Abstract
Introduction
The sinonasal carcinoma are rare tumors of the head and neck. The undifferentiated sinonasal carcinoma subtypes are constantly being explored and new mutations, with different prognosis markers and biological behaviors are being described. The SMARCB1 negative sinonasal carcinoma subtypes have been recently described with few reports of leptomeningeal and spinal cord invasion.
Case presentation
This study presents the case of a 59-year-old woman, with no previous disease, presenting initially with epistaxis that evolved to cranial nerve deficits and a left eye complete oftalmoplegia. After diagnostic investigation, she had a diagnosis of a left ethmoid sinus sinonasal carcinoma. Following resection of the tumor, she evolved with a right foot drop that eventually has been linked to diffuse spinal cord impairment. The histopathological diagnosis confirmed a SMARCB1 negative sinonasal carcinoma. Due to the diffuse metastasis, she underwent palliative care and died eight months after the surgery.
Discussion
Spinal cord metastasis may manifest with different clinical signs. Our case shows a rare manifestation of SMARCB1-deficient sinonasal carcinoma, a new subtype of sinonasal carcinoma, summarizing the importance of a high grade of suspicion of spinal cord invasion on these patients. SMARCB1 sinonasal carcinomas are rare new tumors of the head and neck, whose biological behaviors are yet to be explored. To the best of our knowledge, this is one of the few case reports describing simultaneous spread of this tumor to the central nervous system and spinal cord.
Similar content being viewed by others
Introduction
Sinonasal carcinomas are rare tumors of the head and neck, with an incidence rate of ~1 case per 100,000 inhabitants worldwide [1]. There is high heterogeneity in tumors of this body region. Most of them are squamous cell carcinomas or adenocarcinomas, both of which are strongly associated with environmental insults [1]. Some of these carcinomas are undifferentiated, such as the recently described SMARCB1-deficient sinonasal carcinoma found in the sinonasal tract [2]. The neurological symptoms are usually secondary to local invasion of advanced tumors, but spinal cord metastasis has also been described in the literature [3] and are sometimes associated with an aggressive pattern of invasion. Awareness of the neural spread of this variant of sinonasal carcinomas is crucial.
Herein, we present a case of diffuse spinal cord metastasis following surgical resection with an initial clinical feature of a right foot drop.
Case presentation
A previously healthy 59-year-old woman presented with progressive epistaxis for 2 months, which was associated with headache and left-sided eye ophthalmoplegia that progressed in the previous week. She lived far from big medical centers, so she came to São Paulo looking for more diagnostic resources. She was a smoker according to her medical history. She had no history of occupational exposure to wood dust and her familiar history was unremarkable. On admission, her neurological examination revealed palsy of all extraocular muscles in the left eye, with no light response to stimulation. She had ipsilateral complete ptosis, suggesting oculomotor nerve accometiment. She also presented with hypoesthesia in the V1 division of the trigeminal nerve and an absent ipsilateral corneo palpebral reflex. There were no other significant neurological findings during her initial clinical examination.
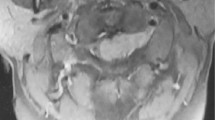
The involvement of the nerves responsible for ocular motor control and the V1 division of the trigeminal nerve revealed topographic orbital accometiment; therefore, magnetic resonance imaging (Fig. 1) was performed and a mass with hyperproteic/hematic content enhanced by paramagnetic contrast agents was identified. It was located on the left ethmoidal cell and extended to the left ethmoid sinus and orbit. It also compressed the pituitary gland and meninges, with leptomeningeal spreading.
Tissue formation with intermediate signal on T2 and high signal on T(E, F) suggestive of hyperproteic/hematic content, with paramagnetic contrast enhancement (D), inside the posterior ethmoid cell on the left, extending to the sphenoid sinus, to the cavernous sinus and orbital apex and superior aspect of the orbit ipsilaterally, with involvement of the superior and lateral rectus muscles, superior oblique and superior ophthalmic vein. There is also a slight extension to the intrasellar compartment, compressing the pituitary gland contralaterally. There is circumferential involvement of the internal carotid artery in its cavernous segment, with a reduction in its caliber and apparent thickening and parietal enhancement. There is also an extension of this process to the dura mater that lines the middle fossa and the lateral aspect of the anterior fossa on the left, which is thickened and impregnated by gadolinium (A–C), presenting a nodulariform aspect adjacent to the lesser wing of the sphenoid on this side. The lesion showed no expressive diffusion restriction (G, H).
Surgery was indicated, and left maxillary sinusotomy was performed following left intranasal ethmoidectomy and frontal sinusotomy. The mass was only partially removed because the sphenoid sinus was limited due to its extension.
Histological studies showed undifferentiated malignant neoplasia infiltrating the mucosa with extensive necrosis, leptomeningeal spreading on the dura mater fragment, and vascular embolization.
Immunohistochemical staining showed positivity for p63; p40; and 40-, 48-, 50-, and 50.6-kDA cytokeratins (markers of sinonasal heritage); however, the Epstein-Barr virus (EBV) and nuclear protein in testis (NUT) test results were negative (excluding other variants of undifferentiated sinonasal carcinoma). A loss of expression of SMARCB1 (INI-1) was noted (Fig. 2).
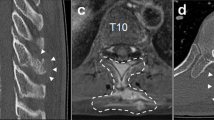
The final diagnosis was SMARCB1 (INI-1)-deficient sinonasal carcinoma with local spread. The patient remained stable after surgery until she developed a right foot drop that compromised her ambulation. Associated with the right foot drop, she had right plantar hypoesthesia, suggesting fibular accometiment or L5 radiculopathy. Her osteotendinous reflexes were normal, with no signs of pyramidal liberation. The patient denied any bladder or intestinal dysfunction. To make a differential diagnosis, lumbar spinal cord imaging was performed, and diffuse accometiment of the cervical, thoracic, and lumbosacral spinal cord segments with round lesions and low T2 signal intensity as well as high gadolinium enhancement was noted, which was suggestive of secondary neoplastic lesions (Fig. 3).
Presence of small, rounded lesions with low signal on T2 sequences, diffusely distributed in the cervical (A–D), thoracic (E–H), lumbar (I–L) vertebral bodies and in the sacral parts, showing intense enhancement by paramagnetic contrast medium, of different sizes, not accompanied by signs of rupture of the cortical bone or soft tissue component in an intra-spinal situation.
During five months of follow-up imaging studies, lesions on the liver and lungs were noted, suggesting metastasis. In general, the lesions were treated with chemotherapy and radiotherapy. Palliative care was started, and the overall survival from the time of diagnosis was ~8 months.
Discussion
Our case reports the biological behavior of a recently discovered subtype of sinonasal carcinoma, presenting with a rare leptomeningeal and spinal cord spreading. Carcinomas of the sinonasal tract are a heterogeneous group of disorders that are rare diseases and are mainly related to occupational factors, such as those involving exposure to wood dust.
There is a rich genetic background among sinonasal carcinomas, with a high diversification of mutations. The most common types of sinonasal carcinomas are glandular and squamous cell carcinomas [1], but there is a group of sinonasal undifferentiated carcinomas whose genetic basis is constantly advancing. Among them, loss of nuclear SMARCB1 expression is a histological marker that has been recently described [2]. This type usually affects men and women equally, regardless of age. The average prognosis is 16 months after diagnosis [4].
As a new variant, only few case reports and series have been reported about the morphologic features and patterns of the central nervous system and spinal cord metastasis. These carcinomas are usually advanced at the time of diagnosis because of their vague symptoms and aggressive nature.
SMARCB1 is a component of the chromatin-remodeling protein complex, acting as a tumor suppressor gene. It is associated with a variety of rhabdoid tumors as well as a histological loss in INI1 expression. SMARCB1-deficient tumors usually do not have specific histological differentiations, such as glandular or squamous, and are mainly composed of basaloid and rhabdoid cells [5]. Loss of SMARCB1 expression has been described in many tumors outside the sinonasal tract, such as atypical teratoid/rhabdoid tumors and epithelioid sarcomas. These carcinomas are negative for NUT, human papillomavirus, and EBV.
There are cases described in the literature that highlight the aggressive features of these tumors [4, 5]. Despite its spreading characteristics, spinal cord metastasis in SMARC-B1 sinonasal carcinoma has been rarely described in case studies in the literature. In general, the most common sites of metastasis from sinonasal undifferentiated carcinomas are the cervical lymph nodes, lung, bone, and liver [4, 5]. The spinal cord is an atypical site of metastasis, as reported in a few cases of some of the largest case series in the literature [4, 5]. However, because of their rarity, only few cases of these tumors have been reported. Acevedo et al. [5] described a case of perineural spread and intradural metastasis with perineural and leptomeningeal spreading, which is similar to the metastasis noted in our case study.
The diagnosis of bone metastasis to the spinal vertebrae, such as the foot drop presented in our patient, probably secondary to a L5 radiculopathy. Spinal metastasis is a marker of poor prognosis with a low overall survival. The best oncologic approach for spinal metastasis is not clear, and patients should be managed by a multidisciplinary team.
The clinical should be aware of the potential aggression of these kinds of tumors. SMARCB1-deficient sinonasal carcinoma is a rare carcinoma of the sinonasal tract that has been rarely described in the literature. The aggressive nature of the tumor combined with its potential for metastasis in the central nervous system can quickly lead to an advanced disease with poor prognosis, regardless of the primary lesion. The biological behavior of this newly described tumor is being elucidated. The small interval between surgical resection and spinal metastasis should enlightens the importance of studying how these undifferentiated carcinoma spreads through the central nervous system, which may be important for developing target therapies and better understating the natural history of SMARCB1-deficient sinonasal carcinoma.
Data availability
Data availability is found within the published article and its supplementary files. Additional data are available from the corresponding author on reasonable request.
References
Llorente JL, López F, Suárez C, Hermsen MA. Sinonasal carcinoma: clinical, pathological, genetic and therapeutic advances. Nat Rev Clin Oncol. 2014;11:460–72.
Agaimy A, Koch M, Lell M, Semrau S, Dudek W, Wachter DL, et al. SMARCB1(INI1)-deficient sinonasal basaloid carcinoma: a novel member of the expanding family of SMARCB1-deficient neoplasms. Am J Surg Pathol. 2014;38:1274–81.
Agaimy A, Hartmann A, Antonescu CR, Chiosea SI, El-Mofty SK, Geddert H, et al. SMARCB1 (INI-1)-deficient sinonasal carcinoma: a series of 39 cases expanding the morphologic and clinicopathologic spectrum of a recently described entity. Am J Surg Pathol. 2017;41:458–71.
Kakkar A, Antony VM, Pramanik R, Sakthivel P, Singh CA, Jain D. SMARCB1 (INI1)-deficient sinonasal carcinoma: a series of 13 cases with assessment of histologic patterns. Hum Pathol. 2019;83:59–67.
Gomez-Acevedo H, Patterson JD, Sardar S, Gokden M, Das BC, Ussery DW, et al. SMARC-B1 deficient sinonasal carcinoma metastasis to the brain with next generation sequencing data: a case report of perineural invasion progressing to leptomeningeal invasion. BMC Cancer. 2019;19:827.
Acknowledgements
I thank Dr. Alex Machado Baeta and Dr. Hennan Salzedas Teixeira for their valuable inputs on my study. And the patient and her family for their dedication.
Author information
Authors and Affiliations
Contributions
MAS was responsible for reviewing the protocol and writing the report. RGL was responsible for extracting and analyzing data. HST was responsible for reviewing and orientating the report. BMC was responsible for extracting and analyzing data. VMB contributed to data extraction. WSMF was responsible for extracting and analyzing data. CMSC was responsible for radiological orientation. MRN was responsible for neurosurgical orientation. AMB was responsible for reviewing and orientating the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Ethical approval was not required, we had patient and familiar authorization to use these data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva, M.A., Bentes, R.G.L., Teixeira, H.S. et al. Diffuse spinal cord metastasis after resection of SMARCB1 sinonasal carcinoma manifesting with a right foot drop—a case report. Spinal Cord Ser Cases 8, 64 (2022). https://doi.org/10.1038/s41394-022-00532-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00532-8