Abstract
Impaired cognition is often overlooked in the clinical management of depression, despite its association with poor psychosocial functioning and reduced clinical engagement. There is an outstanding need for new treatments to address this unmet clinical need, highlighted by our consultations with individuals with lived experience of depression. Here we consider the evidence to support different pharmacological approaches for the treatment of impaired cognition in individuals with depression, including treatments that influence primary neurotransmission directly as well as novel targets such as neurosteroid modulation. We also consider potential methodological challenges in establishing a strong evidence base in this area, including the need to disentangle direct effects of treatment on cognition from more generalised symptomatic improvement and the identification of sensitive, reliable and objective measures of cognition.
Similar content being viewed by others
Introduction
Cognitive impairment is a core feature of major depressive disorder (MDD), broadly characterised by heterogeneous reductions in executive functioning, learning and memory [1,2,3]. Although cognitive impairment occurs in most clinical cases of depression (approximately 85–94%) [4], it is rarely a primary focus of routine clinical management compared with other core features of MDD (e.g. mood disturbances) [5,6,7]. Cognitive impairment presents inimical challenges to quality of life, is associated with poor functional outcomes [8,9,10], and is a key mediator of perceived disability in MDD [11, 12]. Consistent with this, our consultations with individuals with lived experience of depression highlight the impact of impaired cognition on daily living and service engagement (Box 1). Few treatment options for cognitive impairment in depression are available, with no recommended strategies in current clinical practice guidelines for MDD for the United Kingdom, United States or Germany [6, 13,14,15,16]. However, there are several promising novel pharmacological targets, with an increasing evidence base in humans.
In this review, we consider existing evidence from human clinical studies and evaluate potential new directions for pharmacological treatment development for cognitive impairment in MDD. We consider conventional agents which target primary neurotransmission, such as antidepressants, as well as novel pathophysiological targets. In addition, we highlight some methodological challenges of research in this area. The scope of the current review is limited to pharmacological approaches, although psychotherapeutic and transcranial electrotherapy stimulation approaches for cognitive impairment in psychiatric disorders are also being investigated [17,18,19,20].
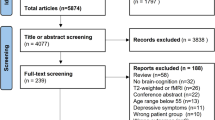
The body of evidence in this narrative review was identified using a literature search to determine relevant human experimental studies, meta-analyses and systematic reviews (further details of the search strategy are described within these databases are described within Supplementary Material 2). Findings from the scientific literature were interpreted in the context of information gathered through consultations with individuals with lived experience of depression.
Pharmacological agents targeting primary neurotransmission
SSRIs and SNRIs
Systematic reviews and meta-analyses of the effects of conventional antidepressant treatment (compared with placebo) on cognitive function in MDD have reported modest positive effect sizes, including improvements across domains of psychomotor speed and delayed recall [21,22,23]. However, these analyses pool data from a broad range of pharmacological agents, including the multimodal agent vortioxetine and the cholinergic agent donepezil [24, 25], which may have inflated the effects seen. Indeed, in one meta-analysis, the effect of antidepressant treatment on cognition became non-significant when vortioxetine studies were excluded [26]. Further, these meta-analyses included heterogenous clinical populations (e.g. depression in Parkinson’s disease), and many studies did not use standardised cognitive assessment batteries, instead making use of highly variable cognitive tasks which lack specificity for cognitive domain measured.
More direct evidence from a parallel-cohort randomised clinical trial (RCT) showed 8-weeks of standard antidepressant monotherapy with sertraline, venlafaxine, or escitalopram had no effect on cognitive performance in MDD across standardised assessments [27]. This evidence is particularly compelling given the large sample size (n = 1008), prospective design (with both pre- and post-treatment assessments) and healthy volunteer control group (to control for non-specific effects of repeated testing and symptomatic changes). These findings are consistent with accounts from our consultations with individuals with lived experience of depression, who often reported that antidepressants did not improve their cognitive impairment (Box 2).
Measuring the direct cognitive effects of drugs which primarily affect mood symptoms of depression is challenging. As depression remits, self-report (subjective) and objective cognitive impairments may not improve in parallel [28, 29]. Further, as subjective cognitive impairment is a symptom of depression within ICD-10 [30] and DSM-V [31] diagnostic classifications, and is measured on most standardised outcome measures for MDD [32,33,34], its improvement may contribute to indices of treatment response/remission. Antidepressants may also change non-specific factors such as motivation, which may increase effortful performance in cognitive tasks leading to improvements in task performance that do not reflect genuine gains in cognitive functioning – a methodological limitation known as pseudo-specificity [35, 36]. Such effects are infrequently controlled for in investigations of the cognitive effects of antidepressants.
5-HTR modulators
Selective targeting of serotonin receptor subtypes may hold potential to more directly modify cognitive functioning [37]. Vortioxetine, a multimodal SSRI with significant affinity for various 5-HT receptor subtypes is the only agent recognised by the FDA as indicated for cognitive impairment in MDD [38]. In particular, vortioxetine is a potent antagonist of the 5-HT3A receptor where it has a 10–38-fold greater affinity compared to the other 5-HT receptor subtypes at which it is active (5-HT1A, 5-HT1D, and 5-HT7) [39]; these broad serotonergic effects are thought to result in downstream modulation of glutamatergic signalling [24, 31, 40]. In multiple placebo-controlled RCTs, eight-weeks of vortioxetine monotherapy in MDD improved domains of executive functioning, learning and memory, with particularly well-replicated improvements on the Digit Symbol Substitution Test (DSST) [41,42,43]; the DSST is a highly sensitive measure of cognitive impairment with low cognitive domain specificity [44]. In a study of healthy volunteers (n = 48) and remitted MDD (n = 48) [45], vortioxetine but not placebo improved executive functioning performance; in addition, greater prefrontal and hippocampal activation was observed during a working memory task following vortioxetine administration, although no effect on objective memory performance was found. In contrast, a healthy volunteer study (n = 24) found no increase in cognitive functioning following vortioxetine administration [46]. Although the beneficial effects of vortioxetine on cognition in MDD are well-replicated, further work is needed to further understand the inconsistent cognitive effects observed in healthy volunteers.
Through path analysis of three clinical studies, McIntyre et al. [47] found DSST improvements following vortioxetine were independent of overall symptomatic improvement on the Montgomery-Asberg Depression Rating Scale (MADRS) [48]. However, it is important to note that these analyses of overall MADRS score do not exclude the possibility that specific symptoms mediated the effects on cognition [49]. For example, anhedonia may decrease motivation and effortful performance in executive functioning tasks [50, 51], and vortioxetine may be efficacious in remediating anhedonic dimensions of MDD [52]; by comparison, other symptom dimensions within the MADRS, such as reduced appetite, are less likely to mediate improved cognition.
Beyond vortioxetine, there is emerging evidence that selective agonists of serotonin receptor subtypes may hold promise as pro-cognitive treatments. For example, an open-label RCT (N = 89), the partial 5-HT1A agonist buspirone, administered as an adjunct to escitalopram for eight weeks, demonstrated improved working memory in MDD compared with escitalopram monotherapy [53]. In contrast, a single dose of buspirone did not affect cognition in healthy volunteers [54]. Tandospirone, a structural analog of buspirone which selectively targets 5-HT1A receptors with high agonist efficacy [55], similarly improved cognitive functioning in older adults with vascular dementia and anxiety (N = 89) [56], when given as an adjunct to escitalopram for eight weeks, compared with escitalopram monotherapy. In contrast, a single dose of tandospirone has been found to dose dependently impair explicit verbal memory in a small sample (N = 9, crossover design) of healthy male volunteers [57]. These limited studies show promise for 5-HT1A as a target for cognitive impairment in depression, although its paradoxical effects in healthy volunteers require further elucidation.
In summary, there is a body of support for the idea that selective 5-HT receptor agonism may be a useful target for cognitive impairment in depression. However, it is important to note that many current 5-HTR modulator agents, such as buspirone and vortioxetine have complex neuropharmacological actions and may also impact cognition via other mechanisms, such as direct pro-dopaminergic [58] or indirect glutaminergic modulation. Further investigation of more selective agonists of 5-HTR subtypes, such as the 5-HT4 receptor agonist prucalopride [59], will further elucidate potential serotonergic targets for cognitive amelioration in MDD. Additionally, many novel 5-HT agonists have recently, or are currently, crossing the clinical threshold, including 5-HT6 receptor agonists and 5-HT7 receptor antagonists [60, 61]. These agents appear to improve cognition in both healthy and neurological rodent models (including Alzheimer’s disease and schizophrenia) [62,63,64,65,66,67,68,69,70,71], and serve as promising novel targets for ameliorating cognitive impairment in MDD.
Dopaminergic modulators
A large body of evidence supports the regulatory role of dopaminergic signalling in cognitive functioning [72,73,74]. Consistent with this, pharmacological manipulation of dopaminergic signalling function with piribedil (D2 and D3 receptor agonist) and methylphenidate (inhibitor of dopamine transporters [DAT]) results in well-replicated improvements in cognitive performance in healthy individuals [75,76,77]. It is therefore interesting to consider whether dopaminergic antidepressant agents, such as bupropion, might have the potential as treatments for cognitive impairment in MDD.
Bupropion (which inhibits the reuptake of dopamine and noradrenaline) has been shown to improve cognitive function in MDD when taken as an adjunct to other antidepressants or as monotherapy [78, 79]. For example, improved visual and verbal memory and executive functioning was observed in patients with MDD after 8-week administration (N = 36) [79], although this effect was not apparent in a separate study of healthy volunteers [80].
Modafinil (which has a complex mechanism of action, including weak inhibition of dopamine reuptake) has also been shown to have pro-cognitive effects in patients with depression. In currently depressed patients 4-weeks administration of modafinil improved executive function (N = 31) [81]. In patients who have recovered from depression, modafinil was shown to improve episodic memory but not executive functioning after one week in remitted depression (N = 60) [82]. This evidence is consistent with multiple studies in healthy adults demonstrating broad improvements in verbal and visuospatial working memory, learning, attention and executive functioning following modafinil administration [81, 83,84,85,86].
Although modafinil and bupropion overlap mechanistically as inhibitors of DAT, bupropion acts on ≤22% of DAT binding sites [87], while modafinil produces weak atypical inhibition of DAT [88, 89]. Bupropion also blocks the reuptake of noradrenaline, with downstream modulation of tumour necrosis factor alpha and upregulation of brain-derived neurotrophic factor (BDNF) in MDD, which may be an alternative intra- and extracellular mechanism by which it exerts its antidepressant and cognitive effects [90, 91]. Similarly, the cognitive effects of modafinil may be explained by intracellular actions, including decreased neuronal free radicals, adenosine 5′-triphosphate production, and promotion of cellular metabolism [89]. Further, given the role of the mesolimbic-dopamine circuitry in reward processing and motivation, it is important to consider the extent to which the cognitive effects of bupropion and modafinil are related to non-specific changes in motivation and affect [35, 36].
NMDA antagonists, AMPAkines, and metabotropic glutamate receptor inhibitors
Glutamatergic neurotransmission accounts for most excitatory activity in cortical structures, and is a predominant regulator of cognitive and sensory functioning [92, 93]. Glutamatergic transmission has gained much attention within the context of depression following the discovery of the potent antidepressant effects of the N-methyl-d-aspartate (NMDA) antagonist ketamine [94]. A single subanaesthetic infusion of ketamine has rapid, transient antidepressant effects in treatment-resistant depression (TRD) [95, 96]. Interestingly, several TRD studies have reported improved cognitive function postinfusion, including improved executive function, visual memory and complex working memory [97,98,99]. Ketamine is also associated with a reduction in suicidal ideation and planning, which it has been suggested could result from improved inhibitory control [100, 101]. The cognitive effects of ketamine may be attributable to the rapid promotion of neuronal plasticity via intracellular protein modulation, including rapamycin complex 1 and BDNF [102, 103], and inhibition of excitotoxicity through modulation of ionotropic and metabotropic glutamate receptors (mGluRs) [104].
It is unclear if ketamine has a direct effect on cognitive function, or if its cognitive effects are an indirect result of its rapid antidepressant properties. In two active placebo-controlled RCTs by Shiroma et al. [105] (N = 43) and Murrough et al. [106] (N = 62), postketamine-infusion improvements in speed of processing and working memory were independent of antidepressant response; however, the cognitive change reported in Murrough et al. [106] was associated with a significant main effect of time only and there were no differences in cognition between the ketamine and active placebo, suggesting the cognitive improvement may have been driven by a non-specific learning effect. An RCT of similar design by Liu et al. [107] (N = 50) found that change in speed of processing post-ketamine was associated with improved anxiety symptoms comorbid to TRD, and improved visual learning and memory performance were associated with improved depressive symptoms in TRD without comorbid anxiety. Two further studies investigating the cognitive effects of ketamine found a moderating effect of depressive symptom improvement on DSST performance and self-reported cognitive deficits, but not visual attention and task-switching performance [108], and a relationship between depressive symptomatic improvement and response inhibition performance [109].
Paradoxically, acute ketamine may induce cognitive impairment in some circumstances: an RCT of non-refractory MDD showed a single subanaesthetic dose reduced performance in executive function, attention and verbal memory [110]. Healthy volunteer studies have demonstrated similar reductions in episodic and working memory, attention and long-term memory both during and 1-hr post-infusion [111,112,113,114], with a return to baseline functioning 3 days post-infusion [115]. Interestingly, fronto-striatal functional connectivity increases in individuals with TRD and decreases in healthy individuals 2-days postinfusion [116], mirroring the opposing effects of ketamine on cognitive ability across these populations. Taken together, the apparent beneficial effects of ketamine on cognition may be specific to TRD, although further work is required. Additionally, the cognitive effects of ketamine may vary depending on dose frequency (single dose vs. repeat dose) and length of treatment [97].
Beyond ketamine, other glutamatergic agents have been investigated for potential cognition improving effects in MDD, including other NMDA antagonists, glutamatergic inhibitors, positive allosteric modulators of AMPAR (AMPAkines) and modulators of mGluRs. The NMDA antagonist riluzole has well-replicated antidepressant effects [117, 118], but did not improve self-reported cognitive impairment when administered as an adjunct to antidepressants [118]. Another NMDA receptor antagonist, memantine, has been shown to have antidepressant effects when administered as an adjunct to escitalopram [119,120,121]. Compared with escitalopram monotherapy, memantine and escitalopram combination therapy improved verbal memory and executive functioning in older adults with MDD [119] (N = 62), although not in younger adults with MDD (N = 80) [122]. The AMPAkine, Org 26576, improved executive functioning and working memory at high doses (n = 10) compared with low dose (n = 10) and placebo (n = 10) in MDD [123]; however, replication in a large cohort study is required [124]. In healthy older adults, an acute dose of a similar AMPAkine (Org 24448) improved short-term memory and executive functioning, but impaired episodic memory [125].
Excitotoxicity and consequential oxidative stress via NMDA hyperactivity is posited as a pathophysiological basis of cognitive impairment in MDD [126, 127], with group I and II mGluRs potentially inhibiting these effects [128, 129]. Although a developing research area, the first mGlu2/3R modulator (decoglurant) to advance to clinical study did not affect objective cognition nor depressive symptoms in an RCT of partial-refractory MDD (N = 357) [129, 130].
Cholinesterase inhibitors
Cholinergic signalling plays a key role in memory processing and cognitive decline [131, 132]. Meta-analyses have demonstrated that cholinergic agents such as citicoline (cholinergic donor for acetylcholine synthesis [133]) administered in neurological populations (e.g. ischemic stroke) facilitate functional and cognitive recovery [134, 135], although these effects are not always replicated [136, 137].
Of the cholinesterase inhibitors investigated within the context of depression [138], donepezil is among the most promising and frequently studied [139]. A two-year placebo-controlled RCT investigating donepezil administered as an adjunct to antidepressants (escitalopram or duloxetine) reported improved global cognition (visuospatial functioning, language processing, executive functioning, delayed memory and processing speed) after one year in older adults with remitted MDD (N = 130); however, these effects did not persist at year two [140]. Similarly, in a pilot placebo-controlled RCT, donepezil administered as an adjunct to open-label antidepressant therapy improved verbal episodic memory in older adults with MDD (N = 12), although there was no effect on executive functioning or attention [141]. In contrast, another placebo-controlled RCT [142] showed that 16-weeks of donepezil administered as an adjunct to citalopram or venlafaxine did not improve cognitive function. These conflicting results may possibly be explained by the measures of cognition used in each study; cognitive improvements were observed following donepezil pharmacotherapy (i.e. [140, 141]) in studies in which batteries of standardised neuropsychological tests not specific to neurological disease were employed (e.g. WAIS-R). In contrast, studies in which no effects were observed (i.e. [142]) used the Alzheimer’s Disease Assessment Scale-Cognitive Subscale [143], which may not be sufficiently sensitive to changes in cognitive function in depressed patients and healthy volunteers [144].
Although donepezil appears promising as a potential cognitive ameliorating agent for MDD, it is important to note that no studies have yet investigated the effects of donepezil on cognitive functioning in younger adults with MDD. Moreover, the cognitive profile of donepezil in healthy volunteer studies is inconclusive; when acutely administered in healthy adults, donepezil improved cognitive function in two studies [145, 146], while it impaired cognition in two further studies [147, 148].
Administration of galantamine, another cholinesterase inhibitor, as an adjunct to antidepressants was shown to have no effect on cognitive function or mood symptoms in older adults with MDD (N = 38) in a placebo-controlled RCT [149]. Consistent with this, galantamine monotherapy did not change cognitive function or mood symptoms in adults with partially remitted MDD in another placebo-controlled RCT [143], although this study had a small sample size (N = 19).
Although galantamine and donepezil are both cholinesterase inhibitors [150], they have divergent secondary mechanisms of action which may explain differences in their cognitive profiles; in particular, donepezil but not galantamine is a potent agonist of sigma-1 receptors (σ1R) [151]. σ1R agonism is associated with promotion of neuroplastic and neuroprotective processes [152, 153], in addition to amplifying signal transduction across glutaminergic and dopaminergic pathways [143, 154, 155].
Beyond primary neurotransmission – novel clinical targets
Recently, novel approaches to the pharmacological targeting of cognitive impairment have emerged. The proposition that cognitive impairment in MDD may be the result of progressive neurotoxic and neuroinflammatory processes, as well as volumetric reductions in neuroanatomical areas such as the hippocampus, striatum, and fronto-cingulate cortices [126, 156,157,158,159,160,161], suggests the modulation of neurosteroid, neurotrophin and pro-inflammatory cytokine activity might be useful targets for treatment development [126, 162,163,164,165].
Neurosteroid dysregulation is suggested to play a role in the pathophysiology of stress, neuroinflammation, and depression [165,166,167,168,169,170]; thus pharmacologically targeting neurosteroid dysregulation may be a useful approach for the treatment of depression and cognitive impairment. In particular, excitatory neurosteroids such as dehydroepiandrosterone and pregnenolone sulphate modulate the function of glutamatergic signalling pathways, thus promoting long-term potentiation [171,172,173]. Consistent with this idea, dehydroepiandrosterone administration was shown to improve verbal memory function in older adults with MDD in a small (N = 6) proof-of-concept study [174, 175]. Two Cochrane systematic reviews concluded there is inadequate evidence supporting a positive effect of dehydroepiandrosterone on cognitive function in healthy older adults and those presenting with age-related cognitive decline [176, 177]. However, a more recent small-scale placebo-controlled study in healthy young males (N = 24) showed dehydroepiandrosterone administration improved verbal episodic memory via cortisol inhibition [178].
Modulation of the σ1R ligands is another potential target for the treatment of cognitive impairment in MDD [179]. Fluvoxamine, an SSRI with high-affinity σ1R agonist properties [180], has been shown to be associated with improvements in the Wechsler Adult Intelligence Scale (WAIS-R) and DSST. However, the effects of fluvoxamine on cognition have not yet been tested against a placebo control; in a double-blind RCT [182], the effects of fluvoxamine were compared with the tetracyclic antidepressant mianserin which is known to have cognition-impairing effects [183]. In another, [184], cognitive improvements were observed only in treatment responders, suggesting a potential confounding effect of symptomatic improvement.
The cognitive effects of σ1R agonists such as fluvoxamine and donepezil are difficult to separate from their serotonergic and cholinergic properties, respectively. Studies using comparator agents such as sertraline and galantamine may further elucidate these effects [179], controlling for potential affective changes associated with neurosteroid modulation [185].
Stimulation of mineralocorticoid receptors via fludrocortisone may indirectly influence cognition [186]. In healthy volunteers (n = 24) and depressed adults (n = 24), verbal memory and executive functioning improved after fludrocortisone administration, with improved verbal memory associated with cortisol inhibition [187]. However, in older adults with MDD (N = 23), a similar experimental paradigm resulted in impairments of psychomotor speed, verbal learning and memory, and executive functioning [188].
Melatonin, when administered as an adjunct to buspirone, was associated with decreased self-reported cognitive impairment in antidepressant non-responders, indicating a potential pro-cognitive effect that is independent of pseudo-specific effects (N = 113) [189]. In multiple studies of healthy individuals, melatonin improved cognitive ability [190], although it is unclear if these cognitive gains might be due to improved sleep.
Erythropoietin improved verbal memory compared with placebo in individuals with TRD following 8 weeks administration (N = 40) [191]. In an additional study, individuals with MDD (n = 36) showed broad improvements in cognitive functioning (including memory, learning and executive functioning) and self-reports of cognitive function following 8 weeks of erythropoietin versus placebo [192]. In healthy volunteers, erythropoietin produced broad enhancements in executive function, memory and hippocampal long-term potentiation [193,194,195]. While promising, the exact mechanisms for cognitive change remain unclear; it has been posited these findings are a result of upregulated stromal cell-derived factor 1 and BDNF [126, 196], however, down-regulation of plasma BDNF following 8 weeks of erythropoietin administration in TRD has been reported independently [197].
The methyl donor, S-Adenosylmethionine, given as monotherapy for MDD resulted in similar depressive symptom reductions to escitalopram in two double-blind RCTs (N = 130; N = 189) [198, 199]. Antidepressant non-responders (N = 46) showed improved self-report of cognitive function following 6 weeks of adjunct S-Adenosylmethionine treatment [200, 201]. Recent metabolomic investigations highlighted the potential of exogenous S-Adenosylmethionine to upregulate toxic metabolite adenine, hindering the clinical practicality of this agent [202].
Taken together, although many of the novel pharmacotherapeutic targets of cognitive impairment in MDD reviewed here appear promising, vigorous independent replication is required to fully elucidate their clinical potential.
Methodological challenges
In reviewing this literature, numerous methodological challenges are apparent in establishing a strong evidence base to support pharmacological targets for the treatment of cognitive impairment in depression.
Pseudo-specificity
A fundamental challenge in establishing evidence of therapeutic validity for drugs which target cognitive function is to identify effects that are primarily mediated by changes in affect (pseudo-specificity). McIntyre et al. [203] posits this can be achieved where depressive symptomatology is appropriately adjusted for, using path analysis and subgroup analysis. Many RCTs have since employed this approach (e.g., [47, 105, 106, 204]), although much of the literature reviewed here has not adopted this methodology. It is also important to consider the influence of other affective domains beyond core depression symptoms, such as motivation, alertness/fatigue, and anxiety, as these may all have an indirect effect on cognitive task performance [205,206,207,208,209].
Inconsistency of cognitive effects across clinical and non-clinical populations
A phenomenon commonly emerging in the reviewed literature is that pharmacological agents often lack shared and domain-specific cognitive effects between individuals with MDD and healthy controls. For example, buspirone and bupropion have both been shown to have cognitive-enhancing effects in patients with MDD [53, 78] but not in healthy volunteers [54, 79, 80]. In contrast, modafinil and citicoline broadly improved cognition in neurological and nonclinical populations, but showed limited or no change in MDD [81, 89, 210]. Furthermore, fludrocortisone resulted in cognitive improvement young adults with MDD but impaired cognitive function in older adults with MDD [187, 188].
One explanation for these differences between patient and healthy control studies is that pharmacologically-induced improvements in cognition may only be seen in those with cognition-related pathophysiological abnormalities, such as progressive neurotoxicity and reduced neurogenesis [126, 211]. For example, reduced grey and white matter integrity in frontal-limbic networks are both associated with cognitive impairment in MDD [212,213,214,215] and reduced neurotrophin and proinflammatory cytokine activity in MDD [216,217,218,219]. Indeed, baseline BDNF, including mature BDNF, and pro-inflammatory cytokine levels in individuals with MDD predicts cognitive improvement and antidepressant effects across a range of agents, including sertraline and vortioxetine [220,221,222,223], although it is important to note that peripheral measures of BDNF may not reflect central BDNF concentration [224]. Further, age and adjunctive therapy may influence antidepressant pharmacodynamics, where the former might explain the inefficacy of cholinergic agents for cognitive impairment in young adults compared with older adults [225]. To better understand pharmacologically-induced cognitive effects across specific populations, the identification of shared and independent treatment-response biomarkers would be beneficial [226, 227]. In particular, if early treatment-induced changes in such biomarkers (e.g. changes in the function of relevant neurocircuitry) were predictive of subsequent efficacy in treating cognitive symptoms, they would lend valuable support to drug development decision-making in this field.
An alternative explanation for inconsistent effects across healthy volunteer and patient samples is that the cognitive tasks used in many studies have insufficient sensitivity to detect pharmacologically-induced cognitive changes in healthy volunteers. Healthy volunteer studies often include high-functioning individuals who perform at ceiling on many standard neuropsychological tasks, thus limiting the detection of pharmacologically induced changes [228, 229]. The use of implicit, automatic measures of cognition may be potentially useful for increasing the sensitivity of pharmacologically-induced cognitive effects in healthy volunteers [77, 228].
Heterogeneity of cognitive impairment in MDD
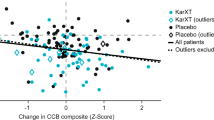
Cognitive impairment in depression is heterogeneous in presentation, due to the pathophysiology of depression itself and external factors such as effects of medication [230]; impairments in specific domains of cognitive function such as memory, executive function and learning differ case-by-case [231, 232]. In future, a better understanding of the specific effects of pharmacological agents on different cognitive domains, when given alone or as an adjunct to antidepressant treatment, may facilitate the more targeted and personalised treatment of cognitive impairment in depression (Fig. 1). It will also be important to define the conditions necessary for successful clinical use of these agents, and where their clinical practicality lies; in particular, whether these agents are best used as preventative therapy, or as treatment for impaired cognitive function during active MDD episodes, or for residual cognitive impairments in remitted MDD.
Efforts to account for the heterogeneity of premorbid intelligence quotients between intervention groups have been made (e.g. [106]), making use of reliable [233] measures of reading and vocabulary, including the National Adult Reading Test; however, as Douglas et al. [234] note, these measures may not generalise to broad metrics of memory, learning and executive function used within studies. A potential solution is subgroup analysis of patient clusters based on cognitive presentations (e.g. working memory impaired vs. intact), although this requires large samples for sufficient power; alternatively, future studies could restrict study inclusion to participants with particular cognitive presentations that align with a priori hypotheses about the cognitive effects of the drug within MDD.
Discrepancies in cognitive outcome measurement
There is considerable heterogeneity in how cognition is measured within the reviewed literature, with both objective neuropsychological measures and subjective self-report of the cognitive function used as outcome measures. Importantly, objective and self-report measures are not reliably correlated [235, 236]. While self-report measures may highlight cognitive deficits which are more meaningful to the individual with depression, they may be confounded by emotional state. Lower self-reported cognitive ability is known to be associated with higher depressive symptomatology [237], which may be the result of negative biases in appraisals of cognitive ability. Our consultations with individuals with lived experience of MDD highlighted the need for person-centred neuropsychological assessments, which focus on the specific cognitive impairments the individual describes affecting their lives. Given the benefits objective and subjective measures of cognition independently offer, both approaches should be used in future research investigating pro-cognitive efficacy of candidate compounds.
Conclusions
Developing better treatments for cognitive impairment is an area of clinical priority in depression, underscored by accounts from individuals with lived experience of depression (Box 3). Throughout this review, we highlight pharmacological agents which hold promise (Table 1), including vortioxetine, modafinil and donepezil. These agents have complex mechanisms of action, and it is unclear whether cognitive change is mediated through primary neurotransmission or through indirect and/or intracellular processes. Better characterisation and consolidation of shared mechanisms between these agents may facilitate future drug discovery and development in this area [238]. There are novel agents such as fludrocortisone and erythropoietin which act on promising mechanistic targets beyond primary neurotransmission; the evidence is however preliminary, requiring further replication. Beyond this, the present review has highlighted multiple methodological challenges of human clinical research in this area (see Table 2), including pseudo-specificity and the selection of sensitive outcome measures.
While the present review is limited in scope to MDD, cognitive deficits in neuropsychiatric populations may be considered transdiagnostically [239], and as such it is worth considering the generalisability of clinical pharmacological evidence beyond MDD. In addition, this review has focussed on non-affective cognitive function, although there are many aspects of affective cognition that are known to play a core role role in depression, such as rumination and emotion regulation [240]. Given the association between impaired executive functioning and increased rumination [241] and reduced cognitive reappraisals [242], future research may consider if these aspects of psychopathology are influenced by drugs which improve cognitive function in depression.
Beyond those reviewed here, there are many further novel promising targets for improving cognitive impairment in MDD where placebo-controlled RCTs have yet to demonstrate cognitive improvement in MDD, or the agents have not yet crossed the preclinical threshold, including creatine, α2-adrenergic receptor antagonists, glucagon-like peptide-1 agonists, GABAB receptor agonists, 5-HT1A biased agonists, and histamine H3 receptor antagonists. With continued efforts in this space, and by adopting robust and consistent methodological approaches across the translational pipeline, there is real promise that the treatment of cognitive impairment in depression may be improved in the future.
References
Roiser JP, Elliott R, Sahakian BJ. Cognitive Mechanisms of Treatment in Depression. Neuropsychopharmacology 2012;37:117–36.
Marazziti D, Consoli G, Picchetti M, Carlini M, Faravelli L. Cognitive impairment in major depression. Eur J Pharm. 2010;626:83–86.
Zaremba D, Schulze Kalthoff I, Förster K, Redlich R, Grotegerd D, Leehr EJ, et al. The effects of processing speed on memory impairment in patients with major depressive disorder. Prog Neuro-Psychopharmacol Biol Psychiatry. 2019;92:494–500.
Conradi HJ, Ormel J, De Jonge P. Presence of individual (residual) symptoms during depressive episodes and periods of remission: a 3-year prospective study. Psychol Med. 2011;41:1165.
Perini G, Cotta Ramusino M, Sinforiani E, Bernini S, Petrachi R, Costa A. Cognitive impairment in depression: recent advances and novel treatments. Neuropsychiatr Dis Treat. 2019;15:1249–58.
Miskowiak KW, Petersen CS. Neuronal underpinnings of cognitive impairment and - improvement in mood disorders. CNS Spectr. 2019;24:30–53.
Czerwińska A, Pawłowski T. Cognitive dysfunctions in depression–significance, description and treatment prospects. Psychiatr Pol. 2020;54:453–66.
Knight MJ, Air T, Baune BT. The role of cognitive impairment in psychosocial functioning in remitted depression. J Affect Disord. 2018;235:129–34.
Koenig AM, Bhalla RK, Butters MA. Cognitive functioning and late-life depression. J Int Neuropsychol Soc Jins 2014;20:461.
Knight MJ, Lyrtzis E, Baune BT. The association of cognitive deficits with mental and physical Quality of Life in Major Depressive Disorder. Compr Psychiatry. 2020;97:152147.
Naismith SL, Longley WA, Scott EM, Hickie IB. Disability in major depression related to self-rated and objectively-measured cognitive deficits: a preliminary study. BMC Psychiatry. 2007;7:32.
Lam RW, Kennedy SH, Mclntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. 2014;59:649–54.
The National Institute for Health and Care Excellence. Depression in adults: recognition and management. Clinical guideline [CG90]. 2009. https://www.nice.org.uk/guidance/cg90. Accessed 4 February 2021.
Qaseem A, Barry MJ, Kansagara D. Nonpharmacologic Versus Pharmacologic Treatment of Adult Patients With Major Depressive Disorder: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2016;164:350–9.
Schneider F, Härter M, Schorr S S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression. Springer-Verlag; 2017.
Hollon SD, Shelton RC. Treatment guidelines for major depressive disorder. Behav Ther. 2001;32:235–58.
Cohen N, Margulies DS, Ashkenazi S, Schaefer A, Taubert M, Henik A, et al. Using executive control training to suppress amygdala reactivity to aversive information. Neuroimage 2016;125:1022–31.
Calkins AW, McMorran KE, Siegle GJ, Otto MW. The effects of computerized cognitive control training on community adults with depressed mood. Behav Cogn Psychother. 2015;43:578–89.
Hallford DJ, Austin DW, Takano K, Fuller-Tyszkiewicz M, Raes F. Computerized Memory Specificity Training (c-MeST) for major depression: A randomised controlled trial. Behav Res Ther. 2021;136:103783.
Brunoni AR, Tortella G, Benseñor IM, Lotufo PA, Carvalho AF, Fregni F. Cognitive effects of transcranial direct current stimulation in depression: results from the SELECT-TDCS trial and insights for further clinical trials. J Affect Disord. 2016;202:46–52.
Baune BT, Renger L. Pharmacological and non-pharmacological interventions to improve cognitive dysfunction and functional ability in clinical depression – A systematic review. Psychiatry Res. 2014;219:25–50.
Keefe RSE, McClintock SM, Roth RM, Doraiswamy PM, Tiger S, Madhoo M. Cognitive effects of pharmacotherapy for major depressive disorder: a systematic review. J Clin Psychiatry. 2014;75:0.
Prado CE, Watt S, Crowe SF. A meta-analysis of the effects of antidepressants on cognitive functioning in depressed and non-depressed samples. Neuropsychol Rev. 2018;28:32–72.
Stahl SM. Modes and nodes explain the mechanism of action of vortioxetine, a multimodal agent (MMA): modifying serotonin’s downstream effects on glutamate and GABA (gamma amino butyric acid) release. CNS Spectr. 2015;20:331–6.
Cutuli D, De Bartolo P, Caporali P, Tartaglione AM, Oddi D, D’Amato FR, et al. Neuroprotective effects of donepezil against cholinergic depletion. Alzheimers Res Ther. 2013;5:1–18.
Rosenblat JD, Kakar R, McIntyre RS. The Cognitive Effects of Antidepressants in Major Depressive Disorder: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int J Neuropsychopharmacol. 2016;19:pyv082.
Shilyansky C, Williams LM, Gyurak A, Harris A, Usherwood T, Etkin A. Effect of antidepressant treatment on cognitive impairments associated with depression: a randomised longitudinal study. Lancet Psychiatry. 2016;3:425–35.
Lahr D, Beblo T, Hartje W. Cognitive performance and subjective complaints before and after remission of major depression. Cogn Neuropsychiatry. 2007;12:25–45.
Hasselbalch BJ, Knorr U, Kessing LV. Cognitive impairment in the remitted state of unipolar depressive disorder: a systematic review. J Affect Disord. 2011;134:20–31.
Organization WH ICD-10: international statistical classification of diseases and related health problems: tenth revision. 1994.
Association AP Diagnostic and statistical manual of mental disorders: DSM-5TM, 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013.
Beck AT, Steer RA, Brown GK Beck depression inventory (BDI-II). vol. 10. Pearson; 1996.
Bech P, Rasmussen N-A, Olsen LR, Noerholm V, Abildgaard W. The sensitivity and specificity of the Major Depression Inventory, using the Present State Examination as the index of diagnostic validity. J Affect Disord. 2001;66:159–64.
Kroenke K, Spitzer RL, Williams JBW. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Ilieva IP, Farah MJ. Enhancement stimulants: perceived motivational and cognitive advantages. Front Neurosci. 2013;7:198.
Miskowiak KW, Burdick KE, Martinez‐Aran A, Bonnin CM, Bowie CR, Carvalho AF, et al. Methodological recommendations for cognition trials in bipolar disorder by the International Society for Bipolar Disorders Targeting Cognition Task Force. Bipolar Disord. 2017;19:614–26.
de Cates AN, Wright LC, Martens MAG, Gibson D, Türkmen C, Filippini N, et al. Déjà-vu? Neural and behavioural effects of the 5-HT4 receptor agonist, prucalopride, in a hippocampal-dependent memory task. Transl Psychiatry. 2021;11:1–9.
Parker J Brintellix® (Vortioxetine) - Psychopharmacologic Drugs Advisory Committee. Maryland; 2016.
Sanchez C, Asin KE, Artigas F. Vortioxetine, a novel antidepressant with multimodal activity: Review of preclinical and clinical data. Pharm Ther. 2015;145:43–57.
Pehrson A, Li Y, Sanchez C, Gulinello M. Vortioxetine Improves Mood and Cognitive Function in Animal Models of Psychiatric Disease: Relevance of 5-HT3 Receptor-Mediated Regulation of GABA and Glutamate Neurotransmission. Biol Psychiatry. 2021;89:S26.
Frampton JE. Vortioxetine: A Review in Cognitive Dysfunction in Depression. Drugs 2016;76:1675–82.
McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17:1557–67.
McIntyre RS, Florea I, Tonnoir B, Loft H, Lam RW, Christensen MC. Efficacy of vortioxetine on cognitive functioning in working patients with major depressive disorder. J Clin Psychiatry. 2017;78:0.
Jaeger J. Digit Symbol Substitution Test: The Case for Sensitivity Over Specificity in Neuropsychological Testing. J Clin Psychopharmacol. 2018;38:513–9.
Smith D, Dempster C, Glanville J, Freemantle N, Anderson I. Efficacy and tolerability of venlafaxine compared with selective serotonin reuptake inhibitors and other antidepressants: A meta-analysis. Br J Psychiatry. 2002;180:396–404.
Theunissen EL, Street D, Højer A-M, Vermeeren A, van Oers A, Ramaekers JG. A Randomized Trial on the Acute and Steady-State Effects of a New Antidepressant, Vortioxetine (Lu AA21004), on Actual Driving and Cognition. Clin Pharm Ther. 2013;93:493–501.
McIntyre RS, Harrison J, Loft H, Jacobson W, Olsen CK. The Effects of Vortioxetine on Cognitive Function in Patients with Major Depressive Disorder: A Meta-Analysis of Three Randomized Controlled Trials. Int J Neuropsychopharmacol. 2016;19:pyw055.
Svanborg P, Åsberg M. A comparison between the Beck Depression Inventory (BDI) and the self-rating version of the Montgomery Åsberg Depression Rating Scale (MADRS). J Affect Disord. 2001;64:203–16.
Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practiceand problems. Stat Med. 2002;21:2917–30.
Treadway MT, Bossaller NA, Shelton RC, Zald DH. Effort-based decision-making in major depressive disorder: a translational model of motivational anhedonia. J Abnorm Psychol. 2012;121:553.
Ravizza SM, Delgado MR. Motivational enhancement of cognitive control depends on depressive symptoms. Emotion 2014;14:646–50.
Cao B, Park C, Subramaniapillai M, Lee Y, Iacobucci M, Mansur RB, et al. The efficacy of vortioxetine on anhedonia in patients with major depressive disorder. Front Psychiatry. 2019;10:17.
Shin C, Ko Y-H, Shim S-H, Kim JS, Na K-S, Hahn S-W, et al. Efficacy of Buspirone Augmentation of Escitalopram in Patients with Major Depressive Disorder with and without Atypical Features: A Randomized, 8 Week, Multicenter, Open-Label Clinical Trial. Psychiatry Investig. 2020;17:796–803.
Chamberlain SR, Müller U, Deakin JB, Corlett PR, Dowson J, Cardinal RN, et al. Lack of deleterious effects of buspirone on cognition in healthy male volunteers. J Psychopharmacol. 2007;21:210–5.
Bantick RA, Rabiner EA, Hirani E, de Vries MH, Hume SP, Grasby PM. Occupancy of agonist drugs at the 5-HT 1A receptor. Neuropsychopharmacology 2004;29:847–59.
Chen H, Lin Q, Lin T, Lin Y, Lin X, Chen R, et al. A controlled study of the efficacy and safety of tandospirone citrate combined with escitalopram in the treatment of vascular depression: A pilot randomized controlled trial at a single-center in China. J Psychiatr Res. 2019;114:133–40.
Yasuno F, Suhara T, Nakayama T, Ichimiya T, Okubo Y, Takano A, et al. Inhibitory Effect of Hippocampal 5-HT1A Receptors on Human Explicit Memory. Am J Psychiatry. 2003;160:334–40.
Loane C, Politis M. Buspirone: What is it all about? Brain Res. 2012;1461:111–8.
Murphy SE, De Cates AN, Gillespie AL, Godlewska BR, Scaife JC, Wright LC, et al. Translating the promise of 5HT4 receptor agonists for the treatment of depression. Psychol Med. 2021;51:1111–20.
Benhamú B, Martín-Fontecha M, Vázquez-Villa H, Pardo L, López-Rodríguez ML. Serotonin 5-HT6 receptor antagonists for the treatment of cognitive deficiency in Alzheimer’s disease. J Med Chem. 2014;57:7160–81.
Okubo R, Hasegawa T, Fukuyama K, Shiroyama T, Okada M. Current limitations and candidate potential of 5-ht7 receptor antagonism in psychiatric pharmacotherapy. Front Psychiatry. 2021;12:161.
King MV, Marsden CA, Fone KCF. A role for the 5-HT1A, 5-HT4 and 5-HT6 receptors in learning and memory. Trends Pharm Sci. 2008;29:482–92.
Upton N, Chuang TT, Hunter AJ, Virley DJ. 5-HT6 Receptor Antagonists as Novel Cognitive Enhancing Agents for Alzheimer’s Disease. Neurotherapeutics 2008;5:458–69.
Stiedl O, Pappa E, Konradsson-Geuken Å, Ögren SO. The role of the serotonin receptor subtypes 5-HT1A and 5-HT7 and its interaction in emotional learning and memory. Front Pharm. 2015;6:162.
Nikiforuk A, Popik P. Amisulpride promotes cognitive flexibility in rats: The role of 5-HT7 receptors. Behav Brain Res. 2013;248:136–40.
Cifariello A, Pompili A, Gasbarri A. 5-HT7 receptors in the modulation of cognitive processes. Behav Brain Res. 2008;195:171–9.
Solas M, Van Dam D, Janssens J, Ocariz U, Vermeiren Y, De Deyn PP, et al. 5-HT7 receptors in Alzheimer’s disease. Neurochem Int. 2021;150:105185.
Codony X, Vela JM, Ramírez MJ. 5-HT6 receptor and cognition. Curr Opin Pharm. 2011;11:94–100.
Meffre J, Chaumont‐Dubel S, Mannoury la Cour C, Loiseau F, Watson DJG, Dekeyne A, et al. 5‐HT6 receptor recruitment of mTOR as a mechanism for perturbed cognition in schizophrenia. EMBO Mol Med. 2012;4:1043–56.
Holenz J, Pauwels PJ, Díaz JL, Mercè R, Codony X, Buschmann H. Medicinal chemistry strategies to 5-HT6 receptor ligands as potential cognitive enhancers and antiobesity agents. Drug Disco Today. 2006;11:283–99.
Khoury R, Grysman N, Gold J, Patel K, Grossberg GT. The role of 5 HT6-receptor antagonists in Alzheimer’s disease: an update. Expert Opin Investig Drugs. 2018;27:523–33.
Shafiei G, Zeighami Y, Clark CA, Coull JT, Nagano-Saito A, Leyton M, et al. Dopamine Signaling Modulates the Stability and Integration of Intrinsic Brain Networks. Cereb Cortex. 2019;29:397–409.
Klostermann EC, Braskie MN, Landau SM, O’Neil JP, Jagust WJ. Dopamine and frontostriatal networks in cognitive aging. Neurobiol Aging. 2012;33:623.e15–623.e24.
Schneider JS, Marshall CA, Keibel L, Snyder NW, Hill MP, Brotchie JM, et al. A novel dopamine D3R agonist SK609 with norepinephrine transporter inhibition promotes improvement in cognitive task performance in rodent and non-human primate models of Parkinson’s disease. Exp Neurol. 2021;335:113514.
Cools R. The costs and benefits of brain dopamine for cognitive control. Wiley Interdiscip Rev Cogn Sci. 2016;7:317–29.
Lövdén M, Karalija N, Andersson M, Wåhlin A, Axelsson J, Köhncke Y, et al. Latent-Profile Analysis Reveals Behavioral and Brain Correlates of Dopamine-Cognition Associations. Cereb Cortex. 2018;28:3894–907.
Klinge C, Shuttleworth C, Muglia P, Nobre AC, Harmer CJ, Murphy SE. Methylphenidate enhances implicit learning in healthy adults. J Psychopharmacol. 2018;32:70–80.
Herrera-Guzmán I, Gudayol-Ferré E, Lira-Mandujano J, Herrera-Abarca J, Herrera-Guzmán D, Montoya-Pérez K, et al. Cognitive predictors of treatment response to bupropion and cognitive effects of bupropion in patients with major depressive disorder. Psychiatry Res. 2008;160:72–82.
Soczynska JK, Ravindran LN, Styra R, McIntyre RS, Cyriac A, Manierka MS, et al. The effect of bupropion XL and escitalopram on memory and functional outcomes in adults with major depressive disorder: Results from a randomized controlled trial. Psychiatry Res. 2014;220:245–50.
Siepmann M, Werner K, Schindler C, Oertel R, Kirch W. The effects of bupropion on cognitive functions in healthy subjects. Psychopharmacol (Berl). 2005;182:597–8.
DeBattista C, Lembke A, Solvason HB, Ghebremichael R, Poirier J. A prospective trial of modafinil as an adjunctive treatment of major depression. J Clin Psychopharmacol. 2004;24:87–90.
Kaser M, Deakin JB, Michael A, Zapata C, Bansal R, Ryan D, et al. Modafinil Improves Episodic Memory and Working Memory Cognition in Patients With Remitted Depression: A Double-Blind, Randomized, Placebo-Controlled Study. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:115–22.
Battleday RM, Brem A-K. Modafinil for cognitive neuroenhancement in healthy non-sleep-deprived subjects: A systematic review. Eur Neuropsychopharmacol. 2015;25:1865–81.
Turner DC, Robbins TW, Clark L, Aron AR, Dowson J, Sahakian BJ. Cognitive enhancing effects of modafinil in healthy volunteers. Psychopharmacol (Berl). 2003;165:260–9.
Baranski JV, Pigeau R, Dinich P, Jacobs I. Effects of modafinil on cognitive and meta-cognitive performance. Hum Psychopharmacol Clin Exp. 2004;19:323–32.
Kelley AM, Webb CM, Athy JR, Ley S, Gaydos S. Cognition enhancement by modafinil: a meta-analysis. Aviat Space Environ Med. 2012;83:685–90.
Meyer JH, Goulding VS, Wilson AA, Hussey D, Christensen BK, Houle S. Bupropion occupancy of the dopamine transporter is low during clinical treatment. Psychopharmacol (Berl). 2002;163:102–5.
Schmitt KC, Reith MEA. The atypical stimulant and nootropic modafinil interacts with the dopamine transporter in a different manner than classical cocaine-like inhibitors. PLoS One. 2011;6:e25790.
Gerrard P, Malcolm R. Mechanisms of modafinil: A review of current research. Neuropsychiatr Dis Treat. 2007;3:349–64.
Tafseer S, Gupta R, Ahmad R, Jain S, Bhatia MS, Gupta LK. Bupropion monotherapy alters neurotrophic and inflammatory markers in patients of major depressive disorder. Pharm Biochem Behav. 2021;200:173073.
Costa R, Oliveira NG, Dinis-Oliveira RJ. Pharmacokinetic and pharmacodynamic of bupropion: integrative overview of relevant clinical and forensic aspects. Drug Metab Rev. 2019;51:293–313.
Rahn AK, Slusher SB, Kaplin IA. Glutamate in CNS neurodegeneration and cognition and its regulation by GCPII inhibition. Curr Med Chem. 2012;19:1335–45.
Volk L, Chiu S-L, Sharma K, Huganir RL. Glutamate synapses in human cognitive disorders. Annu Rev Neurosci. 2015;38:127–49.
Duman RS, Li N, Liu R-J, Duric V, Aghajanian G. Signaling pathways underlying the rapid antidepressant actions of ketamine. Neuropharmacology 2012;62:35–41.
Fava M, Freeman MP, Flynn M, Judge H, Hoeppner BB, Cusin C, et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). Mol Psychiatry. 2020;25:1592–603.
Vidal S, Gex-Fabry M, Bancila V, Michalopoulos G, Warrot D, Jermann F, et al. Efficacy and safety of a rapid intravenous injection of ketamine 0.5 mg/kg in treatment-resistant major depression: an open 4-week longitudinal study. J Clin Psychopharmacol. 2018;38:590–7.
Gill H, Gill B, Rodrigues NB, Lipsitz O, Rosenblat JD, El-Halabi S, et al. The Effects of Ketamine on Cognition in Treatment-Resistant Depression: A Systematic Review and Priority Avenues for Future Research. Neurosci Biobehav Rev. 2021;120:78–85.
Shiroma PR, Albott CS, Johns B, Thuras P, Wels J, Lim KO. Neurocognitive performance and serial intravenous subanesthetic ketamine in treatment-resistant depression. Int J Neuropsychopharmacol. 2014;17:1805–13.
Stippl A, Scheidegger M, Aust S, Herrera A, Bajbouj M, Gärtner M, et al. Ketamine specifically reduces cognitive symptoms in depressed patients: An investigation of associated neural activation patterns. J Psychiatr Res. 2021;136:402–08.
Zhang MWB, Ho R. Controversies of the effect of ketamine on cognition. Front Psychiatry. 2016;7:47.
Lee Y, Syeda K, Maruschak NA, Cha DS, Mansur RB, Wium-Andersen IK, et al. A new perspective on the anti-suicide effects with ketamine treatment: a procognitive effect. J Clin Psychopharmacol. 2016;36:50–56.
Abdallah CG, Averill LA, Gueorguieva R, Goktas S, Purohit P, Ranganathan M, et al. Modulation of the antidepressant effects of ketamine by the mTORC1 inhibitor rapamycin. Neuropsychopharmacology 2020;45:990–7.
Chen M-H, Lin W-C, Wu H-J, Cheng C-M, Li C-T, Hong C-J, et al. Antisuicidal effect, BDNF Val66Met polymorphism, and low-dose ketamine infusion: Reanalysis of adjunctive ketamine study of Taiwanese patients with treatment-resistant depression (AKSTP-TRD). J Affect Disord. 2019;251:162–9.
Abdallah CG, Sanacora G, Duman RS, Krystal JH. The neurobiology of depression, ketamine and rapid-acting antidepressants: Is it glutamate inhibition or activation? Pharm Ther. 2018;190:148–58.
Shiroma PR, Thuras P, Wels J, Albott CS, Erbes C, Tye S, et al. Neurocognitive performance of repeated versus single intravenous subanesthetic ketamine in treatment resistant depression. J Affect Disord. 2020;277:470–7.
Murrough JW, Burdick KE, Levitch CF, Perez AM, Brallier JW, Chang LC, et al. Neurocognitive Effects of Ketamine and Association with Antidepressant Response in Individuals with Treatment-Resistant Depression: A Randomized Controlled Trial. Neuropsychopharmacology 2015;40:1084–90.
Liu W, Zhou Y, Zheng W, Wang C, Zhan Y, Lan X, et al. Repeated intravenous infusions of ketamine: Neurocognition in patients with anxious and nonanxious treatment-resistant depression. J Affect Disord. 2019;259:1–6.
McIntyre RS, Rosenblat JD, Rodrigues NB, Lipsitz O, Chen-Li D, Lee JG, et al. The effect of intravenous ketamine on cognitive functions in adults with treatment-resistant major depressive or bipolar disorders: Results from the Canadian rapid treatment center of excellence (CRTCE). Psychiatry Res. 2021;302:113993.
Chen M-H, Li C-T, Lin W-C, Hong C-J, Tu P-C, Bai Y-M, et al. Cognitive function of patients with treatment-resistant depression after a single low dose of ketamine infusion. J Affect Disord. 2018;241:1–7.
Davis MT, DellaGiogia N, Maruff P, Pietrzak RH, Esterlis I. Acute cognitive effects of single-dose intravenous ketamine in major depressive and posttraumatic stress disorder. Transl Psychiatry. 2021;11:205.
Malhotra AK, Pinals DA, Weingartner H, Sirocco K, David Missar C, Pickar D, et al. NMDA receptor function and human cognition: The effects of ketamine in healthy volunteers. Neuropsychopharmacology 1996;14:301–7.
Harborne GC, Watson FL, Healy DT, Groves L. The effects of sub-anaesthetic doses of ketamine on memory, cognitive performance and subjective experience in healthy volunteers. J Psychopharmacol. 1996;10:134–40.
Morgan CJA, Mofeez A, Brandner B, Bromley L, Curran HV. Acute Effects of Ketamine on Memory Systems and Psychotic Symptoms in Healthy Volunteers. Neuropsychopharmacology 2004;29:208–18.
Hetem LAB, Danion JM, Diemunsch P, Brandt C. Effect of a subanesthetic dose of ketamine on memory and conscious awareness in healthy volunteers. Psychopharmacol (Berl). 2000;152:283–8.
Morgan CJA, Mofeez A, Brandner B, Bromley L, Curran HV. Ketamine impairs response inhibition and is positively reinforcing in healthy volunteers: a dose–response study. Psychopharmacol (Berl). 2004;172:298–308.
Mkrtchian A, Evans JW, Kraus C, Yuan P, Kadriu B, Nugent AC, et al. Ketamine modulates fronto-striatal circuitry in depressed and healthy individuals. Mol Psychiatry. 2020. 2020. https://doi.org/10.1038/s41380-020-00878-1.
Sakurai H, Dording C, Yeung A, Foster S, Jain F, Chang T, et al. Longer-term open-label study of adjunctive riluzole in treatment-resistant depression. J Affect Disord. 2019;258:102–8.
Mathew SJ, Gueorguieva R, Brandt C, Fava M, Sanacora G. A Randomized, Double-Blind, Placebo-Controlled, Sequential Parallel Comparison Design Trial of Adjunctive Riluzole for Treatment-Resistant Major Depressive Disorder. Neuropsychopharmacology 2017;42:2567–74.
Lavretsky H, Laird KT, Krause-Sorio B, Heimberg BF, Yeargin J, Grzenda A, et al. A Randomized Double-Blind Placebo-Controlled Trial of Combined Escitalopram and Memantine for Older Adults With Major Depression and Subjective Memory Complaints. Am J Geriatr Psychiatry. 2020;28:178–90.
Lenze EJ, Skidmore ER, Begley AE, Newcomer JW, Butters MA, Whyte EM. Memantine for late‐life depression and apathy after a disabling medical event: a 12‐week, double‐blind placebo‐controlled pilot study. Int J Geriatr Psychiatry. 2012;27:974–80.
Kishi T, Matsunaga S, Iwata N. A meta-analysis of memantine for depression. J Alzheimer’s Dis. 2017;57:113–21.
Muhonen LH, Lönnqvist J, Juva K, Alho H. Double-blind, randomized comparison of memantine and escitalopram for the treatment of major depressive disorder comorbid with alcohol dependence. J Clin Psychiatry. 2008;69:0.
Nations KR, Dogterom P, Bursi R, Schipper J, Greenwald S, Zraket D, et al. Examination of Org 26576, an AMPA receptor positive allosteric modulator, in patients diagnosed with major depressive disorder: an exploratory, randomized, double-blind, placebo-controlled trial. J Psychopharmacol. 2012;26:1525–39.
Jaso BA, Niciu MJ, Iadarola ND, Lally N, Richards EM, Park M, et al. Therapeutic Modulation of Glutamate Receptors in Major Depressive Disorder. Curr Neuropharmacol. 2017;15:57–70.
Wezenberg E, Verkes RJ, Ruigt GSF, Hulstijn W, Sabbe BGC. Acute effects of the ampakine farampator on memory and information processing in healthy elderly volunteers. Neuropsychopharmacology 2007;32:1272–83.
Carvalho FA, Miskowiak KK, Hyphantis NT, Kohler AC, Alves SG, Bortolato B. et al. Cognitive dysfunction in depression–pathophysiology and novel targets. CNS Neurol Disord Targets (Formerly Curr Drug Targets-CNS Neurol Disord. 2014;13:1819–35..
Xia Q, Wang H, Yin H, Yang Z. Excessive corticosterone induces excitotoxicity of hippocampal neurons and sensitivity of potassium channels via insulin-signaling pathway. Metab Brain Dis. 2019;34:119–28.
Sagara Y, Schubert D. The activation of metabotropic glutamate receptors protects nerve cells from oxidative stress. J Neurosci. 1998;18:6662–71.
Qunies AM, Emmitte KA. Negative allosteric modulators of group II metabotropic glutamate receptors: A patent review (2015 – present). Expert Opin Ther Pat. 2021;31:687–708.
Umbricht D, Niggli M, Sanwald-Ducray P, Deptula D, Moore R, Grünbauer W, et al. Randomized, double-blind, placebo-controlled trial of the mGlu2/3 negative allosteric modulator decoglurant in partially refractory major depressive disorder. J Clin Psychiatry. 2020;81:0.
Gualtieri F, Manetti D, Romanelli M, Ghelardini C. Design and study of piracetam-like nootropics, controversial members of the problematic class of cognition-enhancing drugs. Curr Pharm Des. 2002;8:125–38.
Bentley P, Driver J, Dolan RJ. Cholinergic modulation of cognition: insights from human pharmacological functional neuroimaging. Prog Neurobiol. 2011;94:360–88.
Conant R, Schauss AG. Therapeutic applications of citicoline for stroke and cognitive dysfunction in the elderly: a review of the literature. Alter Med Rev. 2004;9:17–31.
Colucci L, Bosco M, Rosario Ziello A, Rea R, Amenta F, Fasanaro AM. Effectiveness of nootropic drugs with cholinergic activity in treatment of cognitive deficit: a review. J Exp Pharm. 2012;4:163–72.
Fioravanti M, Yanagi M. Cytidinediphosphocholine (CDP‐choline) for cognitive and behavioural disturbances associated with chronic cerebral disorders in the elderly. Cochrane Database Syst Rev. 2005;2004:CD000269.
Secades JJ, Alvarez-Sabín J, Castillo J, Díez-Tejedor E, Martínez-Vila E, Ríos J, et al. Citicoline for Acute Ischemic Stroke: A Systematic Review and Formal Meta-analysis of Randomized, Double-Blind, and Placebo-Controlled Trials. J Stroke Cerebrovasc Dis. 2016;25:1984–96.
Meshkini A, Meshkini M, Sadeghi-Bazargani H. Citicoline for traumatic brain injury: a systematic review & meta-analysis. J Inj Violence Res. 2017;9:41.
Fitzgerald PJ, Hale PJ, Ghimire A, Watson BO. Repurposing Cholinesterase Inhibitors as Antidepressants? Dose and Stress-Sensitivity May Be Critical to Opening Possibilities. Front Behav Neurosci. 2021;14:620119.
Burt T. Donepezil and related cholinesterase inhibitors as mood and behavioral controlling agents. Curr Psychiatry Rep. 2000;2:473–8.
Reynolds CF III, Butters MA, Lopez O, Pollock BG, Dew MA, Mulsant BH, et al. Maintenance Treatment of Depression in Old Age: A Randomized, Double-blind, Placebo-Controlled Evaluation of the Efficacy and Safety of Donepezil Combined With Antidepressant Pharmacotherapy. Arch Gen Psychiatry. 2011;68:51–60.
Pelton GH, Harper OL, Tabert MH, Sackeim HA, Scarmeas N, Roose SP, et al. Randomized double-blind placebo-controlled donepezil augmentation in antidepressant-treated elderly patients with depression and cognitive impairment: a pilot study. Int J Geriatr Psychiatry. 2008;23:670–6.
Devanand DP, Pelton GH, D’Antonio K, Ciarleglio A, Scodes J, Andrews H, et al. Donepezil Treatment in Patients With Depression and Cognitive Impairment on Stable Antidepressant Treatment: A Randomized Controlled Trial. Am J Geriatr Psychiatry. 2018;26:1050–60.
Mohs RC. The Alzheimer’s disease assessment scale: an instrument for assessing treatment efficacy. Psychopharmacol Bull. 1983;19:448–50.
Karin A, Hannesdottir K, Jaeger J, Annas P, Segerdahl M, Karlsson P, et al. Psychometric evaluation of ADAS‐C og and NTB for measuring drug response. Acta Neurol Scand. 2014;129:114–22.
FitzGerald DB, Crucian GP, Mielke JB, Shenal BV, Burks D, Womack KB, et al. Effects of donepezil on verbal memory after semantic processing in healthy older adults. Cogn Behav Neurol. 2008;21:57–64.
Zaninotto ALC, Bueno OFA, Pradella‐Hallinan M, Tufik S, Rusted J, Stough C, et al. Acute cognitive effects of donepezil in young, healthy volunteers. Hum Psychopharmacol Clin Exp. 2009;24:453–64.
Beglinger LJ, Gaydos BL, Kareken DA, Tangphao-Daniels O, Siemers ER, Mohs RC. Neuropsychological test performance in healthy volunteers before and after donepezil administration. J Psychopharmacol. 2004;18:102–8.
Beglinger LJ, Tangphao-Daniels O, Kareken DA, Zhang L, Mohs R, Siemers ER. Neuropsychological test performance in healthy elderly volunteers before and after donepezil administration: a randomized, controlled study. J Clin Psychopharmacol. 2005;25:159–65.
Holtzheimer PE III, Meeks TW, Kelley ME, Mufti M, Young R, McWhorter K, et al. A double blind, placebo‐controlled pilot study of galantamine augmentation of antidepressant treatment in older adults with major depression. Int J Geriatr Psychiatry A J Psychiatry Late Life Allied Sci. 2008;23:625–31.
Pepeu G, Giovannini MG. Cholinesterase inhibitors and beyond. Curr Alzheimer Res. 2009;6:86–96.
Maurice T, Su T-P. The pharmacology of sigma-1 receptors. Pharm Ther. 2009;124:195–206.
Maurice T, Grégoire C, Espallergues J. Neuro (active) steroids actions at the neuromodulatory sigma1 (σ1) receptor: biochemical and physiological evidences, consequences in neuroprotection. Pharm Biochem Behav. 2006;84:581–97.
Ryskamp DA, Korban S, Zhemkov V, Kraskovskaya N, Bezprozvanny I. Neuronal sigma-1 receptors: signaling functions and protective roles in neurodegenerative diseases. Front Neurosci. 2019;13:862.
Sambo DO, Lebowitz JJ, Khoshbouei H. The sigma-1 receptor as a regulator of dopamine neurotransmission: a potential therapeutic target for methamphetamine addiction. Pharm Ther. 2018;186:152–67.
Su T-P, Hayashi T. Understanding the molecular mechanism of sigma-1 receptors: towards a hypothesis that sigma-1 receptors are intracellular amplifiers for signal transduction. Curr Med Chem. 2003;10:2073–80.
Almeida OP, Burton EJ, Ferrier N, McKeith IG, O’Brien JT. Depression with late onset is associated with right frontal lobe atrophy. Psychol Med. 2003;33:675–81.
Sapolsky RM. The possibility of neurotoxicity in the hippocampus in major depression: a primer on neuron death. Biol Psychiatry. 2000;48:755–65.
Sapolsky RM. Glucocorticoids and hippocampal atrophy in neuropsychiatric disorders. Arch Gen Psychiatry. 2000;57:925–35.
Sheline YI. 3D MRI studies of neuroanatomic changes in unipolar major depression: the role of stress and medical comorbidity. Biol Psychiatry. 2000;48:791–800.
Sheline YI, Wang PW, Gado MH, Csernansky JG, Vannier MW. Hippocampal atrophy in recurrent major depression. Proc Natl Acad Sci. 1996;93:3908–13.
Sheline YI, Gado MH, Price JL. Amygdala core nuclei volumes are decreased in recurrent major depression. Neuroreport 1998;9:2023–8.
Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10:1089–93.
de Miranda AS, de Barros JLVM, Teixeira AL. Is neurotrophin-3 (NT-3): a potential therapeutic target for depression and anxiety? Expert Opin Ther Targets. 2020;24:1225–38.
O’Brien SM, Scott LV, Dinan TG. Cytokines: abnormalities in major depression and implications for pharmacological treatment. Hum Psychopharmacol Clin Exp. 2004;19:397–403.
Zorumski CF, Paul SM, Izumi Y, Covey DF, Mennerick S. Neurosteroids, stress and depression: potential therapeutic opportunities. Neurosci Biobehav Rev. 2013;37:109–22.
Almeida FB, Barros HMT, Pinna G. Neurosteroids and Neurotrophic Factors: What Is Their Promise as Biomarkers for Major Depression and PTSD? Int J Mol Sci. 2021;22:1758.
Andrews P, Kornstein S, Halberstadt L, Gardner C, Neale MC. Blue again: perturbational effects of antidepressants suggest monoaminergic homeostasis in major depression. Front Psychol. 2011;2:159.
Morilak DA, Frazer A. Antidepressants and brain monoaminergic systems: a dimensional approach to understanding their behavioural effects in depression and anxiety disorders. Int J Neuropsychopharmacol. 2004;7:193–218.
Murugan S, Jakka P, Namani S, Mujumdar V, Radhakrishnan G. The neurosteroid pregnenolone promotes degradation of key proteins in the innate immune signaling to suppress inflammation. J Biol Chem. 2019;294:4596–607.
Prins J, Olivier B, Korte SM. Triple reuptake inhibitors for treating subtypes of major depressive disorder: the monoamine hypothesis revisited. Expert Opin Investig Drugs. 2011;20:1107–30.
Chen L, Dai X-N, Sokabe M. Chronic administration of dehydroepiandrosterone sulfate (DHEAS) primes for facilitated induction of long-term potentiation via sigma 1 (σ1) receptor: optical imaging study in rat hippocampal slices. Neuropharmacology 2006;50:380–92.
Wang Z-M, Qi Y-J, Wu P-Y, Zhu Y, Dong Y-L, Cheng Z-X, et al. Neuroactive steroid pregnenolone sulphate inhibits long-term potentiation via activation of α2-adrenoreceptors at excitatory synapses in rat medial prefrontal cortex. Int J Neuropsychopharmacol. 2008;11:611–24.
Sabeti J, Nelson TE, Purdy RH, Gruol DL. Steroid pregnenolone sulfate enhances NMDA‐receptor‐independent long‐term potentiation at hippocampal CA1 synapses: Role for L‐type calcium channels and sigma‐receptors. Hippocampus 2007;17:349–69.
Wolkowitz OM, Reus VI, Roberts E, Manfredi F, Chan T, Raum WJ, et al. Dehydroepiandrosterone (DHEA) treatment of depression. Biol Psychiatry. 1997;41:311–8.
Wolkowitz OM, Reus VI, Roberts E, Manfredi F, Chan T, Ormiston S, et al. Antidepressant and cognition‐enhancing effects of DHEA in major depression. Ann N. Y Acad Sci. 1995;774:337–9.
Evans JG, Malouf R, Huppert FAH, Van Niekerk JK. Dehydroepiandrosterone (DHEA) supplementation for cognitive function in healthy elderly people. Cochrane Database Syst Rev. 2006;2006:CD006221.
Huppert FAH, Van Niekerk J. Dehydroepiandrosterone (DHEA) supplementation for cognitive function. Cochrane Database Syst Rev. 2001:CD000304.
Alhaj HA, Massey AE, McAllister-Williams RH. Effects of DHEA administration on episodic memory, cortisol and mood in healthy young men: a double-blind, placebo-controlled study. Psychopharmacol (Berl). 2006;188:541–51.
Hindmarch I, Hashimoto K. Cognition and depression: the effects of fluvoxamine, a sigma-1 receptor agonist, reconsidered. Hum Psychopharmacol. 2010;25:193–200.
Ishikawa M, Ishiwata K, Ishii K, Kimura Y, Sakata M, Naganawa M, et al. High occupancy of sigma-1 receptors in the human brain after single oral administration of fluvoxamine: a positron emission tomography study using [11C] SA4503. Biol Psychiatry. 2007;62:878–83.
la Pia S, Giorgio D, Ciriello R, Sannino A. Double blind controlled study to evaluate the effectiveness and tolerability of fluoxetine versus mianserin in the treatment of depressive disorders among the elderly and their effects on cognitive-behavioral parameters. N. Trends Exp Clin Psychiatry. 1992;8:139–46. al et
Perez A, Ashford JJ. A double-blind, randomized comparison of fluvoxamine with mianserin in depressive illness. Curr Med Res Opin. 1990;12:234–41.
Curran HV, Shine P, Lader M. Effects of repeated doses of fluvoxamine, mianserin and placebo on memory and measures of sedation. Psychopharmacol (Berl). 1986;89:360–3.
Mandelli L, Serretti A, Colombo C, Florita M, Santoro A, Rossini D, et al. Improvement of cognitive functioning in mood disorder patients with depressive symptomatic recovery during treatment: an exploratory analysis. Psychiatry Clin Neurosci. 2006;60:598–604.
Frye CA, Lacey EH. The Neurosteroids DHEA and DHEAS May Influence Cognitive Performance by Altering Affective State. Physiol Behav. 1999;66:85–92.
Wingenfeld K, Otte C. Mineralocorticoid receptor function and cognition in health and disease. Psychoneuroendocrinology 2019;105:25–35.
Otte C, Wingenfeld K, Kuehl LK, Kaczmarczyk M, Richter S, Quante A, et al. Mineralocorticoid Receptor Stimulation Improves Cognitive Function and Decreases Cortisol Secretion in Depressed Patients and Healthy Individuals. Neuropsychopharmacology 2015;40:386–93.
Otte C, Wingenfeld K, Kuehl LK, Richter S, Regen F, Piber D, et al. Cognitive function in older adults with major depression: Effects of mineralocorticoid receptor stimulation. J Psychiatr Res. 2015;69:120–5.
Targum SD, Wedel PC, Fava M. Changes in cognitive symptoms after a buspirone–melatonin combination treatment for Major Depressive Disorder. J Psychiatr Res. 2015;68:392–6.
Obayashi K, Saeki K, Iwamoto J, Tone N, Tanaka K, Kataoka H, et al. Physiological levels of melatonin relate to cognitive function and depressive symptoms: the HEIJO-KYO cohort. J Clin Endocrinol Metab. 2015;100:3090–6.
Miskowiak KW, Vinberg M, Christensen EM, Bukh JD, Harmer CJ, Ehrenreich H, et al. Recombinant Human Erythropoietin for Treating Treatment-Resistant Depression: A Double-Blind, Randomized, Placebo-Controlled Phase 2 Trial. Neuropsychopharmacology 2014;39:1399–408.
Ott CV, Vinberg M, Kessing LV, Miskowiak KW. The effect of erythropoietin on cognition in affective disorders – Associations with baseline deficits and change in subjective cognitive complaints. Eur Neuropsychopharmacol. 2016;26:1264–73.
Miskowiak K, Inkster B, O’Sullivan U, Selvaraj S, Goodwin GM, Harmer CJ. Differential effects of erythropoietin on neural and cognitive measures of executive function 3 and 7 days post-administration. Exp Brain Res. 2008;184:313–21.
Miskowiak K, O’Sullivan U, Harmer CJ. Erythropoietin enhances hippocampal response during memory retrieval in humans. J Neurosci. 2007;27:2788–92.
Adamcio B, Sargin D, Stradomska A, Medrihan L, Gertler C, Theis F, et al. Erythropoietin enhances hippocampal long-term potentiation and memory. BMC Biol. 2008;6:1–16.
Said MF, Islam AA, Massi MN, Prihantono. Effect of erythropoietin administration on the expression of brain-derived neurotrophic factor, stromal cell-derived Factor-1, and neuron-specific enolase in traumatic brain injury: A literature review. Ann Med Surg. 2021;69:102666.
Vinberg M, Miskowiak K, Hoejman P, Pedersen M, Kessing LV. The effect of recombinant erythropoietin on plasma brain derived neurotrophic factor levels in patients with affective disorders: a randomised controlled study. PLoS One. 2015;10:e0127629.
Mischoulon D, Price LH, Carpenter LL, Tyrka AR, Papakostas GI, Baer L, et al. A double-blind, randomized, placebo-controlled clinical trial of S-adenosyl-L-methionine (SAMe) versus escitalopram in major depressive disorder. J Clin Psychiatry. 2013;74:0.
Cuomo A, Beccarini Crescenzi B, Bolognesi S, Goracci A, Koukouna D, Rossi R, et al. S-Adenosylmethionine (SAMe) in major depressive disorder (MDD): a clinician-oriented systematic review. Ann Gen Psychiatry. 2020;19:50.
Sachinvala ND, Teramoto N, Stergiou A. Proposed neuroimmune roles of dimethyl fumarate, bupropion, S-adenosylmethionine, and vitamin D3 in affording a chronically Ill patient sustained relief from inflammation and major depression. Brain Sci. 2020;10:600.
Levkovitz Y, Alpert JE, Brintz CE, Mischoulon D, Papakostas GI. Effects of S-adenosylmethionine augmentation of serotonin-reuptake inhibitor antidepressants on cognitive symptoms of major depressive disorder. Eur Psychiatry. 2012;27:518–21.
Fukumoto K, Ito K, Saer B, Taylor G, Ye S, Yamano M, et al. Excess S-adenosylmethionine inhibits methylation via catabolism to adenine. Commun Biol. 2022;5:313.
McIntyre RS, Xiao HX, Syeda K, Vinberg M, Carvalho AF, Mansur RB, et al. The Prevalence, Measurement, and Treatment of the Cognitive Dimension/Domain in Major Depressive Disorder. CNS Drugs. 2015;29:577–89.
Ferguson JM, Wesnes KA, Schwartz GE. Reboxetine versus paroxetine versus placebo: effects on cognitive functioning in depressed patients. Int Clin Psychopharmacol. 2003;18:9–14.
Gong L, He C, Zhang H, Zhang H, Zhang Z, Xie C. Disrupted reward and cognitive control networks contribute to anhedonia in depression. J Psychiatr Res. 2018;103:61–68.
Gottschalk MG, Mortas P, Haman M, Ozcan S, Biemans B, Bahn S. Fluoxetine, not donepezil, reverses anhedonia, cognitive dysfunctions and hippocampal proteome changes during repeated social defeat exposure. Eur Neuropsychopharmacol. 2018;28:195–210.
Killgore WDS Effects of sleep deprivation on cognition. In: Kerkhof GA, Dongen HPA van BT-P in BR, editors. vol. 185, Elsevier; 2010. p. 105–29.
McIntyre RS, Woldeyohannes HO, Soczynska JK, Maruschak NA, Wium-Andersen IK, Vinberg M, et al. Anhedonia and cognitive function in adults with MDD: results from the International Mood Disorders Collaborative Project. CNS Spectr. 2016;21:362–6.
Short MA, Chee MWL. Chapter 3 - Adolescent sleep restriction effects on cognition and mood. In: Van Dongen HPA, Whitney P, Hinson JM, Honn KA, Chee MWLBT-P in BR, editors. Sleep Deprivation Cogn., vol. 246, Elsevier; 2019. p. 55–71.
Secades JJ. Citicoline in the treatment of cognitive impairment. J Neurol Exp Neurosci. 2019;5:14–26.
Tang SW, Helmeste D, Leonard B. Is neurogenesis relevant in depression and in the mechanism of antidepressant drug action? A critical review. World J Biol Psychiatry. 2012;13:402–12.
Alves GS, Karakaya T, Fußer F, Kordulla M, O’Dwyer L, Christl J, et al. Association of microstructural white matter abnormalities with cognitive dysfunction in geriatric patients with major depression. Psychiatry Res Neuroimaging. 2012;203:194–200.
Meinert S, Nowack N, Grotegerd D, Repple J, Winter NR, Abheiden I, et al. Association of brain white matter microstructure with cognitive performance in major depressive disorder and healthy controls: a diffusion-tensor imaging study. Mol Psychiatry. 2021;27:1103–10.
Wagner G, Koch K, Schachtzabel C, Reichenbach JR, Sauer H, Schlösser RGM. Enhanced rostral anterior cingulate cortex activation during cognitive control is related to orbitofrontal volume reduction in unipolar depression. J Psychiatry Neurosci. 2008;33:199–208.
Yamada S, Takahashi S, Ohoshi Y, Ishida T, Tsuji T, Shinosaki K, et al. Widespread white matter microstructural abnormalities and cognitive impairment in schizophrenia, bipolar disorder, and major depressive disorder: Tract-based spatial statistics study. Psychiatry Res Neuroimaging. 2020;298:111045.
Kakeda S, Watanabe K, Nguyen H, Katsuki A, Sugimoto K, Igata N, et al. An independent component analysis reveals brain structural networks related to TNF-α in drug-naïve, first-episode major depressive disorder: a source-based morphometric study. Transl Psychiatry. 2020;10:187.
Lim J, Sohn H, Kwon M-S, Kim B. White Matter Alterations Associated with Pro-inflammatory Cytokines in Patients with Major Depressive Disorder. Clin Psychopharmacol Neurosci. 2021;19:449–58.
Choi S, Han K-M, Won E, Yoon B-J, Lee M-S, Ham B-J. Association of brain-derived neurotrophic factor DNA methylation and reduced white matter integrity in the anterior corona radiata in major depression. J Affect Disord. 2015;172:74–80.
Smagula SF, Lotrich FE, Aizenstein HJ, Diniz BS, Krystek J, Wu GF, et al. Immunological biomarkers associated with brain structure and executive function in late‐life depression: exploratory pilot study. Int J Geriatr Psychiatry. 2017;32:692–9.
Bortolato B, Carvalho AF, Soczynska JK, Perini GI, McIntyre RS. The Involvement of TNF-α in Cognitive Dysfunction Associated with Major Depressive Disorder: An Opportunity for Domain Specific Treatments. Curr Neuropharmacol. 2015;13:558–76.
Mikoteit T, Beck J, Eckert A, Hemmeter U, Brand S, Bischof R, et al. High baseline BDNF serum levels and early psychopathological improvement are predictive of treatment outcome in major depression. Psychopharmacol (Berl). 2014;231:2955–65.
Sagud M, Nikolac Perkovic M, Dvojkovic A, Jaksic N, Vuksan-Cusa B, Zivkovic M, et al. Distinct association of plasma BDNF concentration and cognitive function in depressed patients treated with vortioxetine or escitalopram. Psychopharmacol (Berl). 2021;238:1575–84.
Wagner S, Kayser S, Engelmann J, Schlicht KF, Dreimüller N, Tüscher O, et al. Plasma brain-derived neurotrophic factor (pBDNF) and executive dysfunctions in patients with major depressive disorder. World J Biol Psychiatry. 2019;20:519–30.
Le Nedelec M, Glue P, Winter H, Goulton C, Broughton L, Medlicott N. Acute low-dose ketamine produces a rapid and robust increase in plasma BDNF without altering brain BDNF concentrations. Drug Deliv Transl Res. 2018;8:780–6.
Perucca EBT-IR of N. Age‐Related Changes in Pharmacokinetics: Predictability and Assessment Methods. Neurobiol. Epilepsy Aging, vol. 81, Academic Press; 2007. p. 183–99.
Rosenblat JD, Brietzke E, Mansur RB, Maruschak NA, Lee Y, McIntyre RS. Inflammation as a neurobiological substrate of cognitive impairment in bipolar disorder: Evidence, pathophysiology and treatment implications. J Affect Disord. 2015;188:149–59.
Voegeli G, Cléry-Melin ML, Ramoz N, Gorwood P. Progress in elucidating biomarkers of antidepressant pharmacological treatment response: a systematic review and meta-analysis of the last 15 years. Drugs 2017;77:1967–86.
Pringle A, Browning M, Parsons E, Cowen PJ, Harmer CJ. Early markers of cognitive enhancement: developing an implicit measure of cognitive performance. Psychopharmacol (Berl). 2013;230:631–8.
Husain M, Mehta MA. Cognitive enhancement by drugs in health and disease. Trends Cogn Sci. 2011;15:28–36.
Porter RJ, Bourke C, Gallagher P. Neuropsychological impairment in major depression: its nature, origin and clinical significance. Aust N. Zeal J Psychiatry. 2007;41:115–28.
Zakzanis KK, Leach L, Kaplan E. On the nature and pattern of neurocognitive function in major depressive disorder. Neuropsychiatry, Neuropsychol Behav Neurol. 1998;11:111–9.
Snyder HR. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: a meta-analysis and review. Psychol Bull. 2013;139:81.
Crawford JR, Deary IJ, Starr J, Whalley LJ. The NART as an index of prior intellectual functioning: a retrospective validity study covering a 66-year interval. Psychol Med. 2001;31:451–8.
Douglas KM, Gallagher P, Robinson LJ, Carter JD, McIntosh VVW, Frampton CMA, et al. Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disord. 2018;20:260–74.
Svendsen AM, Kessing LV, Munkholm K, Vinberg M, Miskowiak KW. Is there an association between subjective and objective measures of cognitive function in patients with affective disorders? Nord J Psychiatry. 2012;66:248–53.
Mohn C, Rund BR. Neurocognitive profile in major depressive disorders: relationship to symptom level and subjective memory complaints. BMC Psychiatry. 2016;16:108.
Opdebeeck C. Self-reported memory and depression over time. Int Psychogeriatr. 2020;32:681–3.
Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A, et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Disco. 2019;18:41–58.
Petersen CS, Miskowiak KW. Toward a transdiagnostic neurocircuitry-based biomarker model for pro-cognitive effects: challenges, opportunities, and next steps. CNS Spectr. 2021;26:333–7.
Snyder HR, Miyake A, Hankin BL. Advancing understanding of executive function impairments and psychopathology: bridging the gap between clinical and cognitive approaches. Front Psychol. 2015;6:328.
Zetsche U, D’Avanzato C, Joormann J. Depression and rumination: Relation to components of inhibition. Cogn Emot. 2012;26:758–67.
Quinn ME, Joormann J. Executive control under stress: Relation to reappraisal ability and depressive symptoms. Behav Res Ther. 2020;131:103634.
Greer TL, Sunderajan P, Grannemann BD, Kurian BT, Trivedi MH. Does duloxetine improve cognitive function independently of its antidepressant effect in patients with major depressive disorder and subjective reports of cognitive dysfunction? Depress Res Treat. 2014;2014:627863.
Raskin J, Wiltse CG, Siegal A, Sheikh J, Xu J, Dinkel JJ, et al. Efficacy of duloxetine on cognition, depression, and pain in elderly patients with major depressive disorder: an 8-week, double-blind, placebo-controlled trial. Am J Psychiatry. 2007;164:900–9.
Mahableshwarkar AR, Zajecka J, Jacobson W, Chen Y, Keefe RSE. A Randomized, Placebo-Controlled, Active-Reference, Double-Blind, Flexible-Dose Study of the Efficacy of Vortioxetine on Cognitive Function in Major Depressive Disorder. Neuropsychopharmacology 2015;40:2025–37.
Tian Y, Du J, Spagna A, Mackie M-A, Gu X, Dong Y, et al. Venlafaxine treatment reduces the deficit of executive control of attention in patients with major depressive disorder. Sci Rep. 2016;6:28028.
Acknowledgements
We thank the individuals with lived experience of depression who took the time to offer valuable consultations, providing enlightening insight and direction for this review. We thank Alice Quinton for help facilitating lived experiences consultations. This research was funded by the Medical Research Council and supported by the NIHR Oxford Health Biomedical Research Centre and the NIHR Oxford Cognitive Health Clinical Research Facility. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. CH has received consultancy fees from P1vital Ltd., Janssen Pharmaceuticals, Sage Therapeutics, Pfizer, Zogenix, Compass Pathways, and Lundbeck. SM has received consultancy fees from Zogenix, Sumitomo Dainippon Pharma, P1vital Ltd., UCB Pharma and Janssen Pharmaceuticals. CH and SM hold grant income from Zogenix, UCB Pharma, Syndesi and Janssen Pharmaceuticals. CH and PC hold grant income from a collaborative research project with Pfizer. ALG has received consultancy fees from Zogenix/UCB Pharma. The other authors report no conflicts of interest.
Author information
Authors and Affiliations
Contributions
Author MC conceptualised and drafted the article; all authors contributed to revisions to the paper for critically important intellectual content and approval of the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Colwell, M.J., Tagomori, H., Chapman, S. et al. Pharmacological targeting of cognitive impairment in depression: recent developments and challenges in human clinical research. Transl Psychiatry 12, 484 (2022). https://doi.org/10.1038/s41398-022-02249-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-02249-6
This article is cited by
-
Microstructural brain abnormalities, fatigue, and cognitive dysfunction after mild COVID-19
Scientific Reports (2024)
-
Glucocorticoids and cognitive function: a walkthrough in endogenous and exogenous alterations
Journal of Endocrinological Investigation (2023)
-
The Serotonin 1A (5-HT1A) Receptor as a Pharmacological Target in Depression
CNS Drugs (2023)
-
Altered brain dynamic in major depressive disorder: state and trait features
Translational Psychiatry (2023)