Abstract
Study design
Case Series.
Objective
Sudden ‘lockdown’ to contain spread of SarsCoV-2 infection had far-reaching consequences on the Spine Unit of our tertiary care hospital, situated in a hilly-region of Northern India. We intend to share our experience of providing care for acute spinal disorders from 23rd March, 2020, when nationwide lockdown and closure of elective services started in our country, to till 12th May, 2020, and to formulate few recommendations at the end.
Setting
Northern India.
Methods
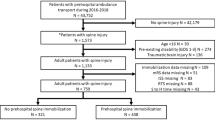
Between 23rd March, 2020 and 12th May, 2020, data of all patients with spinal conditions presenting to Emergency Department for acute care services were collected prospectively. Existing protocols were modified in line with changing national and institute policies for functionality of the spine unit, challenges faced and steps taken were noted.
Results
All elective cases were postponed for an indefinite period at the starting of ‘Lockdown’. A total of 24 patients were received in ED during study period and 14 (58%) were managed operatively. The majority (79%) were with traumatic spine injury, and fall from height was most common mechanism of injury in traumatic spine patients (84%). There was higher incidence of surgical site infections (14%) among operated patients, compared to our previous average. We had modified routine policies to tackle challenges faced and till date of writing this article, none of the members of spine team or patients treated by us tested positive for SARSCoV-2.
Conclusion
To continue providing care for acute spinal conditions and maintaining academic activities of spine unit during ‘lockdown’ needs innovative policies in line with national protocols.
Similar content being viewed by others
Introduction
SarsCoV-2 pandemic has affected and testified our healthcare system in many different ways. With the overwhelmed healthcare systems even in developed nations around the globe [1], it is imperative to state that this pandemic had influences on spine care services of our institute. Our understanding of the virus and of suggested measures to contain and treat the infection are not time-tested, resulting in frequent changes in protocols [2]. Moreover, sudden and strict nationwide ‘lockdown’ imposed further logistic issues that had to be addressed for uninterrupted spine care services.
We intend to share our experience of treating patients with spinal disorders in a tertiary care teaching hospital from 23rd March, 2020, when nationwide lockdown and closure of elective services started in our country, to now.
Materials and methods
Data of all patients who presented with spinal conditions to the Emergency Department (ED) of the institute between 23rd March, 2020 and 12th May, 2020 were collected prospectively and analysed. Particulars were collected in the form of mode of injury (in case of patients with traumatic spinal injuries), region of spinal column involved, type of pathology detected, neurological status of patients, type of management (operative/non-operative), and complications detected. Our ED team received all patients presented to ED wearing full Personal Protective Equipment (PPE), and any patient who required emergency surgical procedure was treated as potentially positive for SarsCoV-2 infection. Following surgery, both the patient and one of his/her attendants were subjected to Polymerase Chain Reaction (PCR)-based testing and they were managed in a dedicated COVID-building in isolation rooms. This was to ensure their status of infectivity before safely discharging them to the society. After availability of the negative COVID report, patients were shifted to main hospital building. If the patient had tested positive without clinical manifestation of the infection, they were managed in a dedicated COVID-building only and were discharged on advice for home-isolation. Healthcare Workers exposed to a COVID-positive patient were quarantined for two weeks in a dedicated centre with instruction for hospital visit should they develop any symptoms. Due to sudden cessation of all elective and outpatient services and nation-wide ‘lockdown’, our clinical pathways had to be changed significantly and were met with a number of challenges, which we have enumerated in a systematic way in the following section.
Challenges
Following enforcement of ‘lockdown’ and social distancing, unique problems were faced by our spine unit and we had to extensively modify our existing policies for hospital admissions, management protocols, discharge policies, and above all academic activities.
1) Due to readjustment in allotment of resources to various departments to develop a separate COVID-facility, we had to work with new teams and in a new set-up leading to curtailed efficiency of the team.
2) As all patients were being received in a common ED, decreasing the transit time of patients, as well as early decision-making and disposal, were mandatory for smooth functioning of that area.
3) The Operating Room (OR) allotted for emergency cases in COVID-building was suboptimal as compared to our routine Spine OR, as the former one lacked a number of specialized instruments, high-quality image intensifier and experienced human resources, all of which are necessary assets of an efficient spine team.
4) In the face of spreading infection across the country, there were obvious risks of both getting and transmitting the SARS-CoV-2 infection to the treating team and to the patients and their attendants during in-hospital treatment.
5) Due to redistribution of ICU beds and pooling of ventilators, availability of these resources was limited for the spine unit. It influenced surgical decision making for any new patient, who potentially required post-operative ICU or ventilator support.
6) As most of our patients who are on rehabilitation or who need bracing are followed up on OPD basis, and OPD services had been closed since the inception of the lockdown, proper rehabilitation of patients with spinal cord injury and availability of braces had to be ensured.
7) Getting proper orthopaedic implants in time was also cumbersome, as was the availability of customised braces, initially due to strong police-patrolling to restrict inter-state mobility, and consequent looming fear of coming to hospital premises among implant and orthotic
distributors.
8) To minimise contact of Health Care Workers with potentially infected patients, inter-departmental consultations were accomplished through video calls as much as possible.
9) Frequent changes in hospital protocols as per new guidelines had mandated parallel changes in clinical pathways of emergency spine cases leading to a state of confusion among residents. For example, there was dubiety in a number of occasions as to whether Orthopaedic surgeon or infectious disease specialist will be primary consultant-in-charge of any patient admitted with spinal disorder in the COVID building.
10) To continue with mandatory academic activities, maintaining social distancing was definitely demanding amidst this chaotic and terrible situation. For example, clinical case presentations for final-year postgraduate students had become an issue.
11) Time-bound research projects allotted to orthopaedic residents, especially those involving surgical interventions, had to be re-visited, owing to significant drop in number of cases being treated surgically and to growing uncertainty about the possible duration of ‘lockdown’.
Results
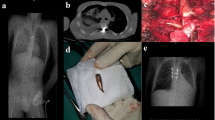
During the study period we had received a total of 24 patients with spinal pathologies in ED. Region- and pathology-wise distributions of these cases are enumerated in Table 1. Among four (04) cases that presented with infection, two were cases of early surgical site infections (SSI) requiring operative debridement. Both of these patients underwent index surgery during the study period only. Out of these, 14 patients were treated with surgical interventions. Operated patients were mobilised on the first post-operative day with brace support and were discharged on the fourth post-operative day with basic lessons of physiotherapy like mobilisation of all joints in bed, transfers in hospital with wheel chair, chest physiotherapy with incentive spirometer etc., to one of his/her family members. We encountered two cases of early post-operative SSI during this period, as stated earlier. This infection rate was much higher (two in 12 or 16.7%) than our previous deep infection rate (eight cases of deep infections requiring surgical debridement in 218 total operated cases or 3.67%, as per departmental adverse-event register), and this could presumably be attributed to sub-optimal conditions in OR and scarce experienced manpower. Most of the procedures performed were open surgeries (13 out of 14/92.8%) due to non-availability of MIS instrumentation during ‘lockdown’. Distribution of treatment modalities (operative/non-operative) and types of surgical procedures performed are shown in Table 1. Non-operatively treated cases (10) included two cervical (AO Type A0), five thoraco-lumbar AO Type A2, and three AO Type A3 spinal trauma without any neurological deficit (Fig. 1). They were kept admitted for 2/3 days and were discharged after application of brace and mobilisation as pain allows. Basic physiotherapy was taught to one of his/her attendants with advice for follow-up in case of deteriorating neurology or after lockdown was over. Among patients with traumatic spinal injuries (n = 19), 16 (84.2%) sustained injuries from fall from more than six-feet height, and only one case (5.3%) was due to Road-traffic accidents (RTA). This could be explained by the hilly geographic terrain of the state where vehicles falling into gorges is a common mode of sustaining injuries, and also by the fact that ‘lockdown’ had led to significantly decreased vehicular movement in the state. AIS grades of patients have been shown in Table 1.
Discussion
Our hospital had started mobilising resources since the detection of first case in India i.e. 30th January,2020. But sudden onset ‘lockdown’ initially created a situation of anxiety and uncertainty among healthcare workers of all levels. Though the unfortunate period continues, we recommend following measures which have helped us to steer through the crisis in various ways till now.
1) Mandatory enrolment of all Health Care Workers for COVID-preparedness workshops, that included general awareness programmes, workshops on basics of airway management and sessions on fundamentals of ECG interpretation and ventilator management, on online platforms. This made every health care professional feel more equipped with knowledge and skill to tackle the situation.
2) Strict adherence to personal protective measures like maintenance of hand-hygiene etc. was ensured by infection control team of the hospital.
3) Whatsapp-based sharing of clinical and radiological details of patients presented to ED with any acute spinal problems fostered urgent decision-making and expedited transit time thereon. This method of telecommunication for Orthopaedic consultation is also described recently in a body of literatures [3, 4].
4) For patients with spinal trauma with intact neurology, we ceased to get MRI routinely for treatment-decisions, which we used to practise otherwise previously. This reduced the transit time of patients in ED. Rajasekaran et al. in their work had concluded that they do “not support the need for routine MRI in patients for classification, assessing instability or need for surgery” in patients with thoraco-lumbar spine injuries [5]. However, we continued to get MRI before proceeding with surgery for any patient with incomplete spinal cord injury.
5) Decreasing the number of attendants to one per patient significantly reduced crowd in in-patient areas and also ensured proper screening.
6) With the availability of rapid tests, all patients, along-with one attendant for each, were subjected to COVID-19 testing before semi-emergency procedures and for all patients undergoing emergency surgery or for patients whose COVID-status was unknown, OR team had to mandatorily use full PPEs including face shield, shoe covers, cap, N95 respirator mask and fluid-impervious gowns.
7) Hospital administration in collaboration with state administration had started issuing travel passes for implant distributors so that they could reach the hospital in-time and keep the show going in the state of ‘lockdown’.
8) We started to develop hospital-based inventory for most commonly-used spinal implants eg, pedicle screw systems, anterior cervical plating system, lateral mass instrumentation system with multiple sets of commonly used sizes, to decrease lesser hospital visits by implant vendors.
9) To decrease surgical time and to decrease high-risk behaviours (e.g. deliberate use of electro-cautery, over-crowding of OR) that might spread the infection among residents and OT staffs, presence of consultant during surgery was mandatory as per policy of the unit. Moreover, operating with personal protective equipments is technically a more difficult job and hence presence of unit chief during surgery acted both to alleviate fears among residents working in this difficult time and to smoothen the whole process.
10) Six persons were allowed inside including personnel from the surgical, anaesthesia, technician and nursing teams.
11) To decrease hospital stay, patients were discharged on an accelerated protocol and attached to community hospitals, nearby to their hometown for further post-operative care and were advised to report if they needed any urgent care. Every possible effort was made to take care of perioperative pain including sub-fascial para-spinal blocks, local anaesthetic infiltration and pre-emptive analgesia to facilitate early discharges.
12) Regular telephonic follow-up was continued regarding status of surgical site and feasibility of physical therapy at home. This type of follow-up is not a routine in our setup due to a high volume of patients we had to attend; but due to a lesser number of patients it was possible, and both the early post-operative infections were suspected on telephonic conversation, and patients were then called for urgent hospital visit and early debridement.
13) All academic activities were gradually shifted from classroom presentations to online platforms. This again helped in two ways. Firstly, and obviously, it decreased social gathering, and secondly, it paved the way for a more informal interaction between residents and faculties, that certainly acted as a morale-booster for orthopaedic and trauma residents who were working in the frontline amid panic and uncertainty.
14) Time-bound research projects were being revisited in view of unforeseeable continuation of current situation, and shorter projects, based on retrospective methodology, were being allotted to those who were about to end their tenure. Researchers have tried to formulate guidelines regarding indications for spine surgeries during these difficult times, but triaging of cases needs to be done as per resources available, especially in resource-scarce countries [6, 7]. Meyer et al. has shown preponderance of degenerative and tumour cases and a steep decrease in trauma cases [8], whereas most of our patients were of traumatic spine injuries, the most common mechanism being fall from height. This discrepancy can be explained by different socio-economic conditions and hilly terrain in this part of the world. This pandemic is certainly proving itself as one of the most difficult times for us as part of medical fraternity [9], as well as the human race. But our capacity to work in tandem with our infectious disease specialist colleagues or medical colleagues is being proven in this critical period.
Conclusion
As part of spine unit, we must remain vigilant to restrict numbers of admissions, procedures and days in hospital to minimise chance of contacts. At the same time, we have to maintain the morale of our colleagues. Doing so may sometimes need innovative measures pertinent to that socio-economic scenario. As uncertainty still prevails regarding the probable duration of this pandemic, repeated evaluation and modification of our existing policies as a team seems prudent.
Data availability
Within the published paper.
References
“Home | Ministry of Health and Family Welfare | GOI”. mohfw.gov.in. Accessed 12 May 2020.
Vaishya R, Vaish A. Roles and responsibilities of the orthopaedic community and the society during COVID-19 pandemic [published online ahead of print, 2020 Apr 14]. Indian J Orthop. 2020;1–2. https://doi.org/10.1007/s43465-020-00105-7.
Khanna V, Sambandam SN, Gul A, Mounasamy V. “WhatsApp”ening in orthopedic care: a concise report from a 300-bedded tertiary care teaching center. Eur J Orthop Surg Traumatol. 2015;25:821–6. https://doi.org/10.1007/s00590-015-1600-y.
Giordano V, Koch HA, Mendes CH, Bergamin A, de Souza FS. Whatsapp messenger is useful and reproducible in the assessment of tibial plateau fractures: inter- and intra-observer agreement study. Int J Med Inform. 2015;84:141–8.
Rajasekaran S, Vaccaro AR, Kanna RM. The value of CT and MRI in the classification and surgical decision-making among spine surgeons in thoracolumbar spinal injuries. Eur Spine J. 2017;26:1463–9. https://doi.org/10.1007/s00586-016-4623-0.
Donnally CJ 3rd, Shenoy K, Vaccaro AR, Schroeder GD, Kepler CK. Triaging spine surgery in the COVID-19. Era Clin Spine Surg. 2020;33:129–130. https://doi.org/10.1097/BSD.0000000000000988.
Zou J, Yu H, Song D, Niu J, Yang H. Advice on standardized diagnosis and treatment for spinal diseases during the coronavirus disease 2019 pandemic. Asian Spine J. 2020;14:258–263. https://doi.org/10.31616/asj.2020.0122.
Meyer M, Prost S, Farah K, Denis JB, Dufour H, Blondel B et al. Spine surgical procedures during coronavirus disease 2019 pandemic: is it still possible to take care of patients? results of an observational study in the first month of confinement. Asian Spine J. 2020. https://doi.org/10.31616/asj.2020.0197.
Viswanath A, Monga P. Working through the COVID-19 outbreak: rapid review and recommendations for MSK and allied heath personnel. J Clin Orthop Trauma. 2020;11:500–503. https://doi.org/10.1016/j.jcot.2020.03.014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sarkar, B., Dubey, S., Goyal, N. et al. Acute spine care services during covid-19 pandemic and ‘lockdown’: case series and our perspective from a level 1 trauma centre. Spinal Cord Ser Cases 8, 3 (2022). https://doi.org/10.1038/s41394-021-00471-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00471-w