Abstract
Introduction
This is a 20-year-old wheelchair athlete with history of caudal regression syndrome and cervical canal stenosis who developed spinal segmental myoclonus following routine intubation for an elective procedure.
Case presentation
This patient is a 20-year-old man with history of caudal regression syndrome and chronic cervical stenosis. He is a high-level wheelchair racer and paralympic hopeful. This patient initially presented 18 months prior with shoulder abduction weakness. He was found to have cervical stenosis at C4, C5 on MRI. Neurosurgical treatment was not needed at that time as symptoms resolved. On this encounter, he presented for an elective urologic surgical procedure. Glidescope intubation was performed with notable cervical extension. In the Post Anesthesia Care Unit, the patient began experiencing twitching movements in his pectoral muscles bilaterally as well as left deltoid and biceps. His findings were consistent with myoclonus due to his cervical myelopathy. He was initially started on levetiracetam, but experienced dizziness. His symptoms were finally controlled with clonazepam. Neurosurgery performed cord decompression and fusion with resolution of his symptoms.
Discussion
There are few cases of myoclonus secondary to myelopathy documented in literature. The current recommended treatments, levetiracetam and/or benzodiazepines, were successful in managing the myoclonus in this patient. However, cord decompression is necessary to avoid progression of myelopathic symptoms. In conclusion, myoclonus can be a presenting symptom of myelopathy and warrants further investigation, especially in patients with known spinal cord or vertebral pathology.
Similar content being viewed by others
Introduction
Myoclonus is an involuntary jerking of the muscles, either rhythmic, or arrhythmic. It is commonly associated with brain lesions; however, a rare subtype of myoclonus, spinal myoclonus, occurs in muscle groups supplied by one or a few contiguous segments of the spinal cord [1]. Spinal cord pathologies associated with myoclonus include tumors, lumbar radiculopathy, and myelopathy, among others [1].
Regarding myelopathy as a cause, there are few documented cases in the literature. Most of the reported patients are adults in their fifth to eighth decades of life with central canal stenosis or cord compression due to disc herniation or cervical spondylosis [2,3,4]. To our knowledge, outside of compression due to spinal tumors, there are very few pediatric cases of spinal myoclonus due to myelopathy in the literature. We present one such case below in which a patient with known chronic central canal stenosis and cord compression developed acute myelopathy with segmental spinal myoclonus.
Case presentation
The patient is a 20-year-old male with a past medical history of sacral agenesis, paraplegia, neurogenic bowel, neurogenic bladder, imperforate anus, previous bladder rupture, anxiety, autofusion of C2–C3, rotatory levoscoliosis of the lower cervical spine, thoracic dextroscoliosis with 41 degree curvature, chronic tethered spinal cord, cervical central canal stenosis affecting C4, C5, and increasing cervical kyphosis causing progressive unroofing of the facets. With reference to the ASIA/ISCoS International Standards for Neurological Classification of Spinal Cord Injury, he is a low-thoracic ASIA A. He also has an extensive surgical history which notably includes: sigmoid colostomy, bladder neck reconstruction and fascial sling, Mitrofanoff, bladder rupture repair, and multiple orthopedic procedures to his lower extremities. His baseline level of function is independent with ADLs, including bowel and bladder management with Mitrofanoff and colostomy, as well as independence with transfers. For many years, he has competed in wheelchair racing and is a Paralympic hopeful. It is important to note that bowel and bladder management for this patient require adequate neck flexion for visualization and wheelchair racing requires a high degree of neck extension for proper posture and visibility.
Prior to this admission, the patient developed proximal left upper limb weakness, specifically shoulder abduction, internal rotation, external rotation, and elbow flexion, after doing ~75 triceps dips. X-ray and MRI of this shoulder were normal. Additionally, MRI cervical spine at this time redemonstrated known autofusion of C2–C3, central canal stenosis, previously measured to be 7.5–8.5 mm anterior to posterior, at C4/C5 and C5/C6 as well as new increased T2 cord signal at C4, and cervical kyphosis with apex at C4/C5. He was treated with a short course of corticosteroids and home exercise program which did not resolve his weakness. On exam by PM&R Sports, C5 myotomal weakness was noted and he was referred for a nerve conduction study and electromyography (NCS/EMG). This demonstrated decreased recruitment and reduced interference pattern on needle EMG of the left C5 myotome with normal insertional activity in the middle left cervical paraspinals; indicating a central source consistent with the patient’s known central canal stenosis. He was seen by neurosurgery who scheduled him for surgical decompression. In the interim, the patient had physical therapy for scapular and shoulder muscle strengthening with eventual resolution of his symptoms. Therefore, our patient and his physicians chose not to proceed with his scheduled surgery. He returned to full participation competing in collegiate wheelchair racing.
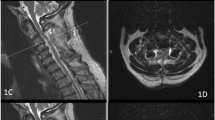
Eleven months after that episode, our patient was in his usual state of health when he presented for elective admission for urologic procedures under general anesthesia. Per anesthesia reports, the patient’s airway was not difficult and there were no complications. However, upon waking in the Post Anesthesia Care Unit, he noted repetitive twitching movements of his chest bilaterally. He was admitted and his chest twitching persisted through hospital day 1. It was noted to be rhythmic with a frequency of about 1 Hz and involved his pectoralis muscles bilaterally as well as his left biceps and deltoid. In this case, the patient’s twitching did not go away with intentional movement. Additionally of note, the movement was not present during sleep. An MRI cervical spine (Fig. 1) showed worsening cervical kyphosis and moderate cord compression with persistent T2 hyperintense signal abnormality noted at C4. He was diagnosed with segmental spinal myoclonus based on his presentation and imaging. NCS/EMG was not performed. Medical management was started with levetiracetam and IV steroids. Benzodiazepines were discussed with the patient, however, he had a history of adverse side effects with lorazepam in the past and elected to try levetiracetam first. The levetiracetam did not provide relief from the myoclonus and therefore midazolam was trialed. He did have some relief with midazolam and then agreed to try clonazepam which did manage his symptoms for a longer duration.
He remained on a stable dose of clonazepam for symptom management until readmission for scheduled posterior C3–6 laminectomy and fusion 4 weeks after symptom onset. Postoperatively, he experienced weakness in his left hand intrinsics and shoulder girdle as well as musculoskeletal neck pain and nerve pain primarily in the left hand. His acute postoperative pain was managed with IV opioid medication and gabapentin. He was discharged with scheduled gabapentin, a decreased dose of scheduled clonazepam and prn hydrocodone/acetaminophen.
This patient was followed in neurosurgery clinic at 3 weeks, 6 weeks, 12 weeks, and 6 months postoperation. His C-collar was cleared at 12 weeks. He has an additional neurosurgery follow up scheduled at the 12 month postoperative mark. Additionally, he was referred for outpatient occupational/hand and physical therapy with the following precautions: c-collar at all times and no flexion or extension of his neck. Therapies started at 4 weeks postoperation and focused on strengthening, shoulder stability, range of motion, and proprioception using targeted exercises, electrical stimulation, and cardio training. For safety reasons, cardio training began on a hand cycle. At 12 weeks postoperation, the patient was cleared for slow progression of weight lifting and wheelchair racing. Sport-specific training was started on a roller as the postoperative restrictions prohibited the patient from extending his neck adequately for safe racing chair ambulation on a road. He demonstrated a steady improvement in muscle strength and hand function, but still had deficits in shoulder external rotation at the time of this report. Electrical stimulation has been focused on the infraspinatus for neuromuscular reeducation. The patient’s postoperative neck range of motion has not yet been tested, but it is expected that some flexion and extension range has been lost as the majority of this motion occurs at C4–C6, which have now been fused [5]. However, it is important to note, he remains independent with bowel and bladder management postoperatively.
Discussion
In the setting of acute on chronic cervical myelopathy, our patient displayed rhythmic jerking of bilateral pectoralis muscles as well as the left deltoids and biceps with a frequency of ~1 Hz. This presentation is most consistent with segmental spinal myoclonus.
Spinal myoclonus, as described above, is a subtype of myoclonus and is characterized by involuntary movements in the myotome(s) of one to a few segments of the spinal cord. It can be further divided into segmental spinal myoclonus and proprioceptive spinal myoclonus based on the spinal cord segments affected [6]. Segmental spinal myoclonus, as seen in our patient, involves myotomes from one to a few contiguous spinal cord levels, in this case bilateral C5 myotomes. Proprioceptive spinal myoclonus is a rare condition involving multisegmental myotomes of the limbs and trunk and is mediated by intersegmental fibers [3].
In the case of segmental spinal myoclonus, most sources agree it is not usually affected by external sensory stimuli, but is often affected by a patient’s emotional stress or fatigue. Though our patient does have a history of anxiety disorder, it did not seem to play a role in his myoclonus as his symptoms began upon awakening from anesthesia and persisted at the same frequency or decreased frequency throughout his hospitalization. Though this may have been obscured by his treatment with clonazepam. In addition, it was noted that our patient’s symptoms resolved during sleep. There is variability in the literature as some sources cite the absence of spinal myoclonus in sleep and others report that it persists [1, 2, 6].
Several medications have been used, off-label, in the management of myoclonus including levetiracetam, sodium valproate, piracetam, and clonazepam [7]. However, there is a lack of studies regarding efficacies of these medications for myoclonus and to guide its treatment. Some literature suggests that a combination of medications may be needed [8]. However, clonazepam monotherapy has been documented to manage symptoms adequately; as was the case for our patient [4, 9]. Although, cervical decompression surgery was needed to ultimately prevent further complications and loss of upper limb function in this case.
As noted above, most of the cases in the literature involve older patients with cervical spondylosis or chronic central canal stenosis due to degenerative changes. It is well documented that central canal stenosis or cord:canal mismatch, meaning a high ratio of space the spinal cord occupies compared to space available in the canal, can predispose individuals to cord compression and spinal cord injury resulting from even minor trauma [10, 11]. This ratio can also be expressed as the spinal cord occupation ratio or SCOR. Studies have found that a SCOR ≥ 70% can predispose a patient to cord compression and myelopathy [10, 11]. Additionally, patients with congenital stenosis seem to be at greater risk than those with a degenerative etiology [11]. Though a SCOR percentage was not calculated for our patient, he does have several notable spine abnormalities including a rotatory levoscoliosis of his lower cervical spine, dextroscoliosis of his thoracic spine, cervical kyphosis, and chronic tethered spinal cord. It seems likely that due to his anatomy, he was at greater risk for cervical myelopathy from the hyperextension required for routine intubation. The first symptom of this was his segmental spinal myoclonus.
In summary, this 20-year-old wheelchair athlete with sacral agenesis, chronic tethered spinal cord, and multiple bony spinal abnormalities developed segmental spinal myoclonus as the primary presenting symptom of acute cervical myelopathy. This presentation has been described in the literature, albeit sparsely. However, it has not been described, to our knowledge, in a patient of this age and functional level. Segmental myoclonus should not be overlooked as a potential symptom of myelopathy, especially in patients with known risk factors for myelopathy, recent history of minor trauma or even routine manipulation of their neck, and new upper limb findings. Close monitoring of symptom progression and surgical intervention may be needed to preserve function and alleviate symptoms.
References
Jankovic J, Pardo R. Segmental myoclonus: clinical and pharmacologic study. Arch Neurol. 1986;43:1025–31.
Daniel DG, Webster DL. Spinal segmental myoclonus: successful treatment with cervical spinal decompression. Arch Neurol. 1984;41:898–9.
Christodoulidea I, Giamouriadis A, Bashford J, Barkas K. Spinal myoclonus: a rare presentation of cervical myelopathy. BMJ Case Rep. 2018. https://doi.org/10.1136/bcr-2018-225455.
Lee CN, Baek SH, Park KW, Kim BJ. Hiccup-like segmental mycolonus in thoracic compressive myelopathy: a case report. Spinal Cord. 2014;52:S16–8.
Lind B, Sihlbom H, Nordwall A, Malchau H. Normal range of motion of the cervical spine. Arch Phys Med Rehabil. 1989;70:692–5.
Eberhardt O, Topka H. Myoclonic disorders. Brain Sci. 2017;7:103.
Jankovic J. Treatment of hyperkinetic movement disorders. Lancet Neurol. 2009;8:844–56.
Stahl C, Frucht S. An update on myoclonus management. Expert Rev Neurother. 2019;19:325–31.
Boudier-Revéret M, Chang MC. Segmental spinal myoclonus following a cervical transforaminal epidural steroid injection: a case report. Am J of Phys Med Rehabil. 2020. https://doi.org/10.1097/PHM.0000000000001414.
Nouri A, Montejo J, Sun X, Virojanapa J, Kolb L, Abbed K, et al. Cervical cord-canal mismatch: a new method for identifying predisposition to spinal cord Injury. World Neurosurg. 2017;108:112–7.
Nouri A, Tetreault L, Nori S, Martin AR, Nater A, Fehlings MG. Congenital cervical spine stenosis in a multicenter global cohort of patients with degenerative cervical myelopathy: an ambispective report based on a magnetic resonance imaging diagnostic criterion. Neurosurgery. 2018;83:521–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pristas, N., Klamar, K., Napolitano, J. et al. Acute on chronic cervical myelopathy causing cervical segmental myoclonus in a high-level wheelchair athlete: a case report. Spinal Cord Ser Cases 7, 90 (2021). https://doi.org/10.1038/s41394-021-00453-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00453-y
This article is cited by
-
Levetiracetam
Reactions Weekly (2022)