Abstract
Sphingosylphosphorylcholine (SPC) is a bioactive sphingolipid in blood plasma that is metabolized from the hydrolysis of the membrane sphingolipid. SPC maintains low levels in the circulation under normal conditions, which makes studying its origin and action difficult. In recent years, however, it has been revealed that SPC may act as a first messenger through G protein-coupled receptors (S1P1-5, GPR12) or membrane lipid rafts, or as a second messenger mediating intracellular Ca2+ release in diverse human organ systems. SPC is a constituent of lipoproteins, and the activation of platelets promotes the release of SPC into blood, both implying a certain effect of SPC in modulating the pathological process of the heart and vessels. A line of evidence indeed confirms that SPC exerts a pronounced influence on the cardiovascular system through modulation of the functions of myocytes, vein endothelial cells, as well as vascular smooth muscle cells. In this review we summarize the current knowledge of the potential roles of SPC in the development of cardiovascular diseases and discuss the possible underlying mechanisms.
Similar content being viewed by others
Introduction
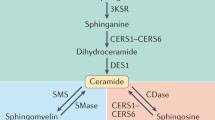
Sphingosylphosphorylcholine (SPC) is a naturally occurring bioactive sphingolipid that shares a similar structure and function with ceramide, sphingosine-1-phosphate (S1P), and lysosphingolipids. It is composed of a long-chain sphingosine and phosphorylcholine. SPC is either metabolized from sphingomyelin or produced by platelets under the effect of stimulation [1, 2]. Under normal conditions, the level of SPC in the circulation is very low (50 nM in plasma, 130 nM in serum) [3]. Certain amounts of SPC exist as a component of lipoproteins, such as high-density lipoprotein (HDL) and low-density lipoprotein (LDL) [4]. Similar to other bioactive sphingolipids, SPC is engaged in numerous cellular processes, such as cell differentiation [5, 6], proliferation [7], and apoptosis [8].
Cardiovascular disease includes a class of diseases that involve the heart, blood vessels, or both. It is the leading cause of death worldwide. Clarifying the pathogenic mechanisms and searching for effective drugs have great significance in relieving the burden caused by diseases. Studies have uncovered potential roles of bioactive sphingolipids in the development of cardiovascular disease. For example, ceramide was found to be involved in the induction of cardiac dysfunction after ischemia/reperfusion [9]. On the other hand, the ceramide derivative S1P has been shown to exert a potent cardioprotective action and an anti-atherosclerosis effect [10]. The function of SPC in diverse human organ systems and human diseases has acquired increasing attention in recent years. Studies in the past decade have identified SPC as an important factor involved in several major human diseases, such as subarachnoid hemorrhage [11], atopic dermatitis [12], Niemann-Pick disease [1], and malicious tumor [13]. HDL is a well-known beneficial factor that can inhibit atherosclerosis. As a component of HDL, SPC may also possess an anti-atherosclerosis effect. The release of SPC in the circulation during coagulation by platelet activation implies a certain effect of SPC in modulating the pathological process of the vasculature and heart. In this review, we summarize the role of SPC in the development of cardiovascular diseases and discuss the possible underlying mechanisms.
Mechanism of action of SPC
SPC may work as an endogenous second messenger
Early findings suggested that SPC was principally an endogenous second messenger mediating Ca2+ release through targeting intracellular proteins. To date, however, little progress has been made in the identification of the intracellular target proteins of SPC. SPC is a popular Ca2+ inducer in a variety of cell types. In addition to the classic inositol trisphosphate receptor signaling pathway, SPC can affect the kinetic properties and function of the ryanodine receptor (RyR) protein in skeletal muscle cells and cardiac myocytes [14,15,16]. SPC binds directly to the cytoplasmic side of the RyR protein in a location in or near the membrane dielectric, but distinct from cytoplasmic Ca2+ binding sites, thus modulating its gating kinetics. SPC was recognized as an inhibitor of calmodulin (CaM), a Ca2+ binding protein that can modulate various target proteins such as kinases or enzymes and thus influence apoptosis, inflammation, muscle contraction, and many other crucial cellular processes [17]. The conformation of the SPC/CaM complex and the modulating mechanism of lipids were recently characterized by Erika Kovacs et al. [18, 19]. SPC can bind with CaM and shield the domain associated with target proteins, thus blocking downstream signal transduction. Since RyRs are also target proteins of CaM, there exists a negative feedback regulation of Ca2+CaM on this channel. SPC can promote the activation of the channel through disruption of the inhibitory complex of Ca2+CaM/RyRs, leading to Ca2+ release from the inner stores [20]. All these studies present a novel insight into the lipid–protein interaction. SPC can be employed as a powerful research tool to understand the lipid–protein modulation model.
SPC works as a first messenger through G protein-coupled receptors (GPCRs)
SPC occurs naturally in blood circulation (50 nM in plasma, 130 nM in serum) [3], most of which exist in the circulation in the HDL-associated form for the sake of stability [21]. The circulating SPC profoundly regulates cardiovascular functions [4, 22]. This suggests that SPC may be able to work as an extracellular agent to modulate target cell function.
Multiple signal responses to SPC were blocked by pertussis toxin (PTX), an inhibitor of the αi subunits of the G protein, indicating the involvement of cell surface GPCRs [10, 23,24,25,26,27,28]. In recent decades, several GPCRs have been reported to show high affinity to SPC, including S1P1, 2, 3 and GPR12 [29]. Through those receptors, SPC extensively participate in cell signal transduction and cell function manipulation (Fig. 1). The endothelial differentiation gene (EDG) receptor family consists of five known members, EDG1–5, which are officially named S1P1–5. S1P1 and S1P3 are ubiquitously expressed, while S1P5 is abundantly expressed in the brain and may play a pivotal role in brain myelination [29]. By coupling to different subtypes of G proteins, they extensively participate in cell signal transduction and cell function manipulation. S1P1 is linked to Gi proteins and is capable of activating enzymes such as phospholipase C (PLC), kinases including MAPK, ERK, or Akt, and the monomer G protein Rac [30]. S1P3 is linked to Gi, Gq, and G12/13 proteins and displays a remarkable stimulating effect on PLC activity and Ca2+ increase. Furthermore, the ERK, Rho, and Rac signaling pathways are also activated by S1P3 [31]. S1P5 is coupled via Gq/11, Gi, and Gs to PLC or MAPK activation and adenylate cyclase stimulation [32,33,34]. GPR12 was found to enhance the Ca2+ increase and stimulate the G protein-gated inwardly rectifying K+ currents through coupling to the Gi protein in response to SPC [35].
Schematic diagram depicting SPC’s action as a first messenger through GPCRs. GPCRs including S1P1, 2, 3, and GPR12 have been reported to show high affinity to SPC. Through coupling to different subtypes of G proteins, they extensively participate in cell signal transduction and cell function manipulation. S1P1 is linked to Gi proteins and activates enzymes such as phospholipase C (PLC) and kinases including MAPK, ERK Akt, and Rac. S1P3 is linked to Gi, Gq, and G12/13 proteins and increases PLC activity and Ca2+ concentration. The ERK, Rho, and Rac signaling pathways are also activated by S1P3. S1P2 is coupled via Gi, Gq/11, and Gs to PLC, adenylate cyclase activity, and MAPK activation. Through coupling to the Gi protein, GPR12 can enhance the Ca2+ and stimulate the G protein-gated inwardly rectifying K+ currents
The identification of GPCRs as the mediating mechanism for extracellular bioactive lipid function is a remarkable breakthrough for lipid molecule research. However, this is not precisely the case with SPC. Even though several GPCRs have been proposed, no detailed mechanisms have been well characterized due to a lack of tools that could selectively modify the activity of these receptors.
Possible role of the lipid raft in SPC function
Despite the extensive investigations of GPCRs for SPC, there are signal transductions that are not sensitive to PTX, indicating other mechanisms responsible for extracellular SPC function. Kobayashi et al. proposed the possible role of membrane lipid rafts in the SPC-induced contraction of vascular smooth muscle cells (VSMCs) [36]. During their research, they found that the SPC-induced VSMC contraction effect was not blocked by PTX but was correlated with cholesterol level. Downregulating the membrane cholesterol of rabbit and human VSMCs by pretreating them with β-cyclodextrin greatly impaired the effect of SPC, which suggested a crucial role of cholesterol in the SPC/Src/RhoA-ROCK/Ca2+ sensitization pathway. Lipid rafts are membrane microdomains enriched with cholesterol and sphingolipids. They were recently discovered to be important membrane components for signal transmission [37, 38]. Depleting cholesterol also destroys this structure; thus, the lipid raft may participate in the signal transduction of SPC. Illuminating the specific mechanism requires more research.
SPC in cardiovascular disease
SPC relieves myocardial infarction (MI)
MI is a heart disease with rather high fatality worldwide. It occurs as a result of coronary artery stenosis and is caused by a lack of oxygen within cardiac muscles. SPC, an important component of HDL, was demonstrated to have a beneficial effect in a mouse model of transient myocardial ischemia/reperfusion [39]. Both pre-ischemic and post-ischemic intravenously injected SPC could reduce the infarct size induced by ischemia (30 min)/reperfusion (24 h) treatment. Apoptosis and inflammation, two characteristic features of MI, were inhibited by SPC both in vitro and in vivo. It appears that the sphingolipid works as a first messenger by acting on a family of GPCRs [25]. So far, multiple GPCRs have been characterized as the receptors of S1P1–5 [29]. The cardioprotective effect of SPC was completely absent in S1P3-deficient mice, implicating that S1P3 has a pivotal role during this process. SPC may share the receptors with S1P due to their similarities in chemical structure (Fig. 2). The specific mechanisms by which SPC modulates apoptosis and inflammation in myocytes have not been clarified yet.
Schematic of the structure of sphingomyelin, SPC and S1P, and the potential interaction between them. SPC is originally generated from sphingomyelin under the catalysis of sphingomyelin deacylase. Additionally, SPC can transform into S1P upon the action of autotoxin. Due to similarities in chemical structure, SPC and S1P share some cellular actions such as mediating mitogenic and antiapoptotic responses or modulating Ca2+ signaling. However, these lipids may also have divergent functions. For example, HL60 cells and human neutrophils respond only to SPC, not to S1P, in the generation of superoxide anions. Novel functions of SPC in regulating cardiomyocyte apoptosis, autophagy, and the differentiation of cardiac stem cells have also been reported recently. Thus, SPC and S1P are both structurally and functionally related but have unique roles under physical or pathological conditions
The role of SPC in human atherosclerosis remains controversial
Atherosclerosis or arteriosclerotic vascular disease is a specific form of arteriosclerosis in which an artery wall thickens due to the invasion and accumulation of white blood cells. Thus, inflammation is a major characteristic of this disease. SPC exists in the circulation either in association with HDL or in a free state released by platelets under injury. Multiple studies in vitro have shown its pronounced influence on vessel pathology [40]. However, unlike S1P, many studies drew conflicting conclusions about the role of SPC in apoptosis and the inflammation of vessel cells [8, 41]. Thus, whether SPC is beneficial or detrimental to atherosclerosis remains undetermined.
Functions of SPC in the cardiovascular system
SPC in the heart
SPC lowered the heart rate
SPC decreased the heart rate in a concentration-dependent manner in isolated guinea pig hearts [42]. The normal function of the heart relies on the production and expansion of action potentials. The abnormal expression and function of the cell membrane ion channels are the fundamental pathologies behind several heart diseases. Thus, SPC may influence the heart rate through modulating ion channels in cardiomyocytes.
SPC controls the ion current in cardiomyocytes
SPC activates K+ channels in a species-dependent manner: SPC activated muscarinic receptor-activated inward rectifier K+ current I(K.ACh) in guinea pig atrial myocytes with an EC50 of 1.5 nM, displaying similar potency as S1P (EC50, 1.2 nM) [42]. However, the effect of SPC on I(K.ACh) was species dependent [43]. Distinct from S1P, SPC failed to elicit the K+ current in mouse and human atrial myocytes. SPC may modulate the K+ current through GPCRs since the channel activation was PTX sensitive. However, the specific GPCRs mediating this process have not been identified.
SPC induces sarcoplasmic reticulum Ca2+ release by binding to the cytoplasmic side of the RyR protein
SPC was capable of causing an increase of cytoplasmic Ca2+ levels in bona fide cells through diverse mechanisms. Ca2+ is a pivotal modulating factor in cardiodynamics. In isolated cardiac sarcoplasmic reticulum membranes, 50 μM SPC induced the release of 70–80% of the accumulated Ca2+ [14]. Further investigation revealed that SPC bound directly to the cytoplasmic side of the RyR protein in a location in or near the membrane dielectric, but distinct from cytoplasmic Ca2+ binding sites and thus modulated its gating kinetics [15, 16]. Thus, the RyR protein was identified as an intracellular receptor of SPC. This implies that bioactive lipids can work not only as a first messenger but also as an intracellular second messenger.
SPC and sphingosine inhibit Na+ and L-type Ca2+ currents
SPC was also shown to have a pronounced inhibitory effect on inward Na+ and L-type Ca2+ currents in rat ventricular myocytes. The mechanisms of the blocking action were most consistent with an effect of SPC on channel gating [44].
SPC inhibits the apoptosis and inflammation of cardiomyocytes
The in vivo investigation confirmed that SPC could relieve the apoptosis and inflammation of cardiomyocytes during ischemia/reperfusion injury. Since reports about the modulation of SPC on heart apoptosis and inflammation are limited, the specific mechanism remains unclear. In normal neonatal rat cardiac myocytes, SPC (0.1–10 μM) worked as a mitogen to promote hypertrophic growth via the activation of a GPCR and the MAPK signaling cascade [45]. Our lab recently found that SPC protected cardiomyocytes against apoptosis in response to serum deprivation by inducing mTORC1-dependent autophagy in vitro. Further investigations showed that this SPC-induced autophagy was mediated by a lipid raft/PTEN/Akt1 pathway [46]. The function of SPC on cardiac myocytes under ischemic conditions has not been further investigated.
SPC in vessels
SPC in blood vessel contraction
In pig coronary arteries, SPC (1–50 μM) was reported to induce the contraction of the vessel without [Ca2+]i elevation [47]. Thus, it was proposed that SPC may cause the contraction effect through Ca2+ sensitization. As Ca2+ sensitization was the major factor leading to vasospasm and hypertension, clarification of the specific mechanism by which SPC modulates this process might provide significant and valuable references for the therapy of vascular vasospasm disease. Evidence for the involvement of a Rho/Rho-kinase pathway in the SPC-induced Ca2+ sensitization of vascular smooth muscle (VSM) contraction has been reported [47, 48]. In primary cultured porcine coronary VSM and rat aortic VSMCs, the subcellular localization and kinase activity of Src family protein tyrosine kinases (SrcPTKs) were influenced by SPC [49]. A digitized immunocytochemical analysis in VSMCs revealed that SPC induced the translocation of Fyn, but not c-Src, from the cytosol to cell membrane. A SrcPTKs inhibitor, PP1, and eicosapentaenoic acid inhibited the translocation of Rho-kinase from the cytosol to the cell membrane as well as the subsequent contraction induced by SPC. Thus, the translocation and activation of SrcPTKs, including Fyn, played an important role in the Ca2+ sensitization of VSM contractions, which was mediated by a SPC-Rho-kinase pathway.
Sphingolipids are widely accepted to exert their functions through GPCRs. However, according to the studies of Kobayashi [36], the contractive effect of SPC was not mediated through GPCRs since it was not abolished by PTX. Thus, there existed another mechanism mediating the signal transduction of SPC. This was the strong linkage between cholesterol and the Ca2+ sensitization of VSM mediated by a novel SPC/SrcPTK/Rho-kinase pathway in both humans and rabbits [36, 50]. The extent of Ca2+ sensitization correlated well with total cholesterol or LDL cholesterol levels in serum. However, an inverse correlation with the serum level of HDL cholesterol was observed. The depletion of primary cultured VSM cholesterol by β-cyclodextrin resulted in the inhibition of SPC-induced Ca2+ sensitization and vasocontraction. All of this evidence confirmed the role of cholesterol in SPC signal transduction. However, the specific mechanism has not been clarified yet. β-Cyclodextrin resulted in a loss of membrane caveolin-1, a marker of cholesterol-enriched lipid rafts. Lipid rafts were reported to be involved in the signal transduction process. Thus, it is reasonable to conclude that lipid rafts mediated the effect of SPC.
SPC in vein endothelial cells (VECs)
SPC regulates apoptosis and inflammation in VECs: Inflammation and apoptosis are two major characteristics during the progression of atherosclerosis. Thus, investigating the modulating effect of SPC on the apoptosis and inflammation of VECs can provide valuable data for clarifying its role in atherosclerosis. HDL-associated SPC (10 μM) blocked the mitochondrial pathway of apoptosis by activating the S1P/Akt signal pathway in human umbilical vein endothelial cells (HUVEC) under growth factor deprivation conditions [4]. Our lab has revealed that SPC (10 μM) could protect HUVECs from serum starvation-induced apoptosis by downregulating integrin β4/PC-PLC and cytosolic p53 levels [51]. SPC could also regulate the inflammation pathway in HUVECs. HDL-associated SPC had the ability to suppress the TNF-α-induced expression of endothelial cell E-selectin and the translocation of NF-κB into the cell nucleus [41]. This process was mediated through the activation of the PI3K/Akt pathway. From all of these data, we concluded that SPC seems to be a beneficial factor in atherosclerosis.
However, several studies do not agree with this point. SPC was reported to induce the cell death of HUVECs at concentrations higher than 10 μM through a caspase-3-dependent pathway [8]. ROS release and subsequent ERK activation induced by SPC were part of the underlying mechanism. SPC stimulates HUVECs, resulting in Jak/STAT3-mediated, NF-κB-mediated, and AP-1-mediated chemokine CCL2 production [23]. It was also observed that SPC stimulated the expression of adhesion molecule ICAM-1 in HUVECs. This suggested that SPC is a pro-inflammatory factor in HUVECs. Thus, we summarized the dual roles of SPC in the regulation of apoptosis and inflammation in Table 1. Further studies are needed to illustrate the specific function of SPC in HUVEC apoptosis and inflammation.
SPC promotes the angiogenesis of VECs
Angiogenesis is a complex process involving endothelial cell migration, proliferation, and morphologic differentiation. SPC induces chemotactic migration and capillary-like tube formation and accelerates the wound healing process in HUVECs [40, 52]. In vivo assay confirmed the angiogenesis effect of SPC [53]. SPC activates its receptor, GPR4, to induce a Gi-dependent transactivation (phosphorylation) of VEGFR2. VEGFR2 is required for SPC-induced Akt activation. SPC may induce ERK activation via a GPR4-independent pathway. Thus, both ERK and Akt are involved in SPC-stimulated angiogenic effects in endothelial cells. U-PA, an important regulator of angiogenesis, and cell surface-associated plasminogen activator are also involved in this process.
SPC promotes the relaxation of vessels through VECs
SPC increased the intracellular Ca2+ concentration and nitric oxide production in endothelial cells in situ on bovine aortic valves and induced the endothelium-dependent relaxation of bovine coronary arteries [54]. As discussed above, SPC could induce a contractive response in VSMCs. Thus, the modulation of SPC between VSMCs and VECs and vessel contraction and relaxation attracted our attention. Our lab employed a HUVEC and VSMC co-culture system to investigate the effect of HUVECs on VSMC contraction. We found that HUVECs could inhibit the SPC-induced VSMC contractive effect through the integrin β4/Fyn signaling pathway [55].
SPC in VSMCs
SPC promotes migration and inflammation in VSMCs: When the endothelium is intact, SPC acts on endothelial cells. However, once the endothelium is injured, VSMCs are exposed to SPC. SPC can exert a modulating effect on VSMCs thereby influence the blood vessels (Fig. 3). SPC promoted the migration of human aortic smooth muscle cells (SMCs) [56]. The proliferation and migration of VSMCs play a key role in the development of atherosclerosis. SPC also activated the MAPK signaling pathway in VSMCs [57, 58]. In rat cerebral arteries, SPC selectively activated p38MAPK in addition to ERK1/2 and JNK. P38MAPK has been widely reported to participate in the inflammatory process through the activation of NF-kB and the release of inflammation factor MCP-1. In conclusion, the effect of SPC on VSMCs promotes vascular pathology.
Roles of sphingosylphosphorylcholine (SPC) in blood vessels. In normal vessels, the endothelium is intact. SPC acts on endothelial cells and has protective effects on blood vessels. When the endothelium is injured, vascular smooth muscle cells (VSMCs) are exposed to SPC, which is harmful to blood vessels
SPC promotes the differentiation of mesenchymal stem cells to VSMCs
SPC is capable of inducing the differentiation of human adipose tissue-derived mesenchymal stem cells (hADSCs) to smooth muscle-like cell types [24]. SPC induces the expression of several smooth muscle-specific genes, such as alpha-smooth-muscle actin, h1-calponin and SM22α, through the Gi/o-ERK-dependent autocrine secretion of TGF-β, which activates a Smad2-SRF/myocardin-dependent pathway. SPC also induces the expression of smooth muscle-specific genes by activating Rho kinase, which promotes the nuclear translocation of myocardin-related transcription factor A [59]. The contractile and ion channel properties of SMCs differentiated from hADSCs were characterized. The hADSC-SMCs expressed functional L-type voltage-gated Ca2+ channels and displayed contractile activities in response to KCl, carbachol, and L-type Ca2+ channel opener Bay K8644. Furthermore, hADSC-SMCs expressed functional big conductance Ca2+-activated K+ (BK(Ca)) channels. SPC could also promote the cardiac and neuronal differentiation of mouse embryonic stem cells at the morphologic and gene expression levels [60].
Discussion
SPC maintains low levels in the circulation under normal conditions, which makes studying its origin and synthesis difficult. To date, the mechanism of the origin of SPC was clarified from pathological tissues such as atopic dermatitis, where the level of SPC was significantly elevated [5,6,7,8]. SPC could metabolize from the hydroxylation of sphingomyelin by sphingomyelin deacylase. However, though working as a key enzyme in the production process of SPC, a clone of this gene has not been characterized yet. The unclear origin and synthesis of SPC are obstacles to the investigation of its function. Another obstacle to the investigation of SPC is the measurement of this sphingolipid. The metabolism of SPC is rather fast in the blood, which makes measuring its levels difficult. Additionally, the traditional intravenous injection method is not suitable for investigating its function in vivo. Fortunately, by employing MS and HPLC, we succeeded in measuring the level of SPC in serum. We found that the levels of SPC in tissues from cardiac disease patients were elevated compared to the normal sample (data not shown).
In conclusion, SPC exerts a pronounced influence on the cardiovascular system through modulation of the functions of myocytes, VECs and VMSCs. The effect of SPC in myocytes is beneficial, while its role in atherosclerosis has not been clarified yet. SPC could promote the function of the heart by regulating the ion channel and inhibiting apoptosis and inflammation. Reports about regulation in apoptosis and inflammation in VECs are conflicting. SPC induces the migration and inflammatory response in VMSCs. The migration of VMSCs from the middle layer of the vasculature to the outside promotes the development of angiogenesis. Furthermore, vascular inflammation is a factor that accelerates the damage of the lesion. Thus, when encountering injuries exposing VSMCs to blood, SPC circulating in the blood may have access to VSMCs to modulate them and accelerate the development of cardiovascular disease.
References
Nixon GF, Mathieson FA, Hunter I. The multi-functional role of sphingosylphosphorylcholine. Prog Lipid Res. 2008;47:62–75.
Yatomi Y, Ruan F, Hakomori S, Igarashi Y. Sphingosine-1-phosphate: a platelet-activating sphingolipid released from agonist-stimulated human platelets. Blood. 1995;86:193–202.
Liliom K, Sun G, Bünemann M, Virág T, Nusser N, Baker DL, et al. Sphingosylphosphocholine is a naturally occurring lipid mediator in blood plasma: a possible role in regulating cardiac function via sphingolipid receptors. Biochem J. 2001;355:189–97.
Nofer JR, Levkau B, Wolinska I, Junker R, Fobker M, von Eckardstein A, et al. Suppression of endothelial cell apoptosis by high density lipoproteins (HDL) and HDL-associated lysosphingolipids. J Biol Chem. 2001;276:34480–5.
Kim KH, Kim YM, Lee MJ, Ko H-C, Kim M-B, Kim JH. Simvastatin inhibits sphingosylphosphorylcholine-induced differentiation of human mesenchymal stem cells into smooth muscle cells. Exp Mol Med. 2012;44:159–66.
Yamamoto H, Naito Y, Okano M, Kanazawa T, Takematsu H, Kozutsumi Y. Sphingosylphosphorylcholine and lysosulfatide have inverse regulatory functions in monocytic cell differentiation into macrophages. Arch Biochem Biophys. 2011;506:83–91.
Jeon ES, Song HY, Kim MR, Moon HJ, Bae YC, Jung JS, et al. Sphingosylphosphorylcholine induces proliferation of human adipose tissue-derived mesenchymal stem cells via activation of JNK. J Lipid Res. 2006;47:653–64.
Jeon ES, Lee MJ, Sung S-M, Kim JH. Sphingosylphosphorylcholine induces apoptosis of endothelial cells through reactive oxygen species-mediated activation of ERK. J Cell Biochem. 2007;100:1536–47.
Kurek K, Piotrowska DM, Wiesiolek-Kurek P, Chabowska A, Lukaszuk B, Zendzian-Piotrowska M. The role of sphingolipids in selected cardiovascular diseases. Post Hig Med Dosw. 2013;67:1018–26.
Knapp M. Cardioprotective role of sphingosine-1-phosphate. J Physiol Pharmacol. 2011;62:601–7.
Kurokawa T, Yumiya Y, Fujisawa H, Shirao S, Kashiwagi S, Sato M, et al. Elevated concentrations of sphingosylphosphorylcholine in cerebrospinal fluid after subarachnoid hemorrhage: a possible role as a spasmogen. J Clin Neurosci. 2009;16:1064–8.
Hara J, Higuchi K, Okamoto R, Kawashima M, Imokawa G. High-expression of sphingomyelin deacylase is an important determinant of ceramide deficiency leading to barrier disruption in atopic dermatitis. J Invest Dermatol. 2000;115:406–13.
Xu Y, Gaudette DC, Boynton JD, Frankel A, Fang XJ, Sharma A, et al. Characterization of an ovarian cancer activating factor in ascites from ovarian cancer patients. Clin Cancer Res. 1995;1:1223–32.
Betto R, Teresi A, Turcato F, Salviati G, Sabbadini RA, Krown K, et al. Sphingosylphosphocholine modulates the ryanodine receptor/calcium-release channel of cardiac sarcoplasmic reticulum membranes. Biochem J. 1997;322:327–33.
Uehara A, Yasukochi M, Imanaga I, Berlin JR. Effect of sphingosylphosphorylcholine on the single channel gating properties of the cardiac ryanodine receptor. FEBS Lett. 1999;460:467–71.
Yasukochi M, Uehara A, Kobayashi S, Berlin JR. Ca2+ and voltage dependence of cardiac ryanodine receptor channel block by sphingosylphosphorylcholine. Pflug Arch. 2003;445:665–73.
Kovacs E, Liliom K. Sphingosylphosphorylcholine as a novel calmodulin inhibitor. Biochem J. 2008;410:427–37.
Kovacs E, Toth J, Vertessy BG, Liliom K. Dissociation of calmodulin-target peptide complexes by the lipid mediator sphingosylphosphorylcholine: implications in calcium signaling. J Biol Chem. 2010;285:1799–808.
Kovacs E, Harmat V, Toth J, Vertessy BG, Modos K, Kardos J, et al. Structure and mechanism of calmodulin binding to a signaling sphingolipid reveal new aspects of lipid-protein interactions. FASEB J. 2010;24:3829–39.
Kovacs E, Xu L, Pasek DA, Liliom K, Meissner G. Regulation of ryanodine receptors by sphingosylphosphorylcholine: involvement of both calmodulin-dependent and -independent mechanisms. Biochem Biophys Res Commun. 2010;401:281–6.
Scherer M, Boettcher A, Schmitz G, Liebisch G. Sphingolipid profiling of human plasma and FPLC-separated lipoprotein fractions by hydrophilic interaction chromatography tandem mass spectrometry. Biochim Biophys Acta. 2011;1811:68–75.
Alewijnse AE, Peters SLM, Michel MC. Cardiovascular effects of sphingosine-1-phosphate and other sphingomyelin metabolites. Br J Pharmacol. 2004;143:666–84.
Lee HY, Lee SY, Kim SD, Shim JW, Kim HJ, Jung YS, et al. Sphingosylphosphorylcholine stimulates CCL2 production from human umbilical vein endothelial cells. J Immunol. 2011;186:4347–53.
Jeon ES, Moon HJ, Lee MJ, Song HY, Kim YM, Bae YC, et al. Sphingosylphosphorylcholine induces differentiation of human mesenchymal stem cells into smooth-muscle-like cells through a TGF-beta-dependent mechanism. J Cell Sci. 2006;119:4994–5005.
Meyer zu Heringdorf D, Himmel HM, Jakobs KH. Sphingosylphosphorylcholine-biological functions and mechanisms of action. Biochim Biophys Acta. 2002;1582:178–89.
Okajima F, Kondo Y. Pertussis toxin inhibits phospholipase C activation and Ca2+ mobilization by sphingosylphosphorylcholine and galactosylsphingosine in HL60 leukemia cells. Implications of GTP-binding protein-coupled receptors for lysosphingolipids. J Biol Chem. 1995;270:26332–40.
Chin TY, Chueh SH. Sphingosylphosphorylcholine stimulates mitogen-activated protein kinase via a Ca2+-dependent pathway. Am J Physiol. 1998;275:C1255–63.
Lyons JM, Karin NJ. A role for G protein-coupled lysophospholipid receptors in sphingolipid-induced Ca2+signaling in MC3T3-E1 osteoblastic cells. J Bone Miner Res. 2001;16:2035–42.
Meyer zu Heringdorf D, Jakobs KH. Lysophospholipid receptors: signalling, pharmacology and regulation by lysophospholipid metabolism. Biochim Biophys Acta. 2007;1768:923–40.
Okamoto H, Takuwa N, Gonda K, Okazaki H, Chang K, Yatomi Y, et al. EDG1 is a functional sphingosine-1-phosphate receptor that is linked via a Gi/o to multiple signaling pathways, including phospholipase C activation, Ca2+ mobilization, Ras-mitogen-activated protein kinase activation, and adenylate cyclase inhibition. J Biol Chem. 1998;273:27104–10.
Okamoto H, Takuwa N, Yatomi Y, Gonda K, Shigematsu H, Takuwa Y. EDG3 is a functional receptor specific for sphingosine 1-phosphate and sphingosylphosphorylcholine with signaling characteristics distinct from EDG1 and AGR16. Biochem Biophys Res Commun. 1999;260:203–8.
Ancellin N, Hla T. Differential pharmacological properties and signal transduction of the sphingosine 1-phosphate receptors EDG-1, EDG-3, and EDG-5. J Biol Chem. 1999;274:18997–9002.
Windh RT, Lee MJ, Hla T, An S, Barr AJ, Manning DR. Differential coupling of the sphingosine 1-phosphate receptors Edg-1, Edg-3, and H218/Edg-5 to the G(i), G(q), and G(12) families of heterotrimeric G proteins. J Biol Chem. 1999;274:27351–8.
Wang J-Q, Kon J, Mogi C, Tobo M, Damirin A, Sato K, et al. TDAG8 is a proton-sensing and psychosine-sensitive G-protein-coupled receptor. J Biol Chem. 2004;279:45626–33.
Ignatov A, Lintzel J, Hermans-Borgmeyer I, Kreienkamp H-J, Joost P, Thomsen S, et al. Role of the G-protein-coupled receptor GPR12 as high-affinity receptor for sphingosylphosphorylcholine and its expression and function in brain development. J Neurosci. 2003;23:907–14.
Morikage N, Kishi H, Sato M, Guo F, Shirao S, Yano T, et al. Cholesterol primes vascular smooth muscle to induce Ca2 sensitization mediated by a sphingosylphosphorylcholine-Rho-kinase pathway: possible role for membrane raft. Circ Res. 2006;99:299–306.
Suzuki KGN. Lipid rafts generate digital-like signal transduction in cell plasma membranes. Biotechnol J. 2012;7:753–61.
Head BP, Patel HH, Insel PA. Interaction of membrane/lipid rafts with the cytoskeleton: impact on signaling and function membrane/lipid rafts, mediators of cytoskeletal arrangement and cell signaling. Biochim Biophys Acta. 2014;1838:532–45.
Herzog C, Schmitz M, Levkau B, Herrgott I, Mersmann J, Larmann J, et al. Intravenous sphingosylphosphorylcholine protects ischemic and postischemic myocardial tissue in a mouse model of myocardial ischemia/reperfusion injury. Mediat Inflamm. 2010;2010:425191.
Boguslawski G, Lyons D, Harvey KA, Kovala AT, English D. Sphingosylphosphorylcholine induces endothelial cell migration and morphogenesis. Biochem Biophys Res Commun. 2000;272:603–9.
Schmidt A, Geigenmüller S, Buddecke E. The antiatherogenic and antiinflammatory effect of HDL-associated lysosphingolipids operates via Akt—NF-kappaB signalling pathways in human vascular endothelial cells. Basic Res Cardiol. 2006;45:109–16.
Liliom K, Bunemann M, Sun G, Miller D, Desiderio DM, Brandts B, et al. Sphingosylphosphorylcholine is a bona fide mediator regulating heart rate. Ann N Y Acad Sci. 2000;905:308–10.
Himmel HM, Meyer Zu Heringdorf D, Graf E, Dobrev D, Kortner A, Schuler S, et al. Evidence for Edg-3 receptor-mediated activation of I(K.ACh) by sphingosine-1-phosphate in human atrial cardiomyocytes. Mol Pharmacol. 2000;58:449–54.
Yasui K, Palade P. Sphingolipid actions on sodium and calcium currents of rat ventricular myocytes. Am J Physiol. 1996;270:C645–9.
Robert P, Tsui P, Laville MP, Livi GP, Sarau HM, Bril A, et al. EDG1 receptor stimulation leads to cardiac hypertrophy in rat neonatal myocytes. J Mol Cell Cardiol. 2001;33:1589–606.
Yue H-W, Liu J, Liu P-P, Li W-J, Chang F, Miao J-Y, et al. Sphingosylphosphorylcholine protects cardiomyocytes against ischemic apoptosis via lipid raft/PTEN/Akt1/mTOR mediated autophagy. Biochim Biophys Acta. 2015;1851:1186–93.
Todoroki-Ikeda N, Mizukami Y, Mogami K, Kusuda T, Yamamoto K, Miyake T, et al. Sphingosylphosphorylcholine induces Ca(2+)-sensitization of vascular smooth muscle contraction: possible involvement of rho-kinase. FEBS Lett. 2000;482:85–90.
Nakao F, Kobayashi S, Mogami K, Mizukami Y, Shirao S, Miwa S, et al. Involvement of Src family protein tyrosine kinases in Ca(2+) sensitization of coronary artery contraction mediated by a sphingosylphosphorylcholine-Rho-kinase pathway. Circ Res. 2002;91:953–60.
Shirao S, Kashiwagi S, Sato M, Miwa S, Nakao F, Kurokawa T, et al. Sphingosylphosphorylcholine is a novel messenger for Rho-kinase-mediated Ca2+ sensitization in the bovine cerebral artery: unimportant role for protein kinase C. Circ Res. 2002;91:112–9.
Somlyo AV. New roads leading to Ca2+ sensitization. Circ Res. 2002;91:83–4.
Ge D, Jing Q, Meng N, Su L, Zhang Y, Zhang S, et al. Regulation of apoptosis and autophagy by sphingosylphosphorylcholine in vascular endothelial cells. J Cell Physiol. 2011;226:2827–33.
Piao Y-J, Lee C-H, Zhu MJ, Kye K-C, Kim J-M, Seo Y-J, et al. Involvement of urokinase-type plasminogen activator in sphingosylphosphorylcholine-induced angiogenesis. Exp Dermatol. 2005;14:356–62.
Kim K-S, Ren J, Jiang Y, Ebrahem Q, Tipps R, Cristina K, et al. GPR4 plays a critical role in endothelial cell function and mediates the effects of sphingosylphosphorylcholine. FASEB J. 2005;19:819–21.
Mogami K, Mizukami Y, Todoroki-Ikeda N, Ohmura M, Yoshida K, Miwa S, et al. Sphingosylphosphorylcholine induces cytosolic Ca(2+) elevation in endothelial cells in situ and causes endothelium-dependent relaxation through nitric oxide production in bovine coronary artery. FEBS Lett. 1999;457:375–80.
Ge D, Meng N, Su L, Zhang Y, Zhang S-l, Miao J-y, et al. Human vascular endothelial cells reduce sphingosylphosphorylcholine-induced smooth muscle cell contraction in co-culture system through integrin beta 4 and Fyn. Acta Pharmacol Sin. 2012;33:57–65.
Boguslawski G, Grogg JR, Welch Z, Ciechanowicz S, Sliva D, Kovala AT, et al. Migration of vascular smooth muscle cells induced by sphingosine 1-phosphate and related lipids: potential role in the angiogenic response. Exp Cell Res. 2002;274:264–74.
Mathieson FA, Nixon GF. Sphingolipids differentially regulate mitogen-activated protein kinases and intracellular Ca2+ in vascular smooth muscle: effects on CREB activation. Br J Pharmacol. 2006;147:351–9.
Wirrig C, Hunter I, Mathieson FA, Nixon GF. Sphingosylphosphorylcholine is a proinflammatory mediator in cerebral arteries. J Cereb Blood Flow Metab. 2011;31:212–21.
Jeon ES, Park WS, Lee MJ, Kim YM, Han J, Kim JH. A Rho kinase/myocardin-related transcription factor-A-dependent mechanism underlies the sphingosylphosphorylcholine-induced differentiation of mesenchymal stem cells into contractile smooth muscle cells. Circ Res. 2008;103:635–42.
Kleger A, Liebau S, Lin Q, von Wichert G, Seufferlein T. The impact of bioactive lipids on cardiovascular development. Stem Cells Int. 2011;2011:916180.
Acknowledgements
This work was financially supported by the National Science Foundation of China (31501122; 31371158; 31671180; 31070999; 81570454), Science and Technology Developmental Project of Shandong Province (2016GSF201035 and ZR2014CM030), and Shandong Excellent Young Scientist Award Fund (BS2014SW031).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ge, D., Yue, Hw., Liu, Hh. et al. Emerging roles of sphingosylphosphorylcholine in modulating cardiovascular functions and diseases. Acta Pharmacol Sin 39, 1830–1836 (2018). https://doi.org/10.1038/s41401-018-0036-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-018-0036-4