Abstract
The molecular signature underlying autism spectrum disorder remains largely unknown. This study identifies differential expression of mTOR and MAPK pathways in patients affected by mild and severe idiopathic autism. A total of 55 subjects were enrolled, of which 22 were typically developing individuals and 33 were patients aged between 3 and 11 years, with autism spectrum disorder. A detailed history, including physical examination, developmental evaluation, mental health history and autism diagnostic observation schedule were performed for each patient. Components of the mTOR and MAPK signalling pathways were analysed from peripheral blood at the protein level. Patients were then stratified according to their clinical phenotypes, and the molecular profiling was analysed in relation to the degree of autism severity. In this cohort of patients, we identified increased activity of mTOR and the MAPK pathways, key regulators of synaptogenesis and protein synthesis. Specifically, rpS6, p-eIF4E, TSC1 and p-MNK1 expression discriminated patients according to their clinical diagnosis, suggesting that components of protein synthesis signalling pathways might constitute a molecular signature of clinical severity in autism spectrum disorder.
Similar content being viewed by others
Introduction
Autism spectrum disorder (ASD) is characterized by high phenotypic heterogeneity, including deficits in social interaction and communication, as well as repetitive and unusual behaviours1,2. The aetiology of ASD is still largely unknown, although a complex genetic basis is present3. Some insights have been gained through the study of specific genetic disorders, such as fragile X syndrome (FXS) and tuberous sclerosis (TSC), two monogenic disorders characterized by a high incidence of ASD ranging from 25 to 60%4,5,6. FXS, the most common form of inherited intellectual disability, is caused by the loss or mutation of the fragile X mental retardation protein (FMRP)7,8. FMRP regulates several aspects of mRNA metabolism9,10,11. At synapses, FMRP regulates local protein synthesis at different levels9, with one of the characterized mechanisms based on the binding to CYFIP1 (cytoplasmic FMRP interacting protein 1) and eIF4E (eukaryotic translation initiation factor 4E)12,13,14,15. TSC is a dominantly inherited multisystem disorder characterized by the formation of hamartomas in different organs and the brain, caused by mutations in the TSC1 or TSC2 genes encoding hamartin and tuberin, respectively. TSC1 and TSC2 form a biochemical complex that inhibits the mammalian (also named mechanistic) target of rapamycin mTOR signalling pathway16. A large majority (85%) of children and adolescents with TSC display epilepsy, 50% cognitive disorders and ~30–40% ASD16,17.
Several forms of syndromic autism and intellectual disabilities (IDs), including FXS and TSC, are associated with mutations in genes that regulate protein synthesis and affect structure, transmission and plasticity of synapses18. Thus, it has been hypothesized that aberrant synaptic protein synthesis might contribute to ASD and other IDs that share ASD-like clinical features19,20. In the brain, mTOR and MAPK signalling pathways regulate synaptogenesis and local protein synthesis21. The MAPK pathway regulates neural progenitor biogenesis, learning and memory22,23 and mRNA translation, by phosphorylation of TSC2 and eIF4E via MAPK-interacting kinase 1 and 2 (MNK1 and MNK2)14,24. The MAPK pathway is upregulated in patients with syndromic ASD25. Furthermore, the deletion of the 16p11.2 locus, which includes the MAPK3 (mitogen-activated protein kinase 3) gene, is associated with ASD26,27.
The mTOR kinase is part of two functionally distinct biochemical complexes: mechanistic target of rapamycin complex 1 (mTORC1) and mechanistic target of rapamycin complex 2 (mTORC2)24,28. mTORC1 affects protein synthesis by phosphorylation of eukaryotic translation initiation factor 4E-binding protein 1 (eIF4E-BP1) and p70 ribosomal protein S6 kinase (S6K1)21,28. The mTOR pathway is dysregulated in several human diseases, including cancer and diabetes29,30 as well as intellectual disabilities, such as FXS, Rett syndrome and ASD30. Thus, there is a wealth of evidence implicating mTOR and MAPK pathways, and ultimately protein synthesis, in syndromic ASD. Surprisingly, however, less is known about the function of these pathways in idiopathic ASD.
Here, we sought to characterize mTOR and MAPK pathways in children with idiopathic autism who had no other identifiable clinical syndromes. We investigated the expression of the above-described two pathways in peripheral blood mononuclear cells (PBMCs) of children with idiopathic autism and in typically developing individuals (TDI). In addition to performing a global analysis of patients versus TDI, we also analysed the molecular profile according to the clinical severity of ASD to identify a potential molecular signature of the disease severity.
Materials and methods
Subjects
This research was approved by the ethical committee of the University Hospital of Tor Vergata (Rome, Italy) and all participants provided written informed consent. Clinical data were gathered from 33 patients (27 males and 6 females) with idiopathic autism, recruited among those attending the Division of Child Neurology and Psychiatry, University Hospital of Tor Vergata (Rome, Italy). Patients ranged in age from 3 to 11 years, and met clinical criteria for a diagnosis of ASD, based on the diagnostic and statistical manual of mental disorders, fifth edition (DSM5)31. The diagnosis of ASD was also confirmed by using the autism diagnostic observation schedule (ADOS) test. Exclusion criteria included (1) neurodevelopmental disorders of known aetiology (as FXS, TSC, chromosomal abnormalities), (2) significant sensory or motor impairment, (3) significant medical conditions known to affect brain development, (4) low birth weight (< 2200g) or prematurity (<36 week of gestation).
The neuropsychological evaluation of children with ASD, involving development and cognitive assessment, was conducted by means of a diagnostic protocol, which included the administration of (1) the psychoeducational profile third edition (PEP-3)32 to determine the developmental level of young children with autism, (2) Leiter International Performance Scale-Revised (Leiter-R)33 to evaluate non-verbal-cognitive levels and (3) the autism diagnostic observation schedule (ADOS)34 for measuring the severity of autistic symptoms. The patient group was compared with a control group of 22 TDI, children and adolescents, ranging from 3 to 17 years of age (10 males and 12 females), who attended the outpatient clinic of the “Tor Vergata” University Hospital (Rome) for routine visits. The medical history of these children did not report evidence of any neurological or psychiatric disease. All children underwent a medical workup, including neurological examination, awake/sleep EEG, standard genetic analysis and auxological measurements. In addition, medical record examinations and parental interviews about the child history were performed. Consistency was required between parental information and medical records.
PEP-3: a standardised norm‐referenced scale to assess the development of communication and motor skills and the presence of maladaptive behaviours of children suspected of ASD, with a developmental age between 2 and 7 years, who may be non‐verbal, have limited attention skills and poor concentration, and who are not used to a formal testing situation. The PEP-3 does not provide a development quotient (DQ) like PEP-R, obtained by dividing the child’s age-equivalent score by his/her chronological age. We generated the scale by estimating a development level (DL) by the ratio of developmental age/chronological age35 for each developmental subtest.
Leiter-R: expressively non-verbal measure of global intelligence with fair cross-cultural applicability. Its engaging, non-verbal format makes it ideal for use with individuals with ASD. It provides an IQ score, as well as percentile and age-equivalent scores for each subtest. For cases where the IQ score was not possible to evaluate, DL was assessed.
In accordance with a recent study, DLs of each subtest of the PEP-3, can be compared with Leiter-R IQ and can be considered as indicators of cognitive functioning in subjects with ASD36. The decision to administer the PEP-3 or the Leiter-R scale or both, was based on the child’s developmental skills, attention skills and age.
ADOS: a semi-structured assessment of communication, social interaction and relatedness, play, imagination and stereotyped or repetitive behaviours. This measure yields scores in the social domain, communication domain, as well as a combined score. A child can be classified as having autistic disorder, pervasive development disorder not otherwise specified (PDD-NOS), or as non-autistic.
The modules provide social-communicative sequences that combine a series of unstructured and structured situations. The examiner selects the module that is most appropriate for a child on the basis of his/her expressive language level. Module 1 is intended for individuals who do not have verbal language or use just simple words; Module 2 for individuals with some phrase speech who are not verbally fluent; Module 3 for verbally fluent children.
CSS (Calibrated Score System): a standardized severity score based on codes within the domains, that can be calculated to compare autism symptoms across modules37. Based on the CSS, each child was assigned to AUT, for severe symptoms, ASD, for mild symptoms and NS for non-significant symptoms. In our clinical severity analysis, we separated patients into “Mild” and “Severe” groups based on their CSS designation as “ASD” or “AUT”, respectively. The division into groups based on cognitive function was performed using the scores obtained by the cognitive evaluation Leiter-VR or development assessment PEP-3, in accordance with recent data36.
Peripheral blood mononuclear cell (PBMCs) isolation
Blood samples were collected by venepuncture into EDTA-coated tubes. PBMCs were isolated from whole blood (9 ml) using Histopaque-1077 (Sigma-Aldrich) according to manufacturer’s instructions. All samples in this study represent patient peripheral blood mononuclear cells (PBMCs) that were freshly purified after blood collection and not cultured.
Protein extraction and western blotting
Total protein extracts from PBMCs were obtained from the cellular pellet directly in 2X Laemmli Buffer. Samples were boiled and separated by SDS–PAGE electrophoresis and transferred to a PVDF membrane (GE Healthcare). Total and phospho-protein levels were detected simultaneously on the same membranes by using antibodies specific to the desired protein. Membranes were incubated using the following antibodies: rabbit anti-FMRP (1:1000, custom made by 21st Century), mouse anti-mTOR (1:500, CST #4517), rabbit anti-p-mTOR (Ser2448) (1:500, CST #2971), rabbit anti-TSC1 (1:1000, CST #4906), rabbit anti-TSC2 (1:500, CST #4308), rabbit anti-rpS6 (1:1000, CST #2217), rabbit anti-p70S6K1 (1:500, CST #9202), mouse anti-p-p70S6K1 (1:500, CST #9206), mouse anti-eIF4E (1:1000, Santa Cruz #SC-271480), rabbit anti-p-eIF4E (Ser209) (1:500, CST #9741), rabbit anti-4E-BP1 (1:1000, CST #9644), rabbit anti-p-4E-BP1 (Thr37/46) (1:500, CST #2855), rabbit anti-Rheb (1:500, Thermo Fisher #PA5-20129), rabbit anti-MNK1 (1:1000, CST #2195), rabbit anti-p-MNK1 (Thr197/202) (1:500, CST #2111), mouse anti-ERK1-2 (1:1000, Abgent #AM2189B), rabbit anti-p-ERK1-2 (Thr202/Tyr204) (1:500, Santa Cruz #SC-16982), mouse anti-GAPDH (1:2000, Thermo Fisher Scientific #MA5-15738). The following secondary antibodies were used: anti-rabbit or anti-mouse HRP, anti-rabbit or anti-mouse IgG Dylight 800 (1:10000 Promega #W4011, # W402B, and 1:2500, Thermo Fisher Scientific #SA5-35571, #SA5-35521, respectively) and anti-mouse or anti-rabbit IgG Dylight 680 (1:1000, Thermo Fisher Scientific #35518, #35568). Proteins were revealed using an enhanced chemiluminescence kit (Bio-Rad) and the imaging system LAS-4000 mini (GE Healthcare Life Sciences) or, for Dylight-conjugated secondary antibodies, the Odyssey Infrared Imaging System (LI-COR Bioscience). Total and phosphoproteins were revealed using the LI-COR system using differential fluorescently-tagged secondary antibodies to reveal modified and non-modified proteins on the same membrane without any overlap or stripping. All phosphoproteins were normalised relative to the total protein on the same blot. Total proteins were normalised to the average of both Coomassie staining of the membranes (control for total proteins on the membrane) and GAPDH signals. This normalisation is reported in arbitrary units (A.U.) in the figures. ImageQuant TL software was used to quantify the signals. Some antibodies revealed more than one signal for proteins. Specifically, ERK1-2 and p-ERK1-2 were quantified considering the two detected isoforms together. The antibody for rpS6 detected both the manufacturer-specified band at 33 kDa in addition to an unpredicted, non-specific band. In this case, we only quantified the single band at 33 kDa (the upper one) and the non-specific band was not included. The analysis of each protein represents the average of at least two technical replicates per subject.
Statistical analysis
Sample sizes were based on our preliminary results, where we determined the need for a sample size of at least n = 21/group for a power of 85%, alpha = 0.05, and effect size: Hedges' g = 0.67. Randomization of subjects was not possible in this study, as the goal was to compare patients versus controls. Comparisons between patients with ASD and controls were performed using nonparametric Mann–Whitney U test. When more than two groups were compared, analyses were performed using generalized linear models with maximum likelihood estimation followed by post hoc Tukey’s multiple comparison test. InStat statistical software (GraphPad Softwares Inc., La Jolla, CA) was used for the statistical analysis. Canonical discriminant analysis (CDA) was used to investigate whether a set of differentially expressed proteins could discriminate among three groups of patients according to their clinical disease status (controls, mild ASD and severe ASD), using SPSS (IBM Corp. Armonk, NY, US) software, version 24.0. The analysis employed a stepwise technique, based on the Wilks’ ʎ test with the standard probabilities of F (3.84 to enter and 2.71 to be removed) for variable selection, keeping variables with a statistically significant classification performance (p < 0.05) in the model. Cross-validation was performed using a leave-one-out method to assess the model performance.
Significance was denoted as *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Error bars represent the standard error of the mean (SEM). Variances between groups were similar. Outliers were calculated using the Grubbs’ outlier test and were excluded from the figures and the statistical analysis.
Results
Clinical summary
Comprehensive clinical data were gathered from 33 patients with idiopathic autism (Table 1).
At the time of the evaluation, 21 children had acquired verbal language. Of these, 9 children were able to use phrase speech, while the remaining 12 were able to use only simple words. Five children showed comorbid hyperactivity and attention problems, and two children were suffering from celiac disease. All patients had an established diagnosis of ASD at the time of enrolment. For this study, they were re-evaluated for core clinical features of ASD using the ADOS; for developmental skills using standardised scale psychoeducational profile third edition (PEP-3); and for nonverbal-cognitive abilities using the Leiter-R scale. Three patients were unable to complete the neuropsychiatric evaluations (Table 1). Their data were included in the global analyses, but excluded in analyses based on disease severity.
Thirty subjects were evaluated for the presence of ASD symptoms using the ADOS. According to the expressive language level of the child, the examiner selected the most appropriate ADOS module. ADOS-module 1 was used for 22 patients (10 non-verbal children; 12 verbal children whose language was constituted by simple words); ADOS-module 2 (for individuals with some phrase speech not verbally fluent) for two children; ADOS-module 3 (for verbally fluent children) for six patients.
All subjects, except one (ID 15), exceeded cut-off criteria scores for ASD on the ADOS. For each child, a score was calculated according to the Calibrated Score System (CSS), a standardized severity score based on codes within the domains, calculated to compare autism symptoms across ADOS-modules37. Each child was then assessed for cognitive and development. The PEP-3 or the Leiter-R scales or both were applied based on the child’s developmental skills, attention skills and age. Children were grouped according to the scores obtained in the cognitive evaluation Leiter-VR or functional assessment PEP-3, in accordance with recent data36 (Table 1).
Expression of the components of mTOR and MAPK signalling pathways in patients with idiopathic autism
We first performed a global analysis of the expression levels of 17 proteins involved in the mTOR and MAPK pathways in the blood of patients with ASD compared to typically developing controls (Fig. 1 and Supplementary Fig. 1). We targeted proteins with a strong link to local protein synthesis modulation.
a Left, representative Western blot showing protein levels of rpS6, eIF4E and p-eIF4E (Ser209). The molecular weight of each protein is indicated in kDa. Right, bar plots representing the quantification of the technical replicates where rpS6 and p-eIF4E levels are increased in ASD patients compared with controls (rpS6: U = 150, p = 0.03; p-eIF4E: U = 115, p < 0.0001). Error bars represent the standard error of the mean (n = 11-22 CTRL, 26-33 ASD; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001; Mann–Whitney U tests). Each dot represents the average of at least two technical replicates per subject. Total proteins were normalised to the average of Coomassie staining and GAPDH. Phosphoproteins were normalised for respective total protein levels. *indicates the quantified signal b Left, representative Western blot showing protein levels of ERK 1-2, p-ERK 1-2 (Thr202/Tyr204), MNK1 and p-MNK1 (Thr197/202). The molecular weight of each protein is indicated in kDa. Right, bar plots representing the quantification of the technical replicates, where ERK1-2 and p-MNK1 levels are increased in ASD patients compared with controls (ERK1/2: U = 242.5, p = 0.04; p-MNK1: U = 58.5, p = 0.004)
The key effector mTOR did not show any significant differences either in the total level or in the phosphorylation status (Ser2448 site) between ASD patients and controls (Supplementary Fig. 1a). The two downstream mediators of the mTORC1 complex activity, 4E-BP1 and the p70S6K1 kinase, were also similar between groups (Supplementary Fig. 1a,b). Moreover, no differences were observed in the translational repressor FMRP (Supplementary Fig. 1b). Interestingly, the 40S ribosomal subunit component, rpS6, was increased in ASD patients compared to controls (p = 0.03) (Fig. 1a). Moreover, while the translation initiation factor eIF4E did not exhibit differential expression between ASD patients and TDI, its activated phosphorylated form (Ser209) was significantly higher in ASD patients compared to TDI (p < 0.0001) (Fig. 1a).
Since mTORC1 activity and protein synthesis initiation are inhibited by the TSC complexes38, we next investigated if TSC1 and TSC2 levels were dysregulated in ASD patients. However, no differences were observed in TSC1 and TSC2 protein levels (Supplementary Fig. 1c). We also investigated the expression level of RHEB, a protein known to interact and activate mTORC138. RHEB levels also did not differ between ASD patients and TDI (Supplementary Fig. 1c).
ERK1-2 (extracellular signal-regulated kinase 1-2) signalling is also involved in the translational control downstream of the activation of cell surface receptors23,39. The expression of p44/42 MAPK (ERK1-2) was significantly increased in ASD patients compared to controls (p = 0.04), however there were no differences in its phosphorylated status on the Thr202/Tyr204 residues (p-ERK1-2) (Fig. 1b). Interestingly, while the downstream effector of ERK1-2, MNK1, did not show differences between the groups, we observed a significant increase in MNK1 phosphorylation levels (Thr197/202) in ASD patients compared with controls (p = 0.004) (Fig. 1b), suggesting increased activity at the end of this pathway.
Taken together, our findings point to increased activity in mTOR and MAPK pathways in children with idiopathic ASD.
Clinical-molecular correlations
Given the heterogeneity of phenotypes found in autism spectrum disorder, and the variability of protein expression observed within our cohort, we hypothesized that protein expression may change in relation to the severity of the disease. To address this question, we analysed the molecular profile according to the clinical phenotype for each patient. Based on the CSS classification, we identified several of the previously analysed 17 proteins that correlated with the severity of the disease. Among those, p-eIF4E, rpS6 and p-MNK1 proteins, which were increased in the global analysis, exhibited significantly increased levels in the severe group compared with controls (p-eIF4E: p = 0.0003; rpS6: p = 0.03; p-MNK1: p = 0.01; Fig. 2a–c). While ERK1-2 levels were changed in the global analysis, we did not observe any correlation with the severity of ASD. Interestingly, we observed an increase of TSC1 levels in the mild ASD subgroup but not in the severe subgroup (p = 0.048; Fig. 2d).
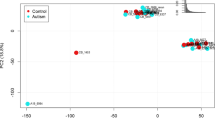
Bar plots representing the quantification of the technical replicates in the three subgroups, CTRL, Mild ASD and Severe ASD show significantly increased levels of a p-eIF4E (F(2,45) = 9.51; p = 0.0004) b rpS6 (F(2,38) = 3.70; p = 0.03) and c p-MNK1 (F(2,29) = 5.02; p = 0.01) in the severe subgroup compared to controls, while d TSC1 levels were significantly increased in the mild group only (F(2,45) = 3.24; p = 0.048). Error bars represent the standard error of the mean (n = 11-21 CTRL, 6-7 Mild ASD, 11-20 Severe ASD; *p < 0.05, **p < 0.01, ***p < 0.001; one-way ANOVA). e Scatter plot of the two canonical functions containing four proteins (p-eIF4E, rpS6, TSC1, p-MNK1) that discriminated subjects according to their severity into three groups: CTRL, mild ASD and severe ASD (Wilks’ Lambda = 0.480; Chi-square = 20.2; df = 8; p = 0.01). The mean discriminant scores for each group are depicted as group centroids. Four patients were not included in this analysis (see Table 1)
Together, these findings suggest that mild and severe autism may be differentiated according to different protein expression profiles.
Finally, as we identified four proteins (p-eIF4E, rpS6, TSC1 and p-MNK1) that demonstrated an association with the clinical severity, we wanted to investigate if, together, those proteins could constitute a molecular signature for autism severity. Therefore, we performed a canonical discriminant analysis between the disease groups and healthy controls. Remarkably, the analysis generated two canonical functions that significantly separated the patient groups with 71.9% accuracy (p = 0.01; Fig. 2e). A cross-validation of the analysis revealed a robust model with 68.8% of cross-validated cases correctly classified. Thus, these four proteins are able to distinguish, with high accuracy, patients with ASD from typically developing controls as well as patients with mild versus severe autistic clinical features.
Discussion
The complexity and heterogeneity of ASD clinical phenotypes makes it difficult to determine the severity of ASD symptomology, predict prognoses and stratify individuals for research purposes40. In this study, we investigated mTOR and MAPK signalling pathways in the peripheral tissue of autism spectrum disorder patients in order to identify a molecular signature both for the disease and for ASD severity. Globally, we found a significant increase of rpS6, p-eIF4E, ERK1-2 and p-MNK1 levels in patients with ASD compared with controls (Fig. 1). Interestingly, we observed a large variability in the protein expression levels of ASD patients compared with typically developing controls that was related to their clinical phenotype. When patients were stratified according to their CSS classification, we found several proteins (p-eIF4E, rpS6, TSC1 and p-MNK1) that appear to constitute a molecular signature of severity. Indeed, a canonical discriminant analysis revealed that p-eIF4E, rpS6, p-MNK1 and TSC1 proteins could discriminate between the three subgroups (controls, mild ASD and severe ASD) (Fig. 2e). We suggest that this set of proteins is a molecular readout, which correlates with ASD severity.
The identified proteins are positive translational regulators, suggesting a peripheral hyperactivation of protein synthesis in autism. Compelling evidence in mice and humans indicates that aberrant synaptic protein synthesis is associated with several forms of neurodevelopmental disorders19,41,42,43. At the molecular level, a dysregulation of MAPK and mTOR pathways has been suggested to disrupt protein synthesis19,20,21,44,45,46. Additionally, a link between two direct regulators of protein synthesis, eIF4E-BPS and S6K1 kinase, in autistic-like phenotypes in mice20 and human cells46,47 was proposed. Moreover, our findings are supported by studies in post-mortem brains and T cells from idiopathic ASD patients, where a hyperactivation of the mTOR pathway was observed47,48.
Functionally, in the brain, mTOR and MAPK are downstream effectors of group I mGluRs, NMDA and TrkB receptors24. MAPKs modulate the activation of MNK1, which phosphorylates eIF4E on serine 20949 and enhances protein synthesis50. Notably, our cohort of ASD patients displayed a significant increase of p-MNK1 and p-eIF4E, both in the global expression and in the clinical correlations (Figs. 1a, b and 2a, c). Surprisingly, the increase in p-MNK1 in ASD patients was not accompanied by an increase in ERK1-2 activation, suggesting that the activation of MNK1 is ERK-independent. MNK1 can also be regulated by the upstream MAP kinase p3851, thus, future studies should examine the possibility for increased activation of this MAP kinase. Furthermore, we analysed the phosphorylation of 4E-BP1 and did not see any significant differences between groups (Supplementary Fig. 1a), suggesting that the upregulation of eIF4E phosphorylation is linked to the MNK axis rather than the mTOR signalling. Ultimately, our findings indicate a hyperactivation of the MAPK pathway leading to hyperphosphorylation of p-eIF4E, which arguably results in aberrant protein synthesis.
Studies in humans and mice indicate that an increased activity of eIF4E leads to ASD and autistic-like phenotypes respectively52–55 eIF4E activity is modulated by the mitogen-activated protein kinase (MAPK)-interacting kinases (MNKs)49. Specifically, MNK1 is required for translational activation in cell migration, cancer metastasis56 and in response to BDNF in the mouse cortical neurons and in the dentate gyrus14,57. Our work here identifies a new role for p-MNK1 in idiopathic ASD, providing further evidence for the contribution of the MAPK pathway to idiopathic ASD58.
Patients affected by FXS and TSC disorders meet the diagnostic criteria of ASD, suggesting that mutations in these pathways may cause ASD21,59. The TSC complex inhibits mTOR activity, leading to translational repression38,60. Tsc1 deletion in neurons has been linked to macrocephaly and embryonic lethality, and Tsc1 models present defects in synaptic plasticity61,62,63. Despite the fact that the small sample size limits interpretations, the observed increase of TSC1 levels may indicate an increased inhibition of protein synthesis in the mild subgroup only. Moreover, these results suggest a possible bidirectional disruption of protein synthesis in ASD. A bidirectional alteration in protein synthesis has been previously proposed in two mouse models for ASD. Fmr1-/y and TSC2+/- mice displayed opposing effects in synaptic protein synthesis that compensate each other in the double mutant Fmr1-/y TSC2+/- mice19. While we observed increased levels of some positive regulators of protein synthesis in the severe subgroup, our data also found an increased level in the negative protein synthesis regulator, TSC1, in the mild ASD group (Fig. 2d). Our study strengthens the bidirectional disruption hypothesis, and indicates that similar mechanisms may occur in humans.
Our findings suggest an overlap in the molecular mechanisms between syndromic and idiopathic ASD. Recently, we demonstrated an increase in protein synthesis levels in non-neuronal cells of individuals with FXS64. As similar findings were obtained in neuronal and non-neuronal cells within the same mouse64, we suggest that peripheral levels of protein synthesis may function as a representative neuronal molecular signature for future clinical trials aiming to restore translational control in FXS and other neurodevelopmental disorders. Interestingly, several studies have explored the use of human peripheral blood cells as a surrogate for the neuronal molecular signature in neurological diseases, suggesting that lymphocytes may constitute an easily accessible “neural probe” to study neuropsychiatric disorders such as autism65,66. Overall, our results suggest that defective protein synthesis may constitute the potential molecular mechanism underlying ASD pathology across different etiologies67.
Our data propose that an increase in both MAPK and mTOR pathways possibly leads to aberrant protein synthesis (Fig. 3) in subjects with ASD, indicating that alteration of mTOR and the MAPK pathways may contribute to intellectual disabilities and to both syndromic and non-syndromic ASD. Although further studies in different cohorts are required, we suggest that measurements of key protein synthesis regulators may constitute a molecular signature in PBMCs that may be predictive for early diagnosis of autism, particularly across severity groups. This may facilitate the identification of suitable targets for future personalised therapies.
p-MNK1, p-eIF4E, TSC1 and rpS6 discriminate mild and severe ASD. Color code indicates different pattern of expression across the two ASD groups. Dark pink denotes upregulated proteins in severe ASD (p-MNK1, p-eIF4E and rpS6). Light pink denotes upregulated TSC1 in mild ASD. The dysregulation of each of those proteins can lead to an excessive protein synthesis
References
Bhat, S., Acharya, U. R., Adeli, H., Bairy, G. M. & Adeli, A. Autism: cause factors, early diagnosis and therapies. Rev. Neurosci. 25, 841–850 (2014).
Volkmar, F. R. & McPartland, J. C. From Kanner to DSM-5: autism as an evolving diagnostic concept. Annu. Rev. Clin. Psychol. 10, 193–212 (2014).
Fakhoury, M. Autistic spectrum disorders: a review of clinical features, theories and diagnosis. Int. J. Dev. Neurosci. 43, 70–77 (2015).
Curatolo, P., Moavero, R. & de Vries, P. J. Neurological and neuropsychiatric aspects of tuberous sclerosis complex. Lancet Neurol. 14, 733–745 (2015).
Wang, L. W., Berry-kravis, E. & Hagerman, R. J. Fragile X: leading the way for targeted treatments in autism. Neurotherapeutics 7, 264–274 (2010).
Kaufmann, W. E. et al. Autism spectrum disorder in fragile X syndrome: cooccurring conditions and current treatment. Pediatrics 139, S194–S206 (2017).
Wang, T., Bray, S. M. & Warren, S. T. New perspectives on the biology of fragile X syndrome. Curr. Opin. Genet. Dev. 22, 256–263 (2012).
Bagni, C. & Oostra, B. A. Fragile X syndrome: from protein function to therapy. Am. J. Med Genet Part A 161, 2809–2821 (2013).
Richter, J. D., Bassell, G. J. & Klann, E. Dysregulation and restoration of translational homeostasis in fragile X syndrome. Nat. Rev. Neurosci. 16, 595–605 (2015).
Pasciuto, E. & Bagni, C. SnapShot: FMRP interacting proteins. Cell 159, 218–218.e1 (2014).
Davis, J. K. & Broadie, K. Multifarious functions of the fragile X mental retardation protein. Trends Genet. 33, 703–714 (2017).
DeRubeis, S. et al. CYFIP1 coordinates mRNA translation and cytoskeleton remodeling to ensure proper dendritic Spine formation. Neuron 79, 1169–1182 (2013).
Napoli, I. et al. The fragile X syndrome protein represses activity-dependent translation through CYFIP1, a new 4E-BP. Cell 134, 1042–1054 (2008).
Panja, D. et al. Two-stage translational control of dentate gyrus LTP consolidation is mediated by sustained BDNF-TrkB signaling to MNK. Cell Rep. 9, 1430–1445 (2014).
Santini, E. et al. Reducing eIF4E-eIF4G interactions restores the balance between protein synthesis and actin dynamics in fragile X syndrome model mice. Sci. Signal. 10, 41–46 (2017).
Curatolo, P., Napolioni, V. & Moavero, R. Autism spectrum disorders in tuberous sclerosis: pathogenetic pathways and implications for treatment. J. Child Neurol. 25, 873–880 (2010).
Curatolo, P. Mechanistic target of rapamycin (mTOR) in tuberous sclerosis complex-associated epilepsy. Pediatr. Neurol. 52, 281–289 (2015).
Zoghbi, H. Y. & Bear, M. F. Synaptic dysfunction in neurodevelopmental intellectual disabilities. Spring 4, 1–22 (2012)..
Auerbach, B. D., Osterweil, E. K. & Bear, M. F. Mutations causing syndromic autism define an axis of synaptic pathophysiology. Nature 480, 63–68 (2011).
Gkogkas, C. G. et al. Autism-related deficits via dysregulated eIF4E-dependent translational control. Nature 493, 371–377 (2012).
Kelleher, R. J. & Bear, M. F. The autistic neuron: troubled translation? Cell 135, 401–406 (2008).
Murphy, L. O. & Blenis, J. MAPK signal specificity: the right place at the right time. Trends Biochem. Sci. 31, 268–275 (2006).
Yang, K. et al. Up-regulation of Ras/Raf/ERK1/2 signaling impairs cultured neuronal cell migration, neurogenesis, synapse formation, and dendritic spine development. Brain. Struct. Funct. 218, 669–682 (2013).
Lipton, J. O. & Sahin, M. The neurology of mTOR. Neuron 84, 275–291 (2014).
Stivaros, S. et al. Randomised controlled trial of simvastatin treatment for autism in young children with neurofibromatosis type 1 (SANTA). Mol. Autism 9, 1–13 (2018).
Kalkman, H. O. Potential opposite roles of the extracellular signal-regulated kinase (ERK) pathway in autism spectrum and bipolar disorders. Neurosci. Biobehav. Rev. 36, 2206–2213 (2012).
Fasano, S. & Brambilla, R. Ras-ERK signaling in behavior: old questions and new perspectives. Front. Behav. Neurosci. 5, 79 (2011).
Laplante, M. & Sabatini, D. M. MTOR signaling in growth control and disease. Cell 149, 274–293 (2012).
Huber, K. M., Klann, E., Costa-Mattioli, M. & Zukin, R. S. Dysregulation of mammalian target of rapamycin signaling in mouse models of autism. J. Neurosci. 35, 13836–13842 (2015).
Crino, P. B. The mTOR signalling cascade: paving new roads to cure neurological disease. Nat Rev Neurol 12, 379–392 (2016).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-5; American Psychiatric Publishing: Washington, DC, USA (2013).
Schopler, E., Lansing, M. D., Reichler, R. J., & Marcus, L. M. Psychoeducational profile: third edition(PEP-3). Austin, TX: Pro-Ed (2004).
Roid GM, Miller LJ. Leiter International Performance Scale-Revised: Examiners Manual. Stoelting Co: Wood Dale, IL (1997).
Lord, C. et al. The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 30, 205–223 (2000).
Fulton, M. L. & D’Entremont, B. Utility of the psychoeducational profile-3 for assessing cognitive and language skills of children with autism spectrum disorders. J. Autism Dev. Disord. 43, 2460–2471 (2013).
De Giacomo A., et al. Can PEP-3 Provide a Cognitive Profile in Children with ASD? A Comparison Between the Developmental Ages of PEP-3 and IQ of Leiter-R. J. Appl. Res. Intellect. Disabil. 8, 337 (2015).
Gotham, K., Pickles, A. & Lord, C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J. Autism Dev. Disord. 39, 693–705 (2009).
Dibble, C. C. & Cantley, L. C. Regulation of mTORC1 by PI3K signaling. Trends Cell Biol. 25, 545–555 (2015).
Kelleher, R. J., Govindarajan, A., Jung, H.-Y., Kang, H. & Tonegawa, S. Translational control by MAPK signaling in long-term synaptic plasticity and memory. Cell 116, 467–479 (2004).
Mehling, M. H. & Tassé, M. J. Severity of autism spectrum disorders: current conceptualization, and transition to DSM-5. J. Autism Dev. Disord 46, 1–17 (2016).
Barnes, S. A. et al. Convergence of hippocampal pathophysiology in Syngap + /- and Fmr1-/y Mice. J. Neurosci. 35, 15073–15081 (2015).
Tao, J. et al. Negative allosteric modulation of mGluR5 partially corrects pathophysiology in a mouse model of Rett syndrome. J. Neurosci. 36, 11946–11958 (2016).
Tian, D. et al. Contribution of mGluR5 to pathophysiology in a mouse model of human chromosome 16p11.2 microdeletion. Nat. Neurosci. 18, 182–184 (2015).
Ehninger, D., Li, W., Fox, K., Stryker, M. P. & Silva, A. J. Reversing neurodevelopmental disorders in adults. Neuron 60, 950–960 (2008).
Costa-Mattioli, M. & Monteggia, L. M. mTOR complexes in neurodevelopmental and neuropsychiatric disorders. Nat. Neurosci. 16, 1537–1543 (2013).
Poopal, A. C., Schroeder, L. M., Horn, P. S., Bassell, G. J. & Gross, C. Increased expression of the PI3K catalytic subunit p110δ underlies elevated S6 phosphorylation and protein synthesis in an individual with autism from a multiplex family. Mol. Autism 7, 3 (2016).
Onore, C., Yang, H., Van de Water, J. & Ashwood, P. Dynamic Akt/mTOR signaling in children with autism spectrum disorder. Front. Pediatr. 5, 1–9 (2017).
Tang, G. et al. Loss of mTOR-dependent macroautophagy causes autistic-like synaptic pruning deficits. Neuron 83, 1131–1143 (2014).
Bramham, C. R., Jensen, K. B. & Proud, C. G. Tuning specific translation in cancer metastasis and synaptic memory: control at the MNK–eIF4E Axis. Trends Biochem. Sci. xx, 1–12 (2016).
Joshi, S. Mnk kinase pathway: cellular functions and biological outcomes. World J. Biol. Chem. 5, 321 (2014).
Waskiewicz, A. J., Flynn, A., Proud, C. G. & Cooper, J. A. Mitogen-activated protein kinases activate the serine/threonine kinaseses Mnk1 and Mnk2. EMBO J. 16, 1909–1920 (1997).
Huynh, T. N. et al. eIF4E/Fmr1 double mutant mice display cognitive impairment in addition to ASD-like behaviors. Neurobiol. Dis. 83, 67–74 (2015).
Santini, E. et al. Exaggerated translation causes synaptic and behavioural aberrations associated with autism. Nature 493, 411–415 (2013).
Neves-Pereira, M. et al. Deregulation of EIF4E: a novel mechanism for autism. J. Med. Genet. 46, 759–765 (2009).
Waltes, R. et al. Common EIF4E variants modulate risk for autism spectrum disorders in the high-functioning range. J. Neural. Transm. (2014).
Bramham, C. R., Jensen, K. B. & Proud, C. G. Tuning specific translation in cancer metastasis and synaptic memory: control at the MNK–eIF4E Axis. Trends Biochem. Sci. 41, 847–858 (2016).
Genheden, M. et al. BDNF stimulation of protein synthesis in cortical neurons requires the MAP kinase-interacting kinase MNK1. J. Neurosci. 35, 972–984 (2015).
Ivanov, H., Stoyanova, V., Popov, N., Bosheva, M. & Vachev, T. Blood-based gene expression in children with autism spectrum disorder. Biodiscovery 17, 2 (2015).
Iossifov, I. et al. The contribution of de novo coding mutations to autism spectrum disorder. Nature 515, 216–221 (2014).
Dibble, C. C. et al. TBC1D7 Is a third subunit of the TSC1-TSC2 complex upstream of mTORC1. Mol. Cell 47, 535–546 (2012).
Ehninger, D. et al. Reversal of learning deficits in a Tsc2 + /- mouse model of tuberous sclerosis. Nat. Med. 14, 843–848 (2008).
Bateup, H. S. et al. Excitatory/inhibitory synaptic imbalance leads to hippocampal hyperexcitability in mouse models of tuberous sclerosis. Neuron 78, 510–522 (2013).
Borrie, S. C., Brems, H., Legius, E. & Bagni, C. Cognitive dysfunctions in intellectual disabilities: the contributions of the Ras-MAPK and PI3K-AKT-mTOR pathways. Annu. Rev. Genom. Hum. Genet. 18, 115–142 (2017).
Jacquemont, S. et al. Protein synthesis levels are increased in a subset of individuals with Fragile X syndrome. Hum. Mol. Genet. 0, 1–13 (2018).
Mohr, S. & Liew, C. C. The peripheral-blood transcriptome: new insights into disease and risk assessment. Trends Mol. Med. 13, 422–432 (2007).
Gladkevich, A., Kauffman, H. F. & Korf, J. Lymphocytes as a neural probe: potential for studying psychiatric disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 28, 559–576 (2004).
Magdalon, J., Sánchez-Sánchez, S., Griesi-Oliveira, K. & Sertié, A. Dysfunctional mTORC1 signaling: a convergent mechanism between syndromic and nonsyndromic forms of autism spectrum disorder? Int. J. Mol. Sci. 18, 659 (2017).
Acknowledgements
We are very thankful to Maria Giulia Farace and Laura D’Andrea for advice and guidance and our laboratory colleagues for discussions and critical reading of the manuscript. We thank the children and families who so generously dedicated their time and effort to this research. This work was supported by the Associazione Italiana Ricerca Neurologia Infantile (AIRNI), Associazione Novartis Italiana Sindrome X Fragile, VIB, Fondazione Cariplo, Telethon GGP15257, Foundation Jérôme Lejeune, NCCR Synapsy (51NF40-158776) and Etat de Vaud. F.H. is a recipient of the Marie Heim-Vögtlin (MHV) fellowship. We thank Annick Crevoisier for her outstanding administrative support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rosina, E., Battan, B., Siracusano, M. et al. Disruption of mTOR and MAPK pathways correlates with severity in idiopathic autism. Transl Psychiatry 9, 50 (2019). https://doi.org/10.1038/s41398-018-0335-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-018-0335-z
This article is cited by
-
Gephyrin phosphorylation facilitates sexually dimorphic development and function of parvalbumin interneurons in the mouse hippocampus
Molecular Psychiatry (2024)
-
Stem Cell Secretions as a Potential Therapeutic Agent for Autism Spectrum Disorder: A Narrative Review
Stem Cell Reviews and Reports (2024)
-
Is tuberous sclerosis complex-associated autism a preventable and treatable disorder?
World Journal of Pediatrics (2024)
-
Recent advances to Neuroprotection: repurposing drugs against neuroinflammatory disorders
Molecular Biology Reports (2023)
-
Neuroprotective Efficacy of Fisetin Against VPA-Induced Autistic Neurobehavioral Alterations by Targeting Dysregulated Redox Homeostasis
Journal of Molecular Neuroscience (2023)