Abstract
Tight junctions (TJs) play an important role in the maintenance of epithelial and endothelial barriers. Zonula occludens (ZO) proteins are scaffolding molecules essential for the formation of TJ complexes, and abnormalities in ZO proteins have been implicated in various TJ-associated human diseases such as tumor invasion and metastasis, and barrier dysfunction. Recent studies reveal that liquid–liquid phase separation of ZO proteins drives the polymerization of TJ proteins into a continuous belt, which then recruits various proteins to form the TJ complex to regulate selective paracellular permeability and signal transduction. Herein, we describe recent advances on how ZO phase separation contributes to TJ formation and discuss the potential of phase separation as a target for the treatment of TJ-associated diseases.
Similar content being viewed by others
Introduction
Tight junctions (TJs) play important roles in the formation of epithelial and endothelial diffusion barriers [1,2,3]. The integrated TJ complex is composed of several transmembrane and cytoplasmic proteins, including zonula occludens (ZO) proteins. ZO proteins are scaffolding molecules that ensure the formation of an integrated TJ complex that selectively regulates cellular permeability and signal transduction [1, 4]. Several TJ-associated human diseases have been linked to mutations and/or the dysregulation of ZO proteins. The impairment of TJ complexes results in abnormal transport of macromolecules and the disappearance of cell polarity [5, 6]. ZO proteins are also targeted by various pathogens, including pathogenic bacteria and viruses. Cellular components, such as proteins and other macromolecules, are segregated through phase separation to perform specific functions. Phase separation also concentrates molecules into liquid droplets, which facilitates biochemical reactions; the dysregulation of this process can lead to various diseases [7, 8]. In this review, we describe how the phase separation of ZO proteins drives the formation of TJ complexes to regulate paracellular permeability [9, 10]. We also discuss the potential of targeting ZO proteins, with a focus on strategies that modulate phase separation, for the treatment of TJ-associated diseases.
TJ structure and function
Epithelial and endothelial cells are connected to adjacent cells through cell–cell junctions located at the most apical part of the lateral plasma membrane. TJs, adherens junctions, and desmosomes are the three major types of junctions [11]. TJs are associated with adherens junctions at the apical plasma membrane and comprise both transmembrane and cytoplasmic proteins [1, 2]. The former integrates adjacent cells, whereas the latter form a dense plaque linking membrane proteins to actin filaments and microtubules. Occludin, claudins, and junctional adhesion molecules are typical transmembrane proteins that mediate cell–cell adhesion. Cytoplasmic plaque proteins include adapter, scaffolding, and cytoskeletal proteins, such as cingulin and membrane-associated guanylate kinase (MAGUK) family proteins. ZO-1 is a typical MAGUK family protein that primarily functions as a scaffold at specific locations within cells [12]. Cingulin is located on the cytoplasmic side of epithelial TJs and interacts with ZO-1, ZO-2, and ZO-3; junctional adhesion molecules; and actin filaments [13]. These various types of TJ proteins interact as part of a complex structural and signaling network [13, 14].
The primary physiological role of TJs is to establish a diffusion barrier that restricts paracellular permeability across the epithelium and endothelium. Permeability to specific ions and macromolecules is determined by their size and charge under a given condition. The mechanism is related to the level of TJ proteins [1, 6]. For example, high expression of occludin promotes the diffusion of small hydrophilic molecules across cultured epithelial monolayers. An intramembrane diffusion barrier establishes cell-surface polarity by restricting the flow of lipids and proteins between the apical and basolateral domains of the plasma membrane; the maintenance of apicobasal cell polarity is necessary for normal cellular activities. The TJ complex recruits various regulatory molecules associated with multiple signaling pathways. For example, ZO-1-associated nucleic acid-binding protein (ZONAB) is a transcription factor with high affinity for the Src homology 3 (SH3) domain of ZO-1 that participates in cell proliferation; ZO-1 and ZONAB regulate gene expression in a cell-density-dependent manner [15]. In Madin–Darby canine kidney cell monolayers, cell proliferation and density are decreased by the overexpression of ZO-1 and the inhibition of ZONAB, which reduce cyclin D1-mediated G1-to-S–phase transition and decrease the level of proliferating cell nuclear antigen (PCNA) [16].
Phase separation and TJ formation
ZO-1, a 220-kDa peripheral membrane protein, was the first identified TJ protein and has two homologs—namely, ZO-2 and ZO-3. ZO-1 interacts with other ZO proteins and TJ proteins, as well as with the cytoskeleton, through multiple domains to form the TJ complex [17]. ZO-1 has three N-terminal postsynaptic density 95 (PSD95)/Dlg/ZO-1 (PDZ) domains and a carboxy terminus that interacts with actin filaments. ZO proteins (especially ZO-1) contain long intrinsically disordered regions (IDRs) in the central region of the protein that make phase separation possible (Fig. 1a). The dysregulation of proteins involved in phase separation results in the formation of pathological aggregates; for example, the aggregation of tau protein into tangles is observed in patients with Alzheimer’s disease [7].
a The PDZ/SH3/GUK domains and IDRs are essential for the phase separation of ZO-1. b ZO-1 first binds to adapter proteins of adherens junctions at the cell membrane. When the threshold concentration is reached, ZO-1 condensates recruit other TJ proteins, such as claudin, occludin, and ZONAB, leading to the formation of a TJ belt.
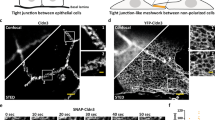
The detailed molecular mechanisms of how TJs are formed are only now starting to be understood. The disruption of ZO-1 results in TJ abnormalities in epithelial cells, highlighting its essential role in TJ formation. The domain organization of ZO proteins facilitates the formation of homo- and heterodimers [18,19,20]. The conserved PSG (PDZ/SH3/guanylate kinase-like [GUK]) domain induces the polymerization of claudins [17, 21]. It has been proposed that ZO proteins change into condensed scaffolds via phase separation and then drive claudin polymerization and the formation of a continuous TJ belt (Fig. 1b). Live-cell photobleaching experiments demonstrate that ZO proteins are highly dynamic, in accordance with the liquid–liquid phase separation of scaffolding proteins [22, 23]. ZO proteins at high concentrations exhibit liquid-like properties in vivo and in vitro. The concentrations required for spontaneous formation of ZO proteins are significantly higher than the endogenous levels required for their activation in vivo. Both in vitro and in vivo assays have indicated that the PSG supradomain plays a critical role in driving the phase separation of ZO-1 via protein–protein interactions (Fig. 1a) [9].
Membrane-bound ZO proteins facilitate the recruitment and enrichment of other TJ proteins (claudin-1 and occludin), cytoskeletal adapters (afadin and cingulin), and regulators (ZONAB and yes-associated protein), leading to the formation of the TJ complex (Fig. 1b). The phosphorylation state of ZO-1 influences the formation of TJ complexes, with dephosphorylation triggering its phase separation [9, 18, 24]. In a study of gastrulation in zebrafish embryos, the phase separation of ZO-1 is required for TJ formation between the enveloping cell and the yolk syncytial layers. The formation of ZO-1 condensates and their movement toward TJs are triggered by actomyosin tension. Impaired phase separation of ZO-1 results in the loss of TJ mechanosensitivity [10].
Phase separation as a potential target
ZO-1 phase separation is essential for TJ complex formation and the maintenance of apical-basal polarity and for ensuring normal paracellular permeability across epithelial and endothelial tissues [25]. Various hereditary TJ-associated human diseases are caused by mutation and the dysregulation of ZO-1, resulting in the loss of cell polarity or compromised barrier function. Decreased levels of ZO-1 and E-cadherin are observed in tumor cell invasion and metastasis, and ZO-1 and ZO-2 are dysregulated along with ZO-1/ZONAB signaling in different types of invasive tumors [1, 2]. In addition, defects in paracellular permeability and associated changes in ion transport are linked to hypertension, cystic fibrosis, and hypomagnesemia. Clarifying the mechanisms underlying the disruption of TJ complex formation and maintenance can provide a basis for developing therapeutic strategies to treat TJ-associated diseases [1, 26].
Tumor invasiveness and metastasis
In human pancreatic cancer, high levels of Zrt- and Irt-related protein 4 (ZIP4) suppress ZO-1 and claudin-1 through interaction with zinc finger E-box–binding homeobox 1 (ZEB1) [27]. The downregulation of ZO-1 promotes tumor growth through focal adhesion kinase (FAK) and paxillin. Based on these observations, inhibiting the ZIP4/ZEB1/ZO-1/claudin-1 pathway is a potential therapeutic strategy in the treatment of pancreatic cancer [28]. Low expression of ZO-1 has been linked to poor prognosis in breast cancer [29]. Several miRNAs have been identified to regulate TJs by targeting ZO-1. For example, miR-25-3p, a cancer-derived exosomal miRNA, participates in the regulation of vascular endothelial growth factor (VEGF) receptor 1 and various TJ proteins through Krüppel-like factor 2 (KLF2). In colorectal cancer, increased miR-25-3 expression results in increased permeability and enhanced metastasis. miR-103 is upregulated in endometrial carcinoma tissues and promotes cell proliferation by directly repressing ZO-1 [30]. The expression of miR-130a is reduced in triple-negative breast cancers (TNBCs), and inhibiting miR-130a reduces the level of ZO-1. High levels of miR-130a inhibit cell migration and invasion through the upregulation of ZO-1 in TNBCs. The effect of miR-130a on ZO-1 can be considered a potential target to suppress cell proliferation in the treatment of TNBCs [31, 32]. Antisense oligonucleotides (ASOs) that mimic the mechanism of action of miRNAs can be used to specifically knockdown repressors of ZO-1 or disrupt its interaction with other molecules to maintain appropriate ZO-1 levels for phase separation and TJ complex formation [22]. Taken together, the current evidence suggests that ZO-1 can serve as a prognostic biomarker in cancer and that therapeutic targeting of ZO-1 is a promising strategy for the treatment of cancer and other diseases (Fig. 2).
Barrier dysfunction
The barrier function of TJs is regulated by different mechanisms in various tissues. Cystic fibrosis is induced by the dysfunction of cystic fibrosis transmembrane conductance regulator (CFTR), a cyclic AMP-activated chloride channel located in the apical membrane of the secretory epithelium of airways, the intestine, bile ducts, and the epididymis [33, 34]. The PDZ domain of CFTR interacts with ZO-1 to regulate cell proliferation and differentiation via the ZO-1/ZONAB pathway. Inhibiting CFTR reduces ZO-1 expression and the recruitment of ZONAB to TJs, resulting in abnormal proliferation and differentiation [35]. A novel therapeutic strategy for the treatment of cystic fibrosis involves increasing CFTR expression at the cell surface to restore chloride flux [33]. CFTR modulators, such as ivacaftor, lumacaftor, and tezacaftor, have been shown to improve CFTR function and demonstrated clinical efficacy in patients with CFTR Phe508 deletion [36, 37]. The loss of blood–brain barrier (BBB) integrity is associated with neuroinflammation and neurodegeneration-related diseases, including Alzheimer’s disease, as well as with postoperative cognitive dysfunction and stroke [38]. Increased membrane permeability and TJ protein downregulation and redistribution are the major features of BBB breakdown, which can be reversed by increasing the expression of ZO-1 [39]. Propofol has neuroprotective effects, including reversing hypoxia and increasing ZO-1 expression and phosphorylation, via the hypoxia-inducible factor 1α/VEGF and calcium/Ca2+/calmodulin-dependent protein kinase II pathways, respectively [40, 41]. Valproic acid, a histone deacetylase inhibitor, inhibits the degradation of ZO-1 through its interaction with hypoxia-inducible factor 1α (HIF1α)/VEGF signaling, thereby protecting against burn-induced gut barrier dysfunction [42]. Thus, small-molecule compounds indirectly alter paracellular permeability by inducing the expression or degradation of ZO-1 (Fig. 2). High-throughput screening can potentially identify novel small-molecule compounds that modulate ZO-1 phase separation, and these compounds may be effective for treating diseases related to barrier dysfunction.
Concluding remarks
Liquid–liquid phase separation is important for the regulation of many dynamic assemblies, including TJ complexes. ZO-1 and PSD95 are MAGUK family proteins that contain multiple protein–protein interaction domains. Phase separation of ZO-1 and PSD95 drives the formation of TJ complexes and the organization of postsynaptic densities in neurons, respectively. ZO-1 condensates not only recruit components of the TJ complex but also facilitate the binding of signaling proteins. These signaling proteins enable the important role of ZO-1 in barrier formation and its physiological roles in cell proliferation and differentiation. Given its widespread cellular and tissue distribution, it is unsurprising that aberrant ZO-1 expression and activity have been implicated in a number of pathophysiological conditions in humans. Deficiency in ZO-1 or other ZOs has been reported in a series of diseases. However, whether excessive expression of ZO-1 is involved in any confined disease is not clear. A high level of ZO-1 might result in abnormal aggregation that influences the recruitment of other TJ proteins or regulators. The level of ZO-1 should be fine-tuned by miRNAs or small-molecule compounds during disease treatment. In this scenario, gradient concentrations of miRNAs or small-molecule compounds should be examined to control ZO-1 to the appropriate level. Moreover, both the method for drug delivery and the duration of drug treatment need to be taken into account for disease treatment.
Determining the conditions that are necessary for the phase separation of ZO-1 may lead to the discovery of an effective treatment for TJ-associated diseases, including cancer. Changes in phosphorylation state, temperature, ion concentration, pH, and the addition of certain drugs have been shown to influence the phase separation of key proteins [26, 43]. The PDZ3-SH3-GUK domain, the core of the MAGUK protein family that participates in various signaling pathways, is unsuitable for the targeting point [21]. However, the IDR of ZO-1 might be targeted to modulate phase separation for its essential role in this process. ASOs that specifically knockdown ZO-1 regulators—which are less widespread than ZO-1 itself and are, therefore, more useful targets—can restore normal levels of ZO-1 and enable its phase separation. Small-molecule compounds, such as propofol and valproic acid, that do not directly target ZO-1 but enhance BBB integrity are another option [40, 42]. The most effective strategy for the identification of such compounds is to screen those that can bind to ZO-1 and have the chemical properties required to influence ZO-1 phase separation. Further investigation is needed to elucidate the molecular basis of TJ-associated diseases so that suitable ASOs can be designed and small-molecule compounds can be identified based on the structure of ZO-1, especially the domains essential for its phase separation.
References
Zihni C, Mills C, Matter K, Balda MS. Tight junctions: from simple barriers to multifunctional molecular gates. Nat Rev Mol Cell Biol. 2016;17:564–80.
Balda MS, Matter K. Tight junctions at a glance. J Cell Sci. 2008;121:3677–82.
Matter K, Balda MS. Signalling to and from tight junctions. Nat Rev Mol Cell Biol. 2003;4:225–36.
Garbett D, Bretscher A, Kozminski KG. The surprising dynamics of scaffolding proteins. Mol Biol Cell. 2014;25:2315–9.
Bhat AA, Uppada S, Achkar IW, Hashem S, Yadav SK, Shanmugakonar M, et al. Tight junction proteins and signaling pathways in cancer and inflammation: a functional crosstalk. Front Physiol. 2018;9:1942.
Tsukita S, Yamazaki Y, Katsuno T, Tamura A, Tsukita S. Tight junction-based epithelial microenvironment and cell proliferation. Oncogene. 2008;27:6930–8.
Boeynaems S, Alberti S, Fawzi NL, Mittag T, Polymenidou M, Rousseau F, et al. Protein phase separation: a new phase in cell biology. Trends Cell Biol. 2018;28:420–35.
Li P, Banjade S, Cheng HC, Kim S, Chen B, Guo L, et al. Phase transitions in the assembly of multivalent signalling proteins. Nature. 2012;483:336–40.
Beutel O, Maraspini R, Pombo-Garcia K, Martin-Lemaitre C, Honigmann A. Phase separation of zonula occludens proteins drives formation of tight junctions. Cell. 2019;179:923–36.
Schwayer C, Shamipour S, Pranjic-Ferscha K, Schauer A, Balda M, Tada M, et al. Mechanosensation of tight junctions depends on ZO-1 phase separation and flow. Cell. 2019;179:937–52.
Tsukita S, Furuse M, Itoh M. Multifunctional strands in tight junctions. Nat Rev Mol Cell Biol. 2001;2:285–93.
Ye F, Zeng M, Zhang M. Mechanisms of MAGUK-mediated cellular junctional complex organization. Curr Opin Struct Biol. 2018;48:6–15.
Citi S, Pulimeno P, Paschoud S. Cingulin, paracingulin, and PLEKHA7: signaling and cytoskeletal adaptors at the apical junctional complex. Ann N Y Acad Sci. 2012;1257:125–32.
Cavey M, Lecuit T. Molecular bases of cell-cell junctions stability and dynamics. Cold Spring Harb Perspect Biol. 2009;1:a002998.
Spadaro D, Tapia R, Jond L, Sudol M, Fanning AS, Citi S. ZO proteins redundantly regulate the transcription factor DbpA/ZONAB. J Biol Chem. 2014;289:22500–11.
Sourisseau T, Georgiadis A, Tsapara A, Ali RR, Pestell R, Matter K, et al. Regulation of PCNA and cyclin D1 expression and epithelial morphogenesis by the ZO-1-regulated transcription factor ZONAB/DbpA. Mol Cell Biol. 2006;26:2387–98.
Pan L, Chen J, Yu J, Yu H, Zhang M. The structure of the PDZ3-SH3-GuK tandem of ZO-1 protein suggests a supramodular organization of the membrane-associated guanylate kinase (MAGUK) family scaffold protein core. J Biol Chem. 2011;286:40069–74.
Ooshio T, Kobayashi R, Ikeda W, Miyata M, Fukumoto Y, Matsuzawa N, et al. Involvement of the interaction of afadin with ZO-1 in the formation of tight junctions in Madin-Darby Canine kidney cells. J Biol Chem. 2010;285:5003–12.
Rodgers LS, Beam MT, Anderson JM, Fanning AS. Epithelial barrier assembly requires coordinated activity of multiple domains of the tight junction protein ZO-1. J Cell Sci. 2013;126:1565–75.
Umeda K, Ikenouchi J, Katahira-Tayama S, Furuse K, Sasaki H, Nakayama M, et al. ZO-1 and ZO-2 independently determine where claudins are polymerized in tight-junction strand formation. Cell. 2006;126:741–54.
Utepbergenov DI, Fanning AS, Anderson JM. Dimerization of the scaffolding protein ZO-1 through the second PDZ domain. J Biol Chem. 2006;281:24671–7.
Shen L, Weber CR, Turner JR. The tight junction protein complex undergoes rapid and continuous molecular remodeling at steady state. J Cell Biol. 2008;181:683–95.
Spadaro D, Le S, Laroche T, Mean I, Jond L, Yan J, et al. Tension-dependent stretching activates ZO-1 to control the junctional localization of its interactors. Curr Biol. 2017;27:3783–95.
Yu D, Marchiando AM, Weber CR, Raleigh DR, Wang Y, Shen L, et al. MLCK-dependent exchange and actin binding region-dependent anchoring of ZO-1 regulate tight junction barrier function. Proc Natl Acad Sci USA. 2010;107:8237–41.
Balda MS, Matter K, Schwartz MA, Randi AM, Conway DE, Almagro LO, et al. ZO-1 controls endothelial adherens junctions, cell–cell tension, angiogenesis, and barrier formation. J Cell Biol. 2015;208:821–38.
Monahan Z, Ryan VH, Janke AM, Burke KA, Rhoads SN, Zerze GH, et al. Phosphorylation of the FUS low-complexity domain disrupts phase separation, aggregation, and toxicity. EMBO J 2017;36:2951–67.
Zeng Q, Liu YM, Liu J, Han J, Guo JX, Lu S, et al. Inhibition of ZIP4 reverses epithelial-to-mesenchymal transition and enhances the radiosensitivity in human nasopharyngeal carcinoma cells. Cell Death Dis. 2019;10:588.
Liu M, Yang J, Zhang Y, Zhou Z, Cui X, Zhang L, et al. ZIP4 promotes pancreatic cancer progression by repressing ZO-1 and claudin-1 through a ZEB1-dependent transcriptional mechanism. Clin Cancer Res. 2018;24:3186–96.
Takai E, Tan X, Tamori Y, Hirota M, Egami H, Ogawa M. Correlation of translocation of tight junction protein Zonula occludens-1 and activation of epidermal growth factor receptor in the regulation of invasion of pancreatic cancer cells. Int J Oncol. 2005;27:645–51.
Du J, Zhang F, Zhang L, Jia Y, Chen H. MicroRNA-103 regulates the progression in endometrial carcinoma through ZO-1. Int J Immunopathol Pharmacol. 2019;33:2058738419872621.
Wang Y, Zhang X, Tang W, Lin Z, Xu L, Dong R, et al. miR-130a upregulates mTOR pathway by targeting TSC1 and is transactivated by NF-κB in high-grade serous ovarian carcinoma. Cell Death Differ. 2017;24:2089–100.
Chen X, Zhao M, Huang J, Li Y, Wang S, Harrington CA, et al. microRNA-130a suppresses breast cancer cell migration and invasion by targeting FOSL1 and upregulating ZO-1. J Cell Biochem. 2018;119:4945–56.
Chaudary N. Triplet CFTR modulators: future prospects for treatment of cystic fibrosis. Ther Clin Risk Manag. 2018;14:2375–83.
Moran O. The gating of the CFTR channel. Cell Mol Life Sci. 2017;74:85–92.
Ruan YC, Wang Y, Da Silva N, Kim B, Diao RY, Hill E, et al. CFTR interacts with ZO-1 to regulate tight junction assembly and epithelial differentiation through the ZONAB pathway. J Cell Sci. 2014;127:4396–408.
Zemanick ET, Accurso FJ. Entering the era of highly effective CFTR modulator therapy. Lancet. 2019;394:1886–8.
Davies JC, Moskowitz SM, Brown C, Horsley A, Mall MA, McKone EF, et al. VX-659-Tezacaftor-Ivacaftor in patients with cystic fibrosis and one or two Phe508del alleles. N Engl J Med. 2018;379:1599–611.
Obermeier B, Daneman R, Ransohoff RM. Development, maintenance and disruption of the blood-brain barrier. Nat Med. 2013;19:1584–96.
Bergmann S, Lawler SE, Qu Y, Fadzen CM, Wolfe JM, Regan MS, et al. Blood-brain-barrier organoids for investigating the permeability of CNS therapeutics. Nat Protoc. 2018;13:2827–43.
Chen W, Ju XZ, Lu Y, Ding XW, Miao CH, Chen JW. Propofol improved hypoxia-impaired integrity of blood-brain barrier via modulating the expression and phosphorylation of zonula occludens-1. CNS Neurosci Ther. 2019;25:704–13.
Sun B, Ou H, Ren F, Huan Y, Zhong T, Gao M, et al. Propofol inhibited autophagy through Ca2+/CaMKKβ/AMPK/mTOR pathway in OGD/R-induced neuron injury. Mol Med. 2018;24:58.
Wang JH, Lee EJ, Ji M, Park SM. HDAC inhibitors, trichostatin A and valproic acid, increase E-cadherin and vimentin expression but inhibit migration and invasion of cholangiocarcinoma cells. Oncol Rep. 2018;40:346–54.
Banani SF, Lee HO, Hyman AA, Rosen MK. Biomolecular condensates: organizers of cellular biochemistry. Nat Rev Mol Cell Biol. 2017;18:285–98.
Acknowledgements
This work was supported by a grant from the Natural Science Foundation of Shandong Province (ZR2018BC002).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Sun, S., Zhou, J. Phase separation as a therapeutic target in tight junction-associated human diseases. Acta Pharmacol Sin 41, 1310–1313 (2020). https://doi.org/10.1038/s41401-020-0470-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-020-0470-y
Keywords
This article is cited by
-
MicroRNAs from Holarrhena pubescens stems: Identification by small RNA Sequencing and their Potential Contribution to Human Gene Targets
Functional & Integrative Genomics (2023)