Abstract
Introduction
Chronic irritation caused by urinary catheter may predispose to metaplastic changes in the bladder and very rarely, nephrogenic metaplasia.
Case presentation
A 53-year-old lady with T-2 paraplegia and urethral catheter drainage for 27 years presented with haematuria. MRI of pelvis, performed seven years ago, showed a 10 cm intramural fibroid within the anterior aspect of the uterine body which was pushing the collapsed urinary bladder containing the Foley catheter to the left. The patient decided to avoid surgery to remove the fibroid at that time. Ultrasound scan of the urinary bladder done now, revealed a polypoidal lesion in the left superolateral wall. Superficial enhancing lesion with no invasion of the bladder wall was seen in the CT urography. Cystoscopy showed extensive catheter reaction, and in the centre, a slightly more papillary area, which was resected. Histology revealed inflamed bladder mucosa showing tubular and papillary structures lined by cuboidal epithelial cells; the features were of nephrogenic metaplasia. The tubular and papillary structures were lined by cells showing positive immunohistochemical staining for CK7 and PAX8.
Discussion
Catheter reaction and nephrogenic metaplasia was found in the left superolateral wall of the bladder where the large uterine fibroid was pushing the balloon of the catheter against the bladder wall for more than seven years. The patient decided to undergo surgery to remove the large fibroid and thereby prevent further pressure effects upon the urinary bladder.
Similar content being viewed by others
Background
Nephrogenic metaplasia represents non-neoplastic localised or diffuse, papillary, tubular, or cystic metaplastic changes of the urothelium in response to chronic infection, calculi, injury, or prolonged catheterization [1]. Nephrogenic metaplasia is found infrequently in neuropathic bladder. Urethro-cystoscopy performed in a consecutive series of 129 patients, who were suffering from neurogenic lower urinary tract dysfunction for at least five years, revealed suspicious lesion in 13 patients; transurethral resection of the bladder lesion and/or random bladder biopsies were carried out. Nephrogenic metaplasia or adenoma was detected in three patients [2]. We present a female patient with spinal cord injury, who had indwelling urethral catheter drainage for 27 years and developed haematuria. A large uterine fibroid has been pressing upon the collapsed urinary bladder and pushing the balloon of Foley catheter against the left lateral wall for more than seven years. Cystoscopy revealed catheter reaction and papillary lesion at this site. Histology showed nephrogenic metaplasia.
Case presentation
A 25-year-old female person sustained complete spinal cord injury at T-2 level following a motorcycle accident in 1994. She has been managing her urinary bladder by indwelling urethral catheter drainage.
In 2014, a mass was noticed in the right iliac fossa. Ultrasound scan of Pelvis (Transvaginal) showed enlarged uterus measuring 13 × 10 x 8.6 cm. A well-defined solid heterogeneous mass was detected at the fundus. MRI Pelvis revealed Foley catheter in empty bladder. The uterus was enlarged due to presence of a 10 cm intramural fibroid within the anterior aspect of the uterine body. Further smaller fibroids of 3 cm and 1.5 cm were noted in the fundus. All showed signs of cystic degeneration. The uterus was slightly deviated to the right. The large uterine fibroid was pressing upon the collapsed urinary bladder and pushing the balloon of Foley catheter against the left lateral wall. (Figs. 1 and 2) Treatment options were discussed, and the patient decided to avoid surgery. Hysteroscopy was done; Mirena coil was fitted to control heavy bleeding. Heavy bleeding persisted with Mirena coil, and she was prescribed Norethisterone cyclically 21 days on and seven days off.
In 2021, this patient noticed a small amount of haematuria. She had been having increased spasms and was sweating below the level of spinal cord injury.
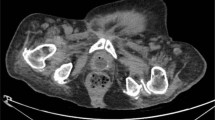
Ultrasound scan of the urinary tract revealed a polypoidal endoluminal projection from the left superolateral wall of the urinary bladder projecting into the lumen. This lesion measured 16 mm × 10 mm. (Fig. 3) The kidneys appeared normal. CT Urography revealed superficial enhancing tumour of the bladder mucosa on the left side with no direct invasion of the bladder wall. (Fig. 4) There was no extravesical spread. There was no filling defect in the pelvicalyceal systems. When the bladder was full, the extrinsic pressure effect by the uterine fibroid upon the Foley catheter was reduced to a large extent.
Cystoscopy revealed extensive catheter reaction in the left side of the bladder dome. In the centre of the catheter reaction, there was a slightly more papillary area, which was resected.
Histology revealed inflamed bladder mucosa showing tubular and papillary structures lined by cuboidal epithelial cells; the features were of nephrogenic metaplasia. (Fig. 5) There was no evidence of carcinoma in situ or invasive malignancy. The tubular and papillary structures were lined by cells showing positive immune-histochemical staining for Cytokeratin7. (Fig. 6) The lining cuboidal cells showed positive immune-histochemical staining for PAX8 (paired box gene 8–family of transcription factors that regulate organogenesis). (Fig. 7)
The pressure effect of the large uterine fibroid upon the catheter balloon was reduced greatly when the urinary bladder was allowed to fill. This observation in CT urography encouraged us to recommend the use of Flip-Flo catheter valve which would allow filling of the bladder. The patient can open the Flip-Flo valve say, every 3–4 h and empty the bladder. This manoeuvre will reduce the extrinsic pressure effect of the large uterine fibroid upon the Foley catheter tip and balloon against the left superolateral wall of a collapsed bladder. In addition to the use of a Flip-Flo valve, periodic screening of the urinary tract by ultrasound scan was arranged during follow-up.
A detailed discussion took place with the patient about the effect of a large uterine fibroid aggravating the chronic irritation caused by the catheter balloon against the left lateral bladder wall. The patient decided to undergo surgery to remove the large fibroid and thereby prevent further pressure effects upon the urinary bladder. The patient is awaiting treatment by Gynaecologist.
Discussion
Nephrogenic metaplasia or nephrogenic adenoma is an uncommon metaplastic lesion of the urothelium found in all locations of the urinary tract often with multifocal appearance and most seen in the urinary bladder. Predisposing factors for its occurrence include urothelial irritation by trauma, previous surgery, urinary calculi, radiation, chronic infections, and urinary catheterization [3, 4]. Patients may be asymptomatic and nephrogenic metaplasia may be discovered during surveillance cystoscopy of a person with spinal cord injury. Or a patient may present with haematuria. Transurethral resection of the lesion is the treatment of choice. Nephrogenic metaplasia may recur; therefore, these patients require follow-up by ultrasound scan or cystoscopy. Very rarely, malignant transformation has been reported [5].
Non-malignant metaplastic lesions of the urinary bladder are seen frequently in persons with spinal cord injury, who have long-term indwelling urinary catheter. Bladder biopsies in 208 spinal cord injury patients who had indwelling urethral or suprapubic catheter for more than 8.5 years revealed cystitis in 89%; non-keratinising squamous metaplasia in 47%; cystitis glandularis in 17%; cystitis cystica in 12%; cystitis follicularis in 10%; keratinising squamous metaplasia in 6%; intestinal metaplasia in 4%; dysplasia in 2%; and nephrogenic metaplasia/adenoma in 1% [6]. This shows that nephrogenic metaplasia is seen infrequently in spinal cord injury patients with chronic indwelling urinary catheters.
Our patient declined surgery for the large uterine fibroid seven years ago. It is possible that the large uterine fibroid produced extrinsic pressure effect upon the collapsed bladder and aggravated the chronic irritation caused by the Foley balloon on the superolateral bladder wall for several years. Such chronic irritation by the catheter balloon produced catheter reaction at this site and possibly nephrogenic metaplasia as well. We advised our patient to use Flip-Flo catheter valve and allow the bladder to get filled with urine to minimise such pressure effect and avoid any increase in the severity of irritation caused by the Foley balloon on the bladder wall. Our patient understood the possible adverse effect of uterine fibroid in aggravating the chronic irritation produced by the Foley balloon and decided to undergo surgery for uterine fibroid now.
The immune histochemistry profile of nephrogenic adenoma shows characteristic expression of renal tubule markers CK7, CD10, AMACR, PAX2 and PAX8, and the absence of urothelial markers (thrombomodulin and p63) and prostate antigens (prostate-specific antigen (PSA) and prostate alkaline phosphatase (PAP) [7, 8]. In our patient, the lining cuboidal cells of nephrogenic metaplasia showed positive immunohistochemical staining for PAX8. The cells lining the tubular and papillary structures showed positive immunohistochemical staining for CK7. We also performed immune-histochemical staining of an archival specimen of nephrogenic metaplasia in a bladder biopsy taken from an able-bodied individual with chronic cystitis to see whether there are differences in the staining pattern of nephrogenic metaplasia occurring in a neuropathic bladder and in the normally innervated bladder. Comparison of the immunostaining pattern for CK7 and PAX8 between the archival specimen and our patient with neuropathic bladder showed no significant variation. Perhaps, a study of larger number of specimens may confirm that the immunostaining pattern of nephrogenic metaplasia in a neuropathic bladder is similar to that observed in nephrogenic metaplasia found in normally innervated urinary bladder.
Learning point
Chronic irritation due to long-term Foley catheter drainage may predispose to metaplastic changes in the urinary bladder. Nephrogenic metaplasia in the urinary bladder associated with long-term urethral Foley catheter in persons with spinal cord injury is very rare. In this patient, a large uterine fibroid was pushing the balloon of the catheter against the collapsed bladder wall for more than seven years and aggravated the local irritation caused by the Foley catheter. Catheter reaction and nephrogenic metaplasia was found in this location. The patient decided to undergo hysterectomy to stop continuing pressure effect on the bladder wall by the large uterine fibroid.
Data availability
All relevant clinical data pertaining to this case have been provided. Only the confidential data of the patient such as name, date of birth have been withheld to maintain anonymity of the patient.
References
Gandhi JS. Nephrogenic metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdernephroadenoma.html. Pathology Outlines - Nephrogenic metaplasia Accessed February 7th, 2022.
Sammer U, Walter M, Knüpfer SC, Mehnert U, Bode-Lesniewska B, Kessler TM, et al. Do we need surveillance urethro-cystoscopy in patients with neurogenic lower urinary tract dysfunction? PLoS ONE. 2015;10:e0140970. https://doi.org/10.1371/journal.pone.0140970.
Chen C-S, Cheng C-L. Nephrogenic adenoma of the urinary bladder: clinical experience and review of the literature. J Chin Med Assoc. 2006;69:166–8. PMID: 16689198 23
Zougkas K, Kalafatis M, Kalafatis P. Nephrogenic adenoma of the urinary bladder. Int Urol Nephrol. 2004;36:513–7.
Hungerhuber E, Bach E, Hartmann A, Frimberger D, Stief C, Zaak D, et al. Adenocarcinoma of the bladder following nephrogenic adenoma: a case report. J Med Case Rep. 2008;2:164. https://doi.org/10.1186/1752-1947-2-164.
Delnay KM, Stonehill WH, Goldman H, Jukkola AF, Dmochowski RR. Bladder histological changes associated with chronic indwelling urinary catheter. J Urol. 1999;161:1106–8.
Piña-Oviedo S, Shen S, Truong L. Flat pattern of nephrogenic adenoma: previously unrecognized pattern unveiled using PAX2 and PAX8 immunohistochemistry. Mod Pathol. 2013;26:792–8. https://doi.org/10.1038/modpathol.2012.239.
Quinones W, Ziober A, Yao Y, Bing Z. Immunohistochemical markers for the differential diagnosis of nephrogenic adenomas. Ann Diagn Pathol. 2013;17:41–4. https://doi.org/10.1016/j.anndiagpath.2012.05.003.
Acknowledgements
The authors are most grateful to all doctors, present and past, who looked after this patient during the 27 years after she sustained spinal cord injury.
Author information
Authors and Affiliations
Contributions
VS conceived the idea, collected data, discussed with other authors, wrote the draft; NH performed and interpreted histology and immunohistochemical images; RK performed surgery; PH interpreted radiological images; BMS provided ideas and contributed to preparation of the draft. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Subramanian, V., Hasan, N., Khadr, R. et al. Nephrogenic metaplasia in a female person with spinal cord injury: chronic irritation caused by Foley balloon was aggravated by a large uterine fibroid pressing upon the bladder wall for several years: a case report. Spinal Cord Ser Cases 8, 51 (2022). https://doi.org/10.1038/s41394-022-00521-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00521-x