromes and acute myeloid leukemia: Literature review and landscape analysis. Eur J Haematol. 2020;104:476–87.
Efficace F, Kemmler G, Vignetti M, Mandelli F, Molica S, Holzner B. Health-related quality of life assessment and reported outcomes in leukaemia randomised controlled trials–a systematic review to evaluate the added value in supporting clinical decision making. Eur J Cancer. 2008;44:1497–506.
Cannella L, Caocci G, Jacobs M, Vignetti M, Mandelli F, Efficace F. Health-related quality of life and symptom assessment in randomized controlled trials of patients with leukemia and myelodysplastic syndromes: what have we learned? Crit Rev Oncol Hematol. 2015;96:542–54.
Horvath Walsh LE, Rider A, Piercy J, Pike J, Wilson S, Pandya BJ, et al. Real-world impact of physician and patient discordance on health-related quality of life in US patients with acute myeloid leukemia. Oncol Ther. 2019;7:67–81.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Cella D, Lai JS, Jensen SE, Christodoulou C, Junghaenel DU, Reeve BB, et al. PROMIS fatigue item bank had clinical validity across diverse chronic conditions. J Clin Epidemiol. 2016;73:128–34.
Garcia SF, Cella D, Clauser SB, Flynn KE, Lad T, Lai JS, et al. Standardizing patient-reported outcomes assessment in cancer clinical trials: a patient-reported outcomes measurement information system initiative. J Clin Oncol. 2007;25:5106–12.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Oppe M, Devlin NJ, van Hout B, Krabbe PF, de Charro F. A program of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value Health. 2014;17:445–53.
Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16:139–44.
Pickard AS, Neary MP, Cella D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes. 2007;5:70.
Sekeres MA, Stone RM, Zahrieh D, Neuberg D, Morrison V, De Angelo DJ, et al. Decision-making and quality of life in older adults with acute myeloid leukemia or advanced myelodysplastic syndrome. Leukemia 2004;18:809–16.
Sekeres MA, Lancet JE, Wood BL, Grove LE, Sandalic L, Sievers EL, et al. Randomized phase IIb study of low-dose cytarabine and lintuzumab versus low-dose cytarabine and placebo in older adults with untreated acute myeloid leukemia. Haematologica 2013;98:119–28.
Kornblith AB, Herndon JE 2nd, Silverman LR, Demakos EP, Odchimar-Reissig R, Holland JF, et al. Impact of azacytidine on the quality of life of patients with myelodysplastic syndrome treated in a randomized phase III trial: a Cancer and Leukemia Group B study. J Clin Oncol. 2002;20:2441–52.
Lübbert M, Suciu S, Baila L, Rüter BH, Platzbecker U, Giagounidis A, et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol. 2011;29:1987–96.
Storey S, Gray TF, Bryant AL. Comorbidity, physical function, and quality of life in older adults with acute myeloid leukemia. Curr Geriatr Rep. 2017;6:247–54.
Kantarjian H, Issa J-PJ, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, et al. Decitabine improves patient outcomes in myelodysplastic syndromes. Cancer 2006;106:1794–803.
Buckley SA, Kirtane K, Walter RB, Lee SJ, Lyman GH. Patient-reported outcomes in acute myeloid leukemia: where are we now? Blood Rev. 2018;32:81–87.
Kayastha N, Wolf SP, Locke SC, Samsa GP, El-Jawahri A, LeBlanc TW. The impact of remission status on patients’ experiences with acute myeloid leukemia (AML): an exploratory analysis of longitudinal patient-reported outcomes data. Support Care Cancer. 2018;26:1437–45.
El-Jawahri A, Abel GA, Traeger L, Waldman L, Markovitz N, VanDusen H, et al. Quality of life and mood of older patients with acute myeloid leukemia (AML) receiving intensive and non-intensive chemotherapy. Leukemia 2019;33:2393–402.
Gnanasakthy A, Mordin M, Clark M, DeMuro C, Fehnel S, Copley-Merriman C. A review of patient-reported outcome labels in the United States: 2006 to 2010. Value Health 2012;15:437–42.
DeMuro C, Clark M, Doward L, Evans E, Mordin M, Gnanasakthy A. Assessment of PRO label claims granted by the FDA as compared to the EMA (2006–2010). Value Health. 2013;16:1150–55.
Velikova G, Coens C, Efficace F, Greimel E, Groenvold M, Johnson C, et al. Health-related quality of life in EORTC clinical trials—30 years of progress from methodological developments to making a real impact on oncology practice. Eur J Cancer. 2012;10:141–49.
Buckley SA, Halpern AB, Othus M, Jimenez-Sahagun D, Walter RB, Lee SJ. Development and validation of the AML-QOL: a quality of life instrument for patients with acute myeloid leukemia. Leuk Lymphoma. 2020;61:1158–67.
Salas M, Henderson M, Wientzek-Fleischmann A, Islam Z, Tu N, Bilitou A, et al. Validated instruments of quality of life (QOL) in patients with acute myeloid leukemia (AML) and other cancers. Front Pharm. 2020;11:1109.
Funding
Venetoclax is being developed in a collaboration between AbbVie and Genentech. AbbVie and Genentech funded NCT02993523 and AbbVie funded NCT03069352 and participated in the given study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the publication. All authors had access to relevant data and participated in the drafting, review, and approval of this article. No honoraria or payments were made for authorship. The authors, AbbVie, and Genentech would like to thank the patients, their families, and caregivers, as well as the study investigators, research, and supporting staff. Medical writing support was provided by Brandy Menges, PhD, of Fishawack Facilitate Ltd (part of Fishawack Health; Conshohocken, PA) and funded by AbbVie.
Author information
Authors and Affiliations
Contributions
All authors had access to the data and participated in data collection and interpretation; initial analysis was performed by RK, CNB, and KB, with all other authors contributing thereafter. All authors contributed to the manuscript development and revisions and gave final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
KWP: grant support and advisory board fees from AbbVie, Astellas, Agios, Bristol Myers Squibb, Celgene, Daiichi Sankyo, Jazz Pharmaceuticals, Servier, and Millennium; grant support from Astellas, Boston BioMedical, Celgene, Jazz Pharmaceuticals. PP: grant and research support from AbbVie, Roche, Novartis, and Genesis; honoraria from AbbVie, Janssen, Roche, Novartis, Gilead, and GCR: Research grants from Abbvie, Amgen, Novartis, Celgene, Jazz Pharmaceuticals, Agios, Chugai, MaatPharma, Astellas, Iqvia, Roche and DS; an advisory role for Abbvie, Janssen, Jazz Pharmaceuticals, Novartis, Celgene, Otsuka, Astellas, Daiichi-Sankyo, Macrogenics, Roche, Takeda, and Pfizer. BAJ: consultant/advisory role for AbbVie, BMS, Genentech, Gilead, GlycoMimetics, Jazz, Pfizer, Servier, Takeda, Tolero, and Treadwell; protocol steering committee for GlycoMimetics; data monitoring committee for Gilead; travel reimbursement from AbbVie; research funding to his institution from 47, AbbVie, Accelerated Medical Diagnostics, Amgen, AROG, BMS, Celgene, Daiichi Sankyo, F. Hoffmann-La Roche, Forma, Genentech/Roche, Gilead, GlycoMimetics, Hanmi, Immune-Onc, Incyte, Jazz, Loxo, LP Therapeutics, Pfizer, Pharmacyclics, Sigma Tau, and Treadwell. PM: advisor/speaker/research support from AbbVie, Janssen, Novartis, Pfizer, and Teva; advisor/speaker/consultant/research support for Astellas, Celgene, and Daiichi-Sankyo; consultant for Agios, Tolero Pharmaceuticals, Glycomimetics, and Forma Therapeutics; advisor/speaker for Incyte and Sanofi; advisor/research support for Karyopharm. ACS: received research funding from AbbVie, Agios, Amgen, BMS/Celgene, Glycomimetics, Pfizer, and Novartis; advisory board member for AbbVie, Agios, Amgen, Astellas, BMS/Celgene, Taiho, and Teva. CD: received research funding from AbbVie/Genentech, Agios, Celgene, Daiichi Sankyo, Millennium, and Novartis and served as consultant for Agios; advisory board member for AbbVie, Agios, Bayer, Celgene, Karyopharm, and Medimmune. JN: consultant/advisor for Novartis, Roche, Pfizer, Amgen, Takeda, and Astellas; received travel expenses from Amgen and Janssen. VP: received advisory board fees, lecture fees, and consulting fees from AbbVie, Janssen, and Amgen; advisory board fees and lecture fees from Takeda, Roche, Pliva, and Sandoz; lecture fees from Alvogen and Oktal Pharma. S-PY: advisory board member for AbbVie, Amgen, Janssen, Astellas, Astex, and Takeda. NF: honoraria from Amgen, Pfizer, Gilead, and AbbVie; speakers bureau for Amgen, Pfizer, and Gilead; advisory board for Amgen, Pfizer, Gilead, and AbbVie; travel support from Amgen, Pfizer, Gilead, and AbbVie. KY: consultancy (includes expert testimony) for AbbVie, AstraZeneca, Celgene, Chugai, Daiichi Sankyo, Eisai, HUYA, Meiji Seika Pharma, MSD, Mundipharma, Ono, Otsuka, Stemline Therapeutics and Takeda; research funding from AbbVie, Astra-Zeneca, Bayer, Celgene, Chugai, Eisai, Gilead Sciences, IQIVA/Incyte, MSD, Mundipharma, Nippon Shinyaku, Novartis, Ono, Otsuka, Solasia Pharma, SymBio, Takeda, Yakult and Zenyaku; honoraria from AbbVie, Bristol-Myers Squibb, Celgene, Chugai, Eisai, IQIVA/HUYA, Janssen, Kyowa Kirin, Meiji Seika Pharma, Mochida, MSD, Mundipharma, Nippon Shinyaku, Novartis, Ono, Otsuka, Pfizer, Sanofi, Sumitomo Dainippon, and Takeda. YO: has served on advisory boards for AbbVie. AHW: served in an advisory role for Astellas, AbbVie/Genentech, Amgen, Celgene/BMS, Novartis, Astra Zeneca, Servier, Janssen, MacroGenics, Pfizer, Gilead, and Syndax; received research funding from Astellas, Astex, AbbVie, Genentech, Amgen, Astra Zeneca, Celgene/BMS, Novartis, Servier, and Syndax; honoraria from Astellas, AbbVie, Genentech, Amgen, Astra Zeneca, Celgene/BMS, Novartis, Servier, Janssen, MacroGenics, Pfizer, Gilead, and Syndax; served as a consultant for: Astellas, Servier, Janssen, Gilead, and Syndax; is an employee of Walter and Eliza Hall Institute (WEHI) and is eligible for financial benefits associated with payments which WEHI receives in relation to venetoclax. WF: advisory and consulting role for Amgen; advisory role for ARIAD/Incyte, Novartis, Pfizer; Celgene, Morphosys, AbbVie, Jazz Pharmaceuticals, and Servier; royalties from Amgen; support for meeting attendance from Amgen, Gilead, Servier, Jazz Pharmaceuticals, and Daiichi Sankyo; research funding from Amgen and Pfizer. IK, XW, VI, DS, and MT: nothing to disclose. CNB, RK, JP, and WM: employees of AbbVie and may hold stock or stock options. KB is a former employee of AbbVie and may hold stock or stock options. JD: employee of Genentech and may hold stock in the company. Venetoclax is being developed in a collaboration between AbbVie and Genentech. AbbVie and Genentech funded NCT02993523 and AbbVie funded NCT03069352 and participated in the given study design, research, analysis, data collection, interpretation of data, reviewing, and approval of the publication. All authors had access to relevant data and participated in the drafting, review, and approval of this article. No honoraria or payments were made for authorship.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pratz, K.W., Panayiotidis, P., Recher, C. et al. Venetoclax combinations delay the time to deterioration of HRQoL in unfit patients with acute myeloid leukemia. Blood Cancer J. 12, 71 (2022). https://doi.org/10.1038/s41408-022-00668-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-022-00668-8
This article is cited by
-
To live is well but to live well is better: venetoclax combination therapy and quality-of-life in acute myeloid leukemia
Blood Cancer Journal (2022)
-
Progress and Challenges in Survivorship After Acute Myeloid Leukemia in Adults
Current Hematologic Malignancy Reports (2022)