Abstract
Introduction
Spinal cord injury (SCI) is a serious disabling syndrome, and the clinical picture depends on the level and extent of the injury. The International Spinal Cord Society (ISCoS) and the American Spinal Cord Association (ASIA) have developed instruments (Data Sets) to assess the various aspects of the SCI. In 2012, the International SCI Pulmonary Function Basic Data Set was elaborated. It is composed of four questions and spirometry for the collection of lung function basic data.
Objective
The objective was to translate and validate the International SCI Pulmonary Function Basic Data Set to the Portuguese language.
Methods
The entire methodology followed the recommendations of the ISCoS and ASIA. Two translations of the original version into Portuguese were performed, and after consensus among the translators, the Portuguese version was sent for back-translation. After back-translation and comparison with the original version, the final Portuguese version was obtained. For the second phase of the study, 30 SCI individuals were selected. Two interviewers applied the questionnaire in two distinct moments.
Results
All results presented constant, excellent, or perfectly concordant data, except for the third question in the inter-rater comparison, where the Kappa coefficient showed value reasonable in the first interview and good in the second.
Conclusion
The translation into Brazilian Portuguese of the “International SCI Pulmonary Function Basic Data Set” created a valid and highly reliable instrument, like the original without linguistic and cultural disagreements that allow its use in the evaluation of patients with SCI in Brazil.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) affects motricity, sensitivity, the autonomic nervous system, sexual and reproduction function and sphincter control, with repercussions in the psychological, economic, and social sphere [1, 2].
According to the National Spinal Cord Injury Statistical Center data (NSCISC) [3], published in 2020, the incidence of SCI in the United States of America, is 54 cases per million or 17,810 new cases a year. In Brazil, the latest Ministry of Health guideline on SCI (2013) informs that the incidence is 40 cases per million generating 6–8 thousand new cases per year [2].
The SCI affects respiratory, vascular, urinary, intestinal, and musculoskeletal functions, according to the level and extent of the injury. Higher SCI leads to greater functional and physiological impairment and impacts on the individual´s independence, social participation, and quality of life [1]. According to International Spinal Cord Society´s (ISCoS) published data in 2011, 21% of the SCI patients die between the first and tenth year post-injury in Brazil [4]. The pulmonary complications caused by respiratory failure are among the leading causes of morbidity and mortality, especially in the first year after SCI [5, 6].
Better pre-hospital care and life-support have contributed to increasing the survival of SCI patients, even in severe cases with great impairment of respiratory function [6, 7]. This condition may persist, preventing the development of a rehabilitation program and aggravating the disabilities of the patients. The development of respiratory function assessment protocols with basic, reproducible, reliable, and easy-to-apply data is essential for the follow-up of this population, prevention of complications, and evaluation of post-treatment outcomes, in addition to the possibility of comparison with other centers results [8].
In 2002, ISCoS and American Spinal Cord Association (ASIA) developed sets of basic and essential data sets for each diagnostic, clinical and functional aspect affected by SCI, which were comprehensive and universal [8]. The International SCI Pulmonary Function Basic Data Set was created in 2012, to collect a minimum amount of data on the respiratory function in SCI patients. Each variable and category of the International SCI Pulmonary Function Basic Data Set was selected to collect the minimum representative and comparable data [6].
The adequate and universal use of the data sets requires translation and validation to counteract linguistic and cultural differences between countries. ISCoS and ASIA encourage the translation and validation of the data sets in different countries and languages [8, 9].
Objectives
Translate and validate the International SCI Pulmonary Function Basic Data Set to the Portuguese language spoken in Brazil in individuals with SCI.
Methods
Translation and validation of the International SCI Pulmonary Function Basic Data Set were authorized by the ISCoS and ASIA committee and prepared following the methodology recommended [8, 9]. The project was approved by the Ethics and Research Committee of the Associação de Assistência à Criança Deficiente (AACD) under document 2,567,152 and registered in Plataforma Brasil under CAAE number: 49547715.4.0000.0085.
Instrument
The International SCI Pulmonary Function Basic Data Set translated as “Conjunto de Dados Básicos da Função Pulmonar na Lesão da Medula Espinal” is a qualitative and quantitative questionnaire that provides information about the respiratory condition. It is composed of demographic data, SCI date (using the International SCI Core Data Set), and four questions about the current and previous respiratory conditions of the individual and the actual spirometry. four questions are: (I) pulmonary conditions before spinal cord injury; (II) the history of tobacco use; (III) pulmonary conditions and complications in the last year after SCI; (IV) present use of ventilatory assistance. After the questionnaire, patients are submitted to the pulmonary function test (spirometry).
Translation
The International SCI Pulmonary Function Basic Data Set was translated for Portuguese by two physiotherapists, with experience in treating patients with SCI, fluent in English, and aware of the objectives of the study. After the two independent translations, a comparison was made between the two translated versions and the original version. The disagreements were resolved after joint analysis by the two translators and the consensual version was validated by a more experienced professional who had more than 15 years of experience and aware of the project.
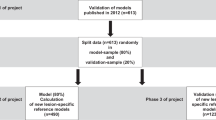
The first version translated and approved in Portuguese was sent to a third translator fluent in English and Portuguese, blind about the original version, who back translated the text into English. After the back translation, the group (two translators and an experienced expert member) compared the back-translated version with the original version. At this stage, if no disagreements were found, the consolidation of the final text in Portuguese was achieved. The final Portuguese version was, then, used in the second phase of the process, the validation (Fig. 1).
Validation
The validation process of the International SCI Pulmonary Function Basic Data Set was made by applying the questionnaire translated into a group of Brazilian SCI individuals.
Participants
We included 30 patients of both genders, residents of São Paulo, belonging to the SCI Clinic of AACD (Ibirapuera unit), who underwent rehabilitation or medical care in the Institution between 2008–2018.
Through telephone contact, patients were informed about the study proposal and in case of acceptance and compliance with the inclusion criteria, were called for an interview, in which they signed the consent form.
Inclusion criteria
-
Age 18 years or older.
-
Diagnosis of spinal cord injury confirmed by clinical examination and imaging tests (Computed Tomography, or Magnetic Resonance Imaging).
-
American Spinal Injury Association Impairment Scale (AIS) A and B.
-
The neurological level was at or above the sixth thoracic level (T6).
-
Individuals able to perform spirometry.
-
No cognitive changes interfere with the questionnaire response.
-
No associated disabling conditions: traumatic brain injury, stroke, neuromuscular diseases, and limb amputations
-
Absence of pregnancy.
Exclusion criteria
-
Unable to contact or refusing to answer the questionnaire in the second evaluation.
Data collection
The questionnaire was applied by two examiners with experience in the treatment of patients with SCI. Each examiner conducted two interviews with the same participant, at two different times, using the same questionnaire (Fig. 2).
-
Time 1 - participant was interviewed by two examiners on the same day, in-person (40 min interval between interviews). After the questionnaire was applied, spirometry was collected: forced vital capacity (FVC), the peak flow of cough (PEF), and the first-minute expiratory volume (FEV1). A Cardinal Health CareFusion Microloop ® spirometer was used, duly calibrated according to the criteria of the American Thoracic Society (ATS) and European Respiratory Society (ERS) [10, 11]. All participants used a nose clip, and the mouth was attached to a mouthpiece to prevent air leakage.
-
Time 2 - (15 days after) - Through a telephone call, the participant was interviewed by the same examiners, respecting the range of 40 min.
In both moments (1 and 2), the answers were given according to the alternatives presented and the researcher marked the answer chosen by the participant.
Statistical analysis
The correlation, reliability, and reproducibility of the study’s qualitative variables were estimated using the Kappa coefficient (κ). The correlation, reliability, and reproducibility of the study’s quantitative variables were estimated using the Intraclass Coefficient Correlation (ICC). As recommended by ISCoS and ASIA [9, 12, 13].
Results
Sample characterization
The mean age was 40.7 ± 10.6 (24–65) years and the time after the SCI ranged from 5 months to 31 years. The other demographic data and on the SCI are seen in Table 1.
Translation
Two divergences were found in the first phase of the instrument’s translation from English to Portuguese in the “History of Tobacco Use” question: translator 1 translated cigars as “charuto” and pipe bowl” as “fornilho de cachimbo” and translator 2 translated cigars as “fumo” and pipe bowl as “cachimbo.” To maintain the construct the group chose “charuto” for cigar and “cachimbo” for pipe bowl.
Validation
Intra and inter-rater assessment
Question 1 - Pulmonary conditions before SCI (collected once) (Table 2).
-
The κ coefficient was not calculated, since all the data were constants.
-
Most patients (96.7%) had no respiratory impairment before the SCI.
Question 2 – Smoking history.
-
The κ coefficient was perfect for raters 1 and 2.
-
70% of participants had never smoked, 16.7% were former smokers, and 13.3% were smokers.
Question 3 - Pulmonary conditions and complications after SCI within the last year.
-
The κ coefficient, in the intra-rater analysis, was excellent for rater 1 and rater 2.
-
The κ coefficient, in the inter-rater analysis, was reasonable at the first assessment and good at the second assessment.
-
83.3% of participants had no pulmonary complications after SCI and 16.7% had pneumonia in the last year.
Question 4 – Current utilization of ventilatory assistance.
-
The κ coefficient was not calculated since the data were constants in all evaluations.
-
100% of the participants do not need any type of ventilatory support.
Spirometry
All variables evaluated spirometry showed ICC values between 0.75 and 1.00. All considered excellent (Table 3).
Discussion
The present study aimed to translate, adapt, and validate the International SCI Pulmonary Function Basic Data Set for the Brazilian spoken Portuguese with an SCI population.
The Data Sets were created by ISCoS and ASIA, the two largest scientific institutions in the area, to improve the quality of data collected by standardizing, simplifying, and structuring the protocols developed. There are currently 25 Data Sets for evaluating different aspects of SCI useful instruments to help in choosing the treatments, collecting data, and improving the care of patients [14].
The translation and validation of the instrument followed the recommendations of ISCoS and ASIA, which helped to prevent any cultural or linguistic deviations in the translation process [9]. A similar methodology was used in the translation and validation process for the Chinese and Spanish languages [15, 16]. The same protocol was used to perform the translation to Portuguese in the International Spinal Cord Injury Quality of Life Data Set, International Spinal Cord Bowel Function, and the International Spinal Cord Injury Lower Urinary Tract Function Data Set [17, 18].
The terms used in the International SCI Pulmonary Function Basic Data Set are, mostly, technical terms, which facilitate the translation. The same facility was referred to in the translation into Chinese and Spanish languages [15, 16]. The translation of the other Data sets, however, may be more difficult, especially in the cultural aspects. During the translation of the International SCI Lower Urinary Tract Function Data Set to Portuguese, the author reported a great number of disagreements, which required more effort from the staff involved for the final version [7]. The translation of the International SCI Quality of Life Data Set for the Chinese language also refers to difficulties on the definition of quality of life across the different countries and cultures, as well as other studies on the same subject [19, 20]. The universally used technical terms facilitate the translation process, as it maintains objectivity with few cultural biases.
Only the item “Smoking history” were seen as translation discrepancies, easily resolved by word choice “charuto” for cigars and “cachimbo” to pipe bowl, terms more used Portuguese language for the types of tobacco consumption, described in the protocol. These choices were approved by the most experienced examiner, who considered that the choice terms are widely used and understood in the Portuguese language spoken in Brazil. In the other stages, there were no differences, allowing to obtain the translated version compatible with the original.
The validation of the instrument was performed by applying the instrument in 30 patients with a high level of SCI with compromised respiratory function. The choice of these patients was deliberate so that the instrument could be evaluated by individuals with some degree of impairment of respiratory function. This choice was different from the one made by the Spanish study, which evaluated a larger sample, 62 patients, but without choosing patients with greater impairment of respiratory function [15].
The instrument’s reliability and agreement were excellent or perfect in most items in the intra-rater (time 1 versus time 2) and inter-rater (same-time comparison) assessments, showing that the instrument has good reliability and reproducibility. Possibly, the main factor of the concordant answers is the characteristics of the International SCI Pulmonary Function Basic Data Set, a protocol with few questions, many of them binary, technical, and objective, which facilitated the translation and validation. The same seems to have happened with the translations to other languages, indeed distinct from other Data sets with more open-ended questions [7, 15, 16, 18]. Important data to be shared with the teams that make the Data sets, so that they are more objective in the elaboration of the questions, avoiding discursive or interpretive answers.
In question 1 “Lung conditions present before SCI”, data were constant in all assessments. The previous pulmonary conditions of the individual can interfere with the performance after SCI since chronic diseases such as asthma and bronchitis can harm lung function. Respondents were able to accurately describe the pre-injury condition, possibly due to the impact of the reported respiratory diseases on health before the SCI. In the current study, 96.7% of the participants had no respiratory disease before the SCI, results like those of the Spanish validation, where 91.9% of the interviewees did not have a respiratory problem before the injury [15].
In question 2, “Smoking history”, the agreement in all evaluations was perfect. Information on smoking habits about the time of use and amounts smoked were very consistent and accurate (κ = 1.00) in both intra- and inter-rater comparisons, with no disagreement. The presence or absence of smoking is a binary and easy reply, and a high rate of language agreement is expected, but the timing and amount could be less accurate, which was not observed, indicating, perhaps, the importance of habit in people. In the present study, 30% of the participants had a history of smoking, where 13.3% were smokers and 16.7% were ex-smokers. This result was different from the Spanish one, where 54.8% of the participants had a history of smoking, with 24.2% smokers and 30.6% ex-smokers [15]. Smoking is a factor in respiratory condition and survival of patients with SCI, as well as the population in general. In a longitudinal study with 430 individuals with SCI, carried out in 2014, it was found that mortality was not associated with pulmonary complications as an independent parameter, but related to the current lifestyle, highlighting smoking and related clinical conditions, such as chronic obstructive pulmonary disease and heart disease [21].
In question 3 “Pulmonary complications and conditions after SCI within the last year” there was the lowest inter-rater agreement. The agreement was reasonable in the first face-to-face evaluation (κ = 0.592) and good in the second evaluation over the telephone (κ = 0.673), showing a degree of disagreement in the answers. It was also lower, albeit with a high index, in the intra-rater evaluation (κ = 0.739 and κ = 0.700), in the same question. The information in question 3 is important, as pulmonary complications are among the main causes of mortality and morbidity, especially in the first year after SCI [3]. The accumulation of secretions, insufficient cough, and the loss of inspiratory muscle strength can aggravate and perpetuate infectious conditions, showing the importance of monitoring the respiratory condition [22, 23]. The lower agreement may be due to the fact that they may have difficulty with recalling the clinical conditions during the first year after SCI. The recent injury, hospitalization, surgery, and all the changes in the patient’s life can disrupt the memory evocative of pulmonary conditions. These may be associated with other changes in the SCI, more marked for the patient in the period, and bring variations in the responses obtained. Patients with chronic SCI may also be confused and not be able to remember with certainty the pulmonary alterations that occurred in the last year. In addition, it should consider the effect of the first questionnaire, which can help in the past data evocation, which was observed in the second interview.
In question 4 “Current utilization of Ventilatory Assistance”, the data were constant in all evaluations, as expected, as it reports on how much ventilation assistance the individual needs to keep the pulmonary function. This condition can change between the hospitalization period and discharge, and it is important in the evaluation of respiratory function. It is a domain with less influence of cultural and linguistic factors, as it is entirely composed of technical terms, and therefore, without disagreeing factors in the answers and the translation of the data set.
In the current study, 100% of the participants reported not using ventilatory assistance, unlike the validation in Spanish, in which 11.3% used some assistance [15]. This data may be related to the fact that individuals in the process or after the rehabilitation period are already clinically stable or to the fact that they are already adapted to the current condition and the real need for the use of ventilatory assistance is not diagnosed. Respiratory changes of sleep are common in individuals with SCI, especially in cervical injuries. They are associated with muscle weakness, areas of hypoventilation, and atelectasis, but are difficult to diagnose in this population. Correcting this dysfunction is essential for maintaining the respiratory condition, health, and quality of life of patients [24].
Spirometry makes up the International SCI Pulmonary Function Basic Data Set and it is the gold standard for assessing lung function and provides the basic data (FVC, PEF, and FEV1) to quantify weaknesses and identify possible causes [6]. In the current study, there was no disagreement with the results found in the two inter-rater assessments carried out at the time of the first interview. All variables showed excellent results concerning the agreement, as measured by the ICC. In the Spanish validation, it was not informed whether spirometry was performed for the second time, nor the ICC values [15], although this information is important to perform a complete validation of the instrument [9]. In the current study, the highest values found were FVC 60.8%, PEF 50.3%, and FEV1 64.6%, whereas in the Spanish study the values found were higher, with FVC 67%, PEF 70%, and FEV1 72% [15], data that are fully understood, since our sample consisted of individuals with lesions above level T6, and in this population, it was expected to find lower lung volumes and capacities [23].
There is consensus that, after the SCI, the damage to the pulmonary function is caused by the decrease in volume and restrictive respiratory insufficiency with hypoventilation and progressive loss of pulmonary condition. The worst dysfunctions are seen in the highest lesions [22,23,24]. Cotton et al, in 2005, evaluate 596 SCI patients and reported that 51.1% of individuals with lesions between the first and sixth thoracic neurological level had pulmonary complications, against 34.5% of patients with lesions between seventh and the twelfth thoracic neurological level [25], data is similar the Morais et al, in 2013, with 72 subjects, that report that the pneumonia was the main clinical complication of individuals with SCI, especially in high lesions [26]. These data demonstrate the importance of a validated instrument to monitor respiratory function in SCI.
The International SCI Pulmonary Function Basic Data Set is a simple and easy-to-apply instrument and can be handled by medical professionals and therapists at a rehabilitation center serving SCI patients. The number of participants in the validation process in the current study, although smaller than recommended, was sufficient to validate the instrument, as a high degree of reliability and reproducibility was obtained.
The recommendation for the use of the International SCI Pulmonary Function Basic Data Set in the daily routine of care in rehabilitation centers can be done safely, as it improves the quality of information about patients’ lung function. The main qualities of the instrument are simplicity, speed, and the low cost of its application, allowing its use in most of the country’s rehabilitation centers.
The limitations of the present study would be the small size of the sample and including only one patient with non-traumatic SCI.
A possible continuation of the current project would be a national multicenter study to test the applicability of the instrument to collect epidemiological data about the pulmonary function in SCI patients, contribute to improve care and rehabilitation and reduce morbidity and mortality.
Conclusion
The translation into Portuguese spoken in Brazil’s of the International SCI Pulmonary Function Basic Data Set created an instrument similar the original without language and cultural disagreements.
Validation of the International SCI Pulmonary Function Basic Data Set showed that the instrument has reliability and high reproducibility allowing its use in the evaluation of SCI patients in Brazil.
Data availability
The data that support the findings of this study are available on request from the corresponding author Freitas SF. The data are not publicly available due to them containing information that could compromise research participant privacy/consent.
References
Moura EWD, Lima E, Borges D, Silva PDAC. Fisioterapia: aspectos clínicos e práticos da reabilitação. Fisioterapia: aspectos clínicos e práticos da reabilitação 2010; 720.
Ministério da Saúde. Departamento de Ações Programáticas Estratégicas: Diretrizes de Atenção à Pessoa com Lesão Medular. Ministério da Saúde Brasília (DF); 2013.
Center NSCIS. Spinal Cord Injury facts and figures at a glance: 2020 SCI data sheet. Birmingham, AL: University of Alabama at Birmingham. 2020.
Committee NCSCI. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) - What’s new? Spinal Cord. 2019;57:815.
Lee B, Cripps RA, Fitzharris M, Wing P. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6.
Biering-Sørensen F, Krassioukov A, Alexander M, Donovan W, Karlsson A, Mueller G, et al. International spinal cord injury pulmonary function basic data set. Spinal Cord. 2012;50:418–21.
Grillo ACDS, Faleiros F, Silva JCF, Tate DG, Greve JMD, Tholl AD, et al. Tradução Para Língua Portuguesa do Data Set Trato Urinário Inferior Para Indivíduos com Lesão Medular. Texto & Contexto-Enfermagem. 2018;27.
Biering-Sørensen F, Charlifue S, Devivo M, Noonan V, Post M, Stripling T, et al. International spinal cord injury data sets. Spinal Cord. 2006;44:530–4.
Biering-Sørensen F, Alexander M, Burns S, Charlifue S, DeVivo M, Dietz V, et al. Recommendations for translation and reliability testing of international spinal cord injury data sets. Spinal Cord. 2011;49:357–60.
Pereira CADC, Sato T, Rodrigues SC, et al. reference values for forced spirometry in white adults in Brazil. Jornal Brasileiro de. Pneumologia. 2007;33:397–406.
Costa D, Jamami M. Fundamentals of spirometry. Rev Bras Physioter. 2001;5:95–102.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia Med: Biochemia Med. 2012;22:276–82.
Monteiro GTR, Hora HRM. Public health research: how to develop and validate data collection instruments: Editora Appris. 2013.
Biering-Sørensen F, DeVivo M, Noonan V, Post M, Stripling T, Wing P. International Spinal Cord Injury Data Sets. Spinal Cord. 2006 Sep;44:530–4.
Devivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International Spinal Cord Injury Core Data Set. Spinal Cord. 2006;44:535–40.
Zimmer MB, Nantwi K, Goshgarian HG. Effect of spinal cord injury on the neural regulation of respiratory function. Exp Neurol. 2008;209:399–406.
Yamauti R, Sato Azeka M, Strike J, Furlan J, Forchheimer M, Tate D, et al. Reliability of the Portuguese Version of the International Bowel Function Basic Spinal Cord Injury (SCI) Dataset. 51st ISCoS Annual Scientific Meeting London UK/3 − 5 September 2012 Poster 236; 2012.
Oikawa A, Castineira C, Strike J, Furlan J, Forchheimer M, Tate D, et al. Reliability of the English version of International Quality of Life spinal cord injury dataset. 52nd Meeting Istanbul Turkey/ 28-30 October 2013 Poster P101; 2013.
Xing H, Liu N, Zhou M, Cao Y, Wang D. Chinese Version of International Spinal Cord Injury Data Set Quality of Life Basic Data Set. Available from: https://www.iscos.org.uk//international-sci-quality-of-life-data-sets.
Faleiros F, Silva JCF e, Cordeiro A, Tholl AD, Fumincelli L, Tate D. Qualidade de vida e lesão medular traumática: um estudo com uso de data sets internacionais. Rev. Eletr. Enferm. [Internet]. 5º de outubro de 2020 [citado 29º de novembro de 2022];22:56256. Available in: https://revistas.ufg.br/fen/article/view/56256.
Danilack VA, Stolzmann KL, Gagnon DR, Brown R, Tun CG, Morse LR, et al. Associations with chest illness and mortality in chronic spinal cord injury. J Spinal Cord Med. 2014;37:662–9.
Schilero GJ, Bauman WA, Radulovic M. Traumatic spinal cord injury: pulmonary physiologic principles and management. Clin chest Med. 2018;39:411–25.
Berlowitz DJ, Tamplin J. Respiratory muscle training for cervical spinal cord injury. Cochrane Database of Systematic Reviews, n. 7, 2013.
Sankari A, Badr MS, Martin JL, Ayas NT, Berlowitz DJ. Impact of spinal cord injury on sleep: current perspectives. Nat Sci sleep. 2019;11:219.
Cotton BA, Pryor JP, Chinwalla I, Wiebe DJ, Reilly PM, Schwab CW, et al. Respiratory complications and mortality risk associated with a thoracic spine injury. J Trauma Acute Care Surg. 2005;59:1400–9.
Freitas D, Morais JS, Neto M, Spotti AR, Tognola WA. Preditores de Complicações Clínicas em Pacientes com Trauma Raquimedular. Column/Column. 2014;13:139–42.
Author information
Authors and Affiliations
Contributions
SFdF participated in the preparation of the study design, translation, application of interviews, interpretation and analysis of data obtained, writing and submission of the article. CVGP participated in the elaboration of the study design, translation and application of the interviews. SKA participated in the application of the interviews, interpretation and analysis of the data obtained. JMDG participated in the elaboration of the study design, translation, interpretation and analysis of the obtained data and writing of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Freitas, S.F.d., Pires, C.V.G., Asa, S.K. et al. Translation and validation into Portuguese of the international spinal cord injury pulmonary function basic data set. Spinal Cord Ser Cases 8, 89 (2022). https://doi.org/10.1038/s41394-022-00555-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00555-1