Abstract
Introduction
Spinal epidural hematomas are a surgical emergency, the delay in diagnosis can develop devastating sequelae due to its acute and progressive course. If not treated properly, it may lead to death or permanent neurological deficit. It is a rare condition that can occur in patients with hematologic pathology.
Case presentation
We report a case report and literature review of a patient with antiphospholipid syndrome, who undergoes a diagnostic lumbar puncture for probable fungal meningitis. Developed a spinal acute epidural hematoma with neurological involvement that is evidenced in MRI. Urgent surgical decompression was performed with good results.
Discussion
Despite the low incidence of an epidural hematoma in patients who undergo lumbar puncture, it is important to perform a thorough evaluation in any patient with coagulation abnormalities prior and after a lumbar puncture, by reason of the inherent possibility of developing an epidural hematoma at the site of the procedure. In the same way, early diagnosis and aggressive treatment is necessary in patients who develop progressive neurological symptoms to limit the damage and improve the prognosis for neurological recovery.
Similar content being viewed by others
Introduction
Lumbar puncture is a common medical procedure that is essential for the diagnosis and treatment of central nervous system infections, neurological diseases and certain types of cancer [1, 2].
It’s important to highlight the spinal epidural hematoma as a catastrophic adverse effect due to its acute and progressive course. If not treated properly, it may lead to death or permanent neurological deficit [1].
There are few studies on the incidence of this type of injury due to its low incidence. An incidence of 1 in 190,000 cases of epidural anesthetics in Germany [3], 1 in 250,000 in the UK [4] and 1 in 150,000 in Canada [5] related to continuous epidural anesthesia. Lately, in a Danish cohort study, the risk of spinal hematoma following lumbar puncture was 0.20% among patients without coagulopathy and 0.23% among those with coagulopathy [1].
Spinal hematoma presents as severe back pain, radiculopathy, urinary incontinence, and progressive paraparesis [6]. The epidural space is surrounded by the epidural venous plexus and has been considered the source of epidural hematoma [7].
Bodilsen et al. described Independent risk factors for spinal hematoma: male sex, age older than 60 years and unpaired international normalized ratio (INR) [1]. Puncture difficulties and bleeding at the point of insertion were reported to be major risk factors for epidural hematoma [8]. Also, a significant correlation has been described between preexisting coagulopathy and poor neurological outcome [4, 8, 9]. Specifically, heparin and coumadin are closely correlated for this disease, and their contraindication to spinal anesthesia is well defined [3].
Antiphospholipid syndrome (APS) is an autoimmune disease, and its most critical pathological process is thrombosis, which may explain most of the clinical features, characterized by venous, arterial or microvascular thrombosis. Patients with moderate-to-high-risk antiphospholipid-anti- body profiles are often treated with warfarin (target INR, 2–3) [10].
We report a case of a patient with APS that presented an epidural hematoma after a lumbar puncture following by the approach and treatment established.
Case presentation
A 21-year-old male with a diagnosis of systemic Lupus erythematous and triple positive APS, lupus anticoagulant (LA), anticardiolipin, and antiβ2-glycoprotein 1 (antiβ2-gp1), diagnosed one year before, with bilateral polyarthralgia asymmetric diseases that begin in the ankles and knees, and that ascend to the proximal metacarpophalangeal and interphalangeal joints, as well as lupus nephropathy syndrome with grade IV/V membranous changes and thrombotic microangiopathy diagnosed by renal biopsy. In addition to a history of a previous hospitalization 1 year ago for pulmonary coccidioidomycosis treated with amphotericin b 100 mg/day for 15 days followed with fluconazole 400 mg/day for 1 month; and warfarin 0.5 mg/day was started. The last one was suspended by the patient without medical prescription 1 month prior to his admission.
The current hospitalization presented fever, oral ulcers, malar rash, dyspnea, urinary symptoms, hair loss, and chest pain, also, presented clinical data of neurological infection of 6 days of evolution; with headache in the right hemicranium of intensity 8/10 in visual analogic scale (VAS) that does not yield to the use of analgesics, associated with episodes of nausea, paresthesia in the right hemiface, right upper extremity and decreased contralateral visual acuity. At the time of hospitalization, he was conscious, oriented, cooperative, negative pull hair test, cervical ganglia were not palpable, left upper and inferior limbs in good neurovascular condition. Laboratory studies are carried out presenting PT 12.8, TTP 54, INR 1.1 platelets of 187,000 K/μL, hemoglobin of 13.5 g/dL and leukocytes of 9.47 K/μL.
Magnetic resonance image (MRI) of the brain is performed: at the intra-axial level in the right wedge and the left postcentral gyrus, two rounded images were identified, hyperintense on T1, hypointense on T2, with peripheral ring enhancement after gadolinium administration, with measurements of 19 × 18 × 16 mm in its face-caudal, lateral and dorsoventral axes respectively, with perilesional vasogenic edema. And the area of gliosis in periventricular white matter at the level of the right corona radiata (Fig. 1).
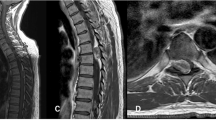
As part of its diagnostic approach, a lumbar puncture with a standard 22G needle, is performed without complications, with a predominantly lymphocytic result, negative for bacteriological culture. After the findings in the MRI, the patient’s symptoms, and the results of the lumbar puncture, the diagnosis of intracerebral fungal abscesses was made. Antifungal treatment is started with amphotericin B 80 mg daily/14 days, fluconazole 800 mg daily/30 days; as well as acetylsalicylic acid 100 mg daily, prednisone 5 mg daily, hydroxychloroquine 300 mg daily, finally the enoxaparin 80 mg subcutaneous each 12 h was started 6 h after lumbar punction. Seven days after the lumbar puncture, the patient presented low back pain, VAS 10/10, there was paresthesia in both lower extremities sensitivity (1/2 in both), decreased strength only in the right one (2/5 right, 5/5 left) and hyporeflexia (+) distally to L4 in the right lower limb, accompanied by impaired sensitivity in the perianal area, with bladder dysfunction, with urinary retention, classified as C in ASIA Impairment Scale (AIS) [11]. Spine compression compatible with cauda equina syndrome was clinically diagnosed. Lumbar MRI was performed showing a mass in the epidural region with a predominance in posterior structures, hyperintense on both T1- and T2-weighted images, which invades the lumbar canal at L4 (Fig. 2), corresponding to the diagnosis of epidural hematoma.
With the following laboratory results at the time of the surgery, prothrombin time (PT) 13.7 seg, partial thromboplastin time PTT 73.3 seg, INR 1.19, platelets 275,000 K/μL and hemoglobin of 12.6 g/dL and leucocytes of 7.14 K/μL at the time of the surgery.
A vertebral decompression with laminotomy at the level of L4 was performed 36 h after the onset of symptoms. Intraoperatively, a significant amount of coagulated blood was observed from the epidural region (Fig. 3).
In the 24 h after the surgical treatment, he presented clinical improvement in muscle strength of right lower limb 4/5, left limb without decreased strength; sensitivity continued with 1/2 distally to L4 in both extremities; also, showed restoration of sensitivity in the perianal area and recovery of bladder dysfunction. At last, the pain decreased, with a VAS 2/10, After 20 rehabilitation sessions the patient presented strength of right lower limbs 4/5 and sensitivity 2/2 distally to L4, with a D in AIS.
Enoxaparin 80 mg subcutaneous every 12 h was reinitiated 72 h after surgery. The patient completed the antifungal treatment, and was discharged with warfarin 2.5 mg/daily with an INR of 2.56.
Discussion
Our patient had a history of APS which is a prothrombotic disorder, in addition to presenting a neurological disease, undergoing a diagnostic lumbar puncture. At the time of the study, the patient did not have anticoagulant treatment and the laboratory tests were in normal ranges. A fungal brain abscess was diagnosed. Also, presented an acute lumbar epidural hematoma with neurological alteration, an urgent vertebral decompression with laminotomy at the L4 level 36 h after the onset of symptoms was realized. After his treatment and rehabilitation, presented good clinical evolution with neurological recovery.
The epidural hematoma is a devastating condition with serious consequences for the person who presented it. An early diagnosis and aggressive treatment are crucial in patients who develop neurological injury. Epidural and subdural spinal cord hematomas present as intense knife-like pain at the hemorrhage site, followed by progressive paralysis below the level of the affected spinal cord [6]. The first choice for the diagnosis is magnetic resonance imaging. After 24 h, hematomas often show high intensity on T1 and T2-weighted images, as it was presented in our patient [12].
Kreppel et al. performed a large systematic review and meta-analysis of 613 patients with spinal hematoma found a male predominance of 2:1 and a peak incidence among patients in patients of 60-70 years. Moreover, only 10% of the cases were attributed to lumbar puncture or spinal blockade, most of whom were treated with intravenous heparin [6]. In this case, the patient had a diagnostic lumbar puncture and unlike the reported risk factors, didn’t have administered heparin before the lumbar puncture. Similarly, Horlocker and Wedel, described that most of the patients are between 55 and 70 years old, and a predominance of 63.9% in men [13]. Contrary, our patient presented at younger age than the range described.
There are few studies about the risk of spinal cord hematoma after lumbar puncture and are limited to selected patients with small to moderate sample sizes [1]. Horlocker and Wedel described the following risk factors for spinal hematoma in neuraxial blockade: anatomic abnormalities of the spinal cord and vertebral column, difficult or repeated puncture, larger needle size, older age, the use of an indwelling epidural catheter as opposed to “single shot” injection and the removal of the epidural catheter [13]. Although, Brown et al. demonstrated that the presence of preexisting coagulopathy correlates with a worse outcome at 6–12 months [9]. In our patient, presented a single time procedure, with a standard 22G needle for the lumbar puncture and oppositely to what is published in the literature had a thrombotic disease without anticoagulant treatment at the time of the diagnostic procedure.
The exact mechanism of the interaction between APS and coagulation to produce clinical events has not been elucidated. A clear diagnosis of APS requires at least one clinical and one laboratory standard. Many patients with APS have abnormal PTT; in fact, PTT is one of the most commonly used tests to diagnose APS. In studies evaluating the relationship between anticoagulant (LA) and thrombosis, LA is considered a clear risk factor for thrombosis. Besides our patient presented a bleeding complication that is not a typical clinical manifestation of APS, although there are occasional reports of severe bleeding in patients affected by the disease in patients with low platelet count or with anticoagulant treatment, risk factors that were not present in our patient. It has been previously associated with spinal subdural hemorrhage, but also with a case of spontaneous epidural hematoma with multiple venous thrombi in the lower limbs [14,15,16].
The complexity of management of these patients requires a multi-disciplinary team of physicians. Platelet counts below 50,000/mm3 settle him at high risk for bleeding, explaining this bleeding event [17]. The Guidelines suggest at least 20 × 109/L or 50 × 109/L platelet count is needed for lumbar puncture and INR levels lower than 1.5 for epidural catheters removal [18]. However, some experts recommend proceeding with lumbar puncture regardless of coagulation status if the medical indication in acute bacterial meningitis [2]. Our patient presented PTT and platelets in normal range at the time of the lumbar puncture. Also, the imperative of an early diagnosis due to neurological impairment it was decided to carry out the diagnostic lumbar puncture without setbacks. Furthermore, all guidelines were followed in this case, performing a lumbar puncture for the early diagnosis of meningitis and initiating enoxaparin 12 h after it [2, 18]. For this reason, the debate remains open to carry out subsequent studies in these patients with hematologic alterations to realize specific guidelines for them.
Our patient presented an epidural hematoma at L4 with an incomplete cauda equina dysfunction before surgery, previous studies showed good outcome in this group of patients [13, 19]. Patients with more severe symptoms in a shorter period of time trend to have larger hematomas; these are all associated with a worse prognosis, especially when four or more spinal segments are involved [6, 13, 19]. Likewise, it has been described that prompt treatment in order to decompress the affected levels is associated with a better prognosis. Many suggest decompression within 24–36 h of symptom onset for complete deficits and within 48 h for incomplete deficits [19]. However, many patients have remained paralyzed even with surgery [4]. In this case, an urgent vertebral decompression with laminotomy at the L4 level 36 h after the onset of symptoms was realized. Presenting a good clinical evolution with neurological recovery after the surgery.
In conclusion, it is important to perform a thorough evaluation in any patients with coagulation abnormalities prior and after a lumbar puncture, by reason of the inherent possibility of developing an epidural hematoma at the site of the procedure. In the same way, early diagnosis and aggressive treatment is necessary in patients who develop progressive neurological symptoms to limit the damage and improve the prognosis for neurological recovery.
References
Bodilsen J, Mariager T, Vestergaard HH, Christiansen MH, Kunwald M, Lüttichau HR, et al. Association of lumbar puncture with spinal hematoma in patients with and without coagulopathy. JAMA. 2020;324:1419–28.
McGill F, Heyderman RS, Michael BD, Defres S, Beeching NJ, Borrow R, et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect. 2016;72:405–38.
Wulf H. Epidural anaesthesia and spinal haematoma. Can J Anaesth. 1996;43:1260–71.
Stoll A, Sanchez M. Epidural hematoma after epidural block: implications for its use in pain management. Surg Neurol. 2002;57:235–40.
Ralley FE. Neuraxial anesthesia is contraindicated in patients undergoing heparinization for surgery. Pro: neuraxial anesthesia should not be used in patients undergoing heparinization for surgery. J Cardiothorac Vasc Anesth. 1996;10:957–60.
Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003;26:1–49.
Beatty RM, Winston KR. Spontaneous cervical epidural hematoma. A consideration of etiology. J Neurosurg. 1984;61:143–8.
Miyazaki M, Takasita M, Matsumoto H, Sonoda H, Tsumura H, Torisu T. Spinal epidural hematoma after removal of an epidural catheter: Case report and review of the literature. J Spinal Disord Tech. 2005;18:547–51.
Brown MW, Yilmaz TS, Kasper EM. Iatrogenic spinal hematoma as a complication of lumbar puncture: What is the risk and best management plan? Surg Neurol Int. 2016;7:S581–S589.
Kim JY, Lee S, Choi YY, Bae SC. Atypical bone change of spine caused by epidural venous thrombosis in systemic lupus erythematosus with antiphospholipid syndrome. Korean J Intern Med. 2017;32:573–4.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34:535–46.
Kumar Y, Hayashi D. Role of magnetic resonance imaging in acute spinal trauma: a pictorial review. BMC Musculoskelet Disord. 2016;17:1–11.
Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg Anesth Pain Med. 2018;43:263–309.
Jayachandran NV, Rajasekhar L, Narsimulu G, Prasad V. Antiphospholipid antibody syndrome presenting with disseminated bleeding and spinal subdural hemorrhage. Spinal Cord. 2007;45:753–5.
Kim WJ, Hong YK, Yoo WH. Epidural hematoma mimicking transverse myelitis in a patient with primary antiphospholipid syndrome. Rheumatol Int. 2008;28:709–12.
Zuliani G, Guerra G, Dalla Nora E, Fainardi E. Spinal anterior epidural hematoma in an elderly man with unrecognized lupic anticoagulant taking warfarin. Aging Clin Exp Res. 2011;23:498–500.
Drazin D, Westley Phillips H, Shirzadi A, Drazin N, Schievink W. Neurosurgical management for complicated catastrophic antiphospholipid syndrome. J Clin Neurosci. 2014;21:680–3.
Estcourt LJ, Birchall J, Allard S, Bassey SJ, Hersey P, Kerr JP. et al. British Committee for Standards in Haematology. Guidelines for the use of platelet transfusions. Br J Haematol. 2017;176:365–394.
Liao CC, Hsieh PC, Lin TK, Lin CL, Lo YL, Lee SC. Surgical treatment of spontaneous spinal epidural hematoma: A 5-year experience - Clinical article. J Neurosurg Spine. 2009;11:480–6.
Author information
Authors and Affiliations
Contributions
EGR conceived the case report, acquired data for the review of the literature, and analyzing the data in comparation to the case. JRPM designed the review of the literature, analyzing data, updated reference lists and contributed to writing the report. PMRF contributed to writing the report, and provided feedback to the report. VMPM contributed analyzing data, interpreting results and provided feedback to the report. LASB contributed to writing the report, extracting and analyzing data. CAAO conducted the research and provided feedback to the report. All the authors agreed to all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Guerrero-Rodriguez, E., Padilla-Medina, J.R., Reyes-Fernández, P.M. et al. Spinal epidural hematoma in antiphospholipid syndrome: case report and review of the literature. Spinal Cord Ser Cases 8, 11 (2022). https://doi.org/10.1038/s41394-022-00476-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00476-z
This article is cited by
-
The role of an open artificial intelligence platform in modern neurosurgical education: a preliminary study
Neurosurgical Review (2023)