By Owen Harries, Department of Oral and Maxillofacial Surgery, University Hospital of South Manchester and Jessica Hutton, General Dental Practitioner, Manchester

©Xuanyu Han/Moment/Getty Images Plus
Introduction
Oro-antral communications and fistulas (OACs & OAFs) are common complications confronting dentists and oral and maxillofacial surgeons. An OAC is an unnatural communication (hole) between the oral cavity and the maxillary sinus.1 Predominantly these complications occur during extraction of upper molar and premolar teeth (48%).2 This happens due to the anatomic proximity of the roots to the maxillary sinus. Other causes of OACs include tuberosity fracture, dentoalveolar/periapical infections, iatrogenic damage (e.g. root or implant dislodged into maxillary sinus or inappropriate elevation), trauma, presence of maxillary cysts or tumours and osteoradionecrosis.3 OACs can be further categorised as alveolo-sinusal, palatal-sinusal, and vestibulo-sinusal based on their location.
Oro-antral fistula
An OAF is an epithelialised pathological unnatural communication between the oral cavity and maxillary sinus.4 It develops when the OAC remains patent and gets epithelialised. This process usually begins within the first 48-72 hours alongside osteitis of the surrounding bony margins, presence of foreign bodies or development of maxillary sinusitis. These developments hamper spontaneous healing leading to chronic fistula formation. On average, it takes 7-8 days for an OAC to become a chronic fistulous tract.2
Radiographs can be helpful such as a new patient exam or to detect if there is a root remaining, root in antrum, osteomyelitis or neoplasia
Diagnosis
OACs can usually be diagnosed clinically through an examination and patient history.4 A summary of signs and symptoms of an OAC can be seen in Table 1. However, some patients may be asymptomatic. While a large communication is easily seen in Figure 1, smaller OACs can be difficult to detect. Fogging of a mouth mirror next to the suspected OAC can confirm diagnosis. Radiographs used in the investigation of an OAC must be justified. An OAC may not always show on a radiograph due to the need for X-rays to pass directly through the defect. When seen radiographically, there is evidence of a break in the cortical outline as shown in Figure 2. There are several scenarios where radiographs can be helpful such as a new patient exam or to detect if there is a root remaining, root in antrum, osteomyelitis or neoplasia.5

Fig. 1 Clinical OAC on intra-oral communication4

Fig. 2 Periapical radiograph showing an OAC (white arrow) following the extraction site of the right maxillary first molar.5
When investigating a possible OAC, asking the patient to pinch their nose and blow may be used, but it is not recommended due to the risk of tearing the antral lining. Probing of the communication should never be attempted
Pre-operative management
Radiographs should be taken prior to treatment to visualise local anatomy and vital structures. Studies show panoramic radiographic assessment is not a reliable method for assessing the risk factors for OAC.4 However, if the root and sinus floor are superimposed on the radiograph, the relative probability of OAC increases during extraction.
Smaller OACs (up to 5mm) can naturally heal in the absence of infection of the maxillary sinus through secondary healing following blood clot formation.
When considering the risk of an OAC the following radiographic features should be considered:
-
Size of the antrum and proximity to teeth
-
Shape and size of teeth and roots
-
Presence of periapical pathology.
OACs are found to be statistically more frequent in patients above the age of 40. Lone standing molars and patients with history of an OAC are more prone to communications forming.6 Patients should be warned about the risk of an OAC and its sequela where appropriate and valid consent must be gained before treatment is carried out. Careful planning of the extraction should take place prior to treatment with consideration for surgical extraction. This preserves more of the bone which forms the sinus floor and reduces the risk of creating an OAC but the risk can never be eliminated entirely.
Initial management of an OAC under 5mm
Smaller OACs (up to 5mm) can naturally heal in the absence of infection of the maxillary sinus through secondary healing following blood clot formation.2 Therefore, a conservative approach is employed for treatment.
-
1.
The socket should be cleaned and debrided, gentle irrigation with saline
-
2.
Pack the socket with oxidised cellulose to stabilise the clot. Care must be taken so as to not push the oxidised cellulose into the antrum.
-
3.
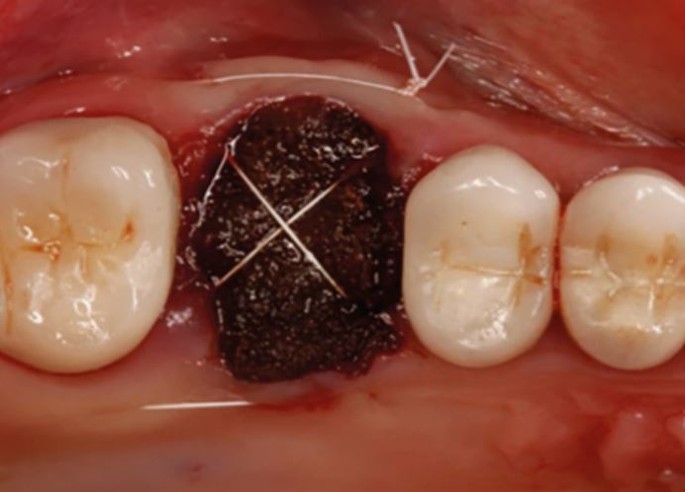
Place a figure-of-eight suture, as shown in Figure 3 - this won't close over the defect, but it will aid healing (primary closure).
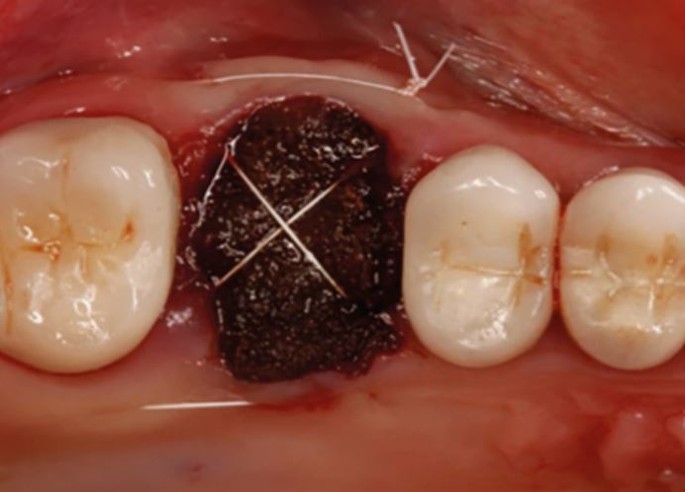
Fig. 3 Closure of an OAC with oxidised cellulose and placement of a figure-of-eight suture4
-
4.
Review the OAC within 2/52, refer the patient for surgical intervention if the defect fails to close.
Specific post-operative OAC advice
An increase in the pressure of the sinus can cause the repaired wound to breakdown therefore the following advice should be given:7
-
Standard post-operative instructions
-
Don't blow nose or hold sneezes
-
Avoid sucking straws or sweets
-
Expect to cough up dried blood form the back of the throat.
Explain that an OAC may not heal and further surgical treatment may be required.
Pharmacological management
Antibiotics are justified in cases of an OAC because some commensal bacteria in the mouth may contaminate the wound or sinus increasing the risk of infection.1
-
Broad spectrum antibiotics
-
First line antibiotics: Amoxicillin
-
For penicillin allergic patients, Clindamycin is indicated
-
Chlorhexidine (0.2%) mouthwash tds
-
-
Nasal decongestant such as Ephedrine (0.5%)
-
Steam inhalations - an aromatic substance such as menthol or eucalyptus should be used
-
Analgesia: NSAIDs and or paracetamol.
Ephedrine should be used with caution with patients that suffer from cardiovascular disease, hypertension, diabetes and who are being treated for depression with medication. Nose drops are used in the nostril on the affected side only and should never be used for more than seven days.8
Early treatment is key for successful closure and therefore knowledge to assess of the defect and selecting appropriate management is vital.
Management of an OAC 5mm and bigger
Untreated larger defects can lead to development of acute sinus disease like sinusitis.1 Therefore, closure within 24 hours is very important to prevent any food or saliva accumulation. It can cause sinus contamination leading to infection, impaired healing and chronic sinusitis. Numerous closure techniques have been described in the literature such as autogenous bone grafts, allogeneic materials, xenografts and synthetic closure although the most common treatment is autogenous soft tissue grafts.4 The three most commonly used treatments are described below. There are two basic principles to follow for surgical closure. Firstly, the sinus and wound must be infection free. Secondly the soft tissue flap must me well vascularised, tension free and over the intact bone.2 The same advice and pharmacological management is employed as described earlier. Management using an acrylic splint to cover the defect when surgical intervention is contraindicated has provided positive outcomes.9
Buccal Advancement Flap (BAF)
This is the simplest of the three flaps to perform and produces the least post-operative pain and discomfort. However, it has limited extent and causes loss of vestibular depth which can cause issues if dentures are made in the future. It is performed by placing two vertical releasing incisions in a trapezoidal shape. The buccal flap is raised and placed over the defect and sutured using horizontal mattress sutures from the buccal to the palatal mucosa.10
Palatal Rotation Flap (PRF)
The PRF can be used on large defects and helps to preserve the buccal vestibular depth. The flap is well vascularised and is firm and more resistant to trauma and infection. However, the palatal flap is feasible only in cases of closing fistulas in the premolar region. It also causes stripping of the palatal surface leading to development of surface irregularities due to secondary intention healing post operatively. The clinical technique is more complicated and therefore can lead to flap necrosis. The procedure starts by excising the surrounding tissue and exposing the OAC. The full thickness palatal flap which is supplied by the greater palatine artery is raised having a posterior base. The flap is then rotated and should be sutured, tension free, into position. Anteriorly the flap must be sufficiently long to allow for lateral rotation and wide enough to completely cover the OAC.5
Buccal fat pad flap (BFP)
The BFP is advantageous as it highly vascularised and has a high rate of success. It is most commonly used in the closure of the OAF. This is due to its location and ease of access with minimal dissection. The incision is made in the area of the zygomatic buttress. Dissection with fine curved artery forceps is done to expose the yellowish coloured buccal fat. The BFP is sutured over the defect to epithelialise.11
Conclusion
OACs are frequently seen complications following extraction of maxillary premolar and molars. Dentists should be able to assess risk of an OAC from clinical and radiographic examination. Early treatment is key for successful closure and therefore knowledge to assess the defect and select appropriate management is vital. For OAC under 5mm conservative management and appropriate follow up is appropriate. The BAF is suitable for closure of small and mesial fistulas. The PRF is used for defects in the premolar area. The BFP is suitable for the closure of large posterior OAC/OAFs.
References
Bhalla N, Sun F, Dym H. Management of Oroantral Communications. Oral Maxillofac Surg Clin N Am 2021; 33: 249-262.
Khandelwal P, Hajira N. Management of Oro-antral Communication and Fistula: Various Surgical Options. World J Plast Surg 2017; 6: 3-8.
Dym H, Wolf J. Oroantral Communication. Oral Maxillofac Surg Clin N Am 2012; 24: 239-247.
Parvini P, Obreja K, Begic A, et al. Decision-making in closure of oroantral communication and fistula. Int J Implant Dent 2019; 5: 13.
Shahrour R, Shah P, Withana T, Jung J, Syed A. Oroantral communication, its causes, complications, treatments and radiographic features: A pictorial review. Imaging Sci Dent 2021; 51: 307.
Lewusz-Butkiewicz K, Kaczor K, Nowicka A. Risk factors in oroantral communication while extracting the upper third molar: Systematic review. Dent Med Problems 2018; 55: 69-74.
British Association of Oral Surgeons. Information for patients: Oro-antral Communication (OAC). 2022. Available online at: www.baos.org.uk/wp-content/uploads/2019/03/Oral-antral-Communications-final.pdf (accessed November 2022).
BNF. Ephedrine hydrochloride | Drugs | BNF content published by NICE. 2022. Available online at: https://bnf.nice.org.uk/drugs/ephedrine-hydrochloride/#cautions (accessed November 2022).
Logan R, Coates E. Non-surgical management of an oro-antral fistula in a patient with HIV infection. Aust Dent J 2003; 48: 255-258.
Belmehdi A, El Harti K. Management of oroantral communication using buccal advanced flap. Pan Afr Med J 2019; 34: 69.
Kim M, Han W, Kim S. The use of the buccal fat pad flap for oral reconstruction. Maxillofac Plast Reconstr Surg 2017; 39: 5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harries, O., Hutton, J. A student guide to oro-antral communication. BDJ Student 30, 22–24 (2023). https://doi.org/10.1038/s41406-022-0920-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41406-022-0920-8