Abstract
Introduction
Virtually every person with a spinal cord injury (SCI) suffers from a neurogenic lower urinary tract dysfunction (NLUTD). In the long term, about 15% of persons with SCI depend on indwelling (suprapubic or transurethral) catheters for bladder management. About 50% of these patients suffer from catheter encrustation and blockage, which may become a vital threat for persons with SCI, as it can lead to septicemia or autonomic dysreflexia. Until today, no prophylaxis of catheter encrustations with an evidence-based proof of efficacy exists.
Case presentation
The homeopathic remedy Hydrastis, made from the goldenseal root, is used for the treatment of thick, mucous urine sediment. In four patients with tetraplegia (three female, one male) who managed NLUTD by suprapubic catheters, recurrent encrustations and catheter blockage occurred despite irrigation and medical treatment. Surgical urinary diversion was envisioned. Applying Hydrastis C30 once weekly as a long-term medication, in three of the four patients, catheter obstructions ceased, with a follow-up for at least 1 year. One patient is awaiting ileal conduit surgery.
Discussion
According to the results of our case series, the application of Hydrastis seems to be beneficial in the prevention of encrustations of indwelling catheters in patients with SCI. As the treatment was effective and well tolerated, the problem is frequent, and effective solutions are scarce, a prospective trial seems justified.
Similar content being viewed by others
Introduction
Virtually every person with a spinal cord injury (SCI) suffers from a neurogenic lower urinary tract dysfunction (NLUTD) [1]. Especially in patients with a suprasacral SCI, the combination of detrusor-sphincter dyssynergia and detrusor overactivity frequently leads to elevated intravesical pressures during urine storage and voiding, with a high risk for subsequent renal damage [1]. Standard treatment of NLUTD consist of suppression of detrusor overactivity, combined with bladder evacuation by intermittent catheterization (IC). However, due to the loss of manual dexterity, the general state of health or the psychic situation, about 15% of the persons with SCI depend on indwelling (suprapubic or transurethral) catheters in the long-term [2]. Indwelling catheters carry several long-term risks, with encrustation and bladder stone formation being the complications with the highest negative impact on the quality of life of the affected persons [3]. About 50% of all patients with long-term indwelling catheters suffer from these problems [4]. Catheter blockage may become a vital threat for persons with SCI, as it can lead to septicemia or autonomic dysreflexia (A.D.) [5]. Therefore, an immediate intervention is mandatory, leading to stress and additional costs.
Thus, prophylaxis of catheter encrustations would be desirable. However, until today, no technique with an evidence-based proof of efficacy exists [6].
The homeopathic remedy Hydrastis canadiensis is made from the goldenseal root. In homeopathy, it is used, among other indications, for thick, ropy mucous urine sediment [7]. Therefore, we used this medication in patients with recurrent catheter obstructions due to encrustation in which other conservative means failed and surgical urinary diversion was envisioned.
Case presentation
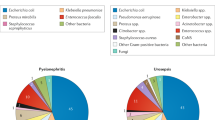
Four patients with SCI with long-term suprapubic catheters, in which standard preventive measures for catheter blockage were not successful, were included in this case series. All patients received Hydrastis C30 (Homöosana, Zug, Switzerland), five globules, and dissolved in one glass (200 ml) of water. Patients were instructed to take one sip of this solution three times daily in week 1, and two times daily in week 2. They prepared the solution at the morning of the respective day, stirred it directly prior to use and used the solution for the entire day. After week 2, patients used Hydrastis once a week as a constant long-term medication. Medication related to bladder management and UTI prophylaxis as well as the bacterial strains detected in the urine of all patients included are listed in Table 1. The local ethics committee approved retrospective data collection.
Case 1
A 34-year-old woman suffered from an incomplete tetraplegia below C4, ASIA impairment score (AIS) C, in July 2009. Due to a traumatic brain injury and impaired manual dexterity, a 14 French suprapubic catheter was inserted in August 2009. The catheter was not clamped, but drained constantly. Since 2015, frequent encrustations with recurrent catheter blockage, leading to acute urinary retention and A.D., occurred. Fluid intake was 1.5 L/24 h. Cystoscopy did not reveal a reason for the encrustations, which persisted despite urine acidification, bladder irrigation with water or citric acid, and the use of a triclosan-containing solution in the catheter balloon. As a consequence, the catheter was changed every 2 to maximum 4 weeks. Thus, we discussed ileal conduit urinary diversion due to repetitive life-threatening A.D. with massive hypertension. As a last option, we used Hydrastis as described above. Since 2017, no catheter obstruction with urinary retention recurred, and the intervals for catheter changes were expanded to every 6 weeks. In addition, the patient reported that the urine was less cloudy and less malodourous. As due to the absence of catheter obstruction, not further episodes of A.D. occurred, the patient elected to continue bladder management by a suprapubic catheter, and ileal conduit diversion was not performed. Fluid management and medication did not change over time. Renal function, assessed by serum cystatin C and renal ultrasound, remained unimpaired until today.
Case 2
Following a car accident in January 2017, a 63-year-old woman developed an incomplete tetraplegia below C4 (AIS C). As neither reflex voiding nor IC could be established, a 12 French suprapubic catheter was inserted 5 months after SCI. She clamped the catheter and emptied the bladder 6 times daily. As urinary retention due to a blocked catheter occurred every 2 weeks, she irrigated the bladder with saline twice daily, and a 14 French catheter was inserted. Despite these measures, the patient developed a bladder stone, which was not present at the time of catheter insertion and was endoscopically removed in March 2018. In April 2018, Hydrastis was started, and until the death of the patient, unrelated to NLUTD, in July 2020, merely two emergency changes of the catheter became necessary. Renal function, assessed by serum cystatin C and renal ultrasound, remained unimpaired during the entire follow-up. As the bladder stone developed in a time period in which the catheter was frequently obstructed, it seemed to be rather a consequence than an immediate cause of the encrustations. Therefore, besides stone removal, the Hydrastis treatment led to the distinct clinical improvement described above.
Case 3
After a mountain bike accident in 2007, a 36-year-old woman suffered from a complete tetraplegia below C6 (AIS A). For bladder management, a 14 French suprapubic catheter was inserted, which was constantly draining. The catheter was changed every 4–5 weeks. In 2014, she developed detrusor overactivity and a third degree vesico-renal reflux to the left kidney, which were treated by onabotulinum toxin injection in the detrusor and bulking agents, respectively. Despite the treatment, detrusor overactivity with massive A.D. persisted. In the same year, a small bladder tumor was detected at the left bladder wall. After transurethral resection, histologic examination revealed squamous metaplasia without signs of malignancy. In 2019, obstruction of the suprapubic catheter occurred every 2 weeks despite urine acidification and daily irrigation with saline. In May 2019, a bladder stone was excluded by cystoscopy, and Hydrastis treatment was commenced. The medication was well tolerated, but until the most recent follow-up (11/2020), catheter encrustations remained unaltered, requiring catheter changes every 1–2 weeks. The patient is currently awaiting ileal conduit urinary diversion, partly due to the recurrent encrustations, partly due to the massive loss of bladder capacity (<50 ml), which complicates bladder management. Fortunately, renal function, assessed by serum cystatin C and renal ultrasound, remained unimpaired until today.
Case 4
A 26-year-old male patient suffered from a complete tetraplegia sub C4 after a motorcycle accident in 2007. Due to a urethral stricture as a consequence of an urethral lesion, a suprapubic 14 French catheter was inserted in 2008, which was not clamped and which was changed every 6 weeks. In 2018, malodorous urine and repetitive catheter obstructions occurred, which persisted despite urine acidification, bladder irrigation, and vitamin C treatment. Cystoscopy excluded bladder stones or tumors. After Hydrastis treatment was commenced, both catheter encrustations and malodorous urine did not recur until the most recent follow-up (11/2020). No side effects related to the medication were reported, renal function, assessed by serum cystatin C and renal ultrasound, remained unimpaired until today.
Discussion
In this case series, we present a new, promising, noninvasive treatment option for catheter encrustations in patients with long-term indwelling catheters.
Obstruction of indwelling catheters is a frequent complication. About 50% of long-term catheterized patients develop catheter encrustations that can block the lumen of the catheter [8]. In patients with SCI, urinary retention despite a catheter in place is not merely bothersome, but may have fatal consequences due to e.g., A.D. [5]. Colonization of indwelling catheters with microorganisms seems to be the most important causative factor for catheter encrustation. The microorganisms produce a biofilm, made up of proteins, electrolytes, and other components of urine on the surface of the catheter [9]. Bacteria can attach to this film and secrete polysaccharides that form the architectural structure of biofilm. The combination of bacteriuria and biofilm formation leads to the production of urease, which hydrolyzes urea in the patient’s urine to ammonium hydroxide. The resulting alkaline environment leads to precipitation of salts that can encrust and block the lumen of the catheter.
As the only causal treatment would be a bladder management without an indwelling catheter, in persons requiring a catheter for long-term urinary drainage merely symptomatic treatment is possible. Unfortunately, there is no ideal preventive measure. Current concepts rely either on cleansing or on dissolving deposits in the bladder, on eradication of crystal-forming bacteria or on decreasing biofilms on the catheter surface.
Cleansing or dissolving deposits
Catheter clamping and emptying the bladder via the catheter at regular intervals seems to be beneficial regarding catheter encrustation [10]. The patients included in this case series, however, all suffered from a tetraplegia, with the risk of A.D. triggered by a full bladder. As patients with tetraplegia often lack the dexterity to open the catheter valve without help, catheter clamping poses an additional risk on the affected persons and is not advised, especially as it does not seem to be beneficial concerning bladder capacity or compliance [11].
Bladder irrigation relies either on mechanical cleansing (e.g., with saline solution) or on dissolving the intravesical crystals, as e.g., citric acid containing solutions [12]. Although in vitro experiments demonstrated that acidic solutions were more effective against encrustations than saline [12], in a randomized prospective trial in patients, no significant differences were detected. Increased fluid intake with citrated drinks has also been described as helpful [13].
Eradication of bacteria
As there is strong evidence that Proteus mirabilis bacteriuria is the main cause of the crystalline biofilms that encrust indwelling catheters [13], long-term eradication of bacteria from the urine would be a reasonable therapeutic option. However, in patients with indwelling catheters, this is virtually impossible [14]. The use of long-term antibiotics is not effective, and furthermore carries the risk of selecting multiresistant bacteria [15]. Triclosan-containing liquids for the inflating balloon demonstrated a certain antimicrobial effect, but already bacterial resistance against this substance has been described [16, 17]. In addition, based on in vitro and animal studies, a correlation between the chronic use of this substance and cancer risk is discussed, but data in humans are not available [18]. Applying a catheter coating with bacteriophages seems to be a promising innovative way to prevent proteus growth [19], but until today experience is limited to in vitro data, and handling of bacteriophages requires strict security measures.
Decreasing biofilms
In vitro experiments demonstrated promising results for a silver-polytetrafluoroethylene nanocomposite catheter coating, [20]. Applying electric current to catheters with silver electrodes can also decreased encrustation rates [21], but clinical results are pending for both measures. In summary, no strategy with evidence-proven efficacy and tolerability exists [22].
To prevent encrustation, we applied Hydrastis as a homeopathic remedy. In homeopathy, Hydrastis Canadensis, derived from the goldenseal root, is used for the treatment of thick, yellowish, stringy discharge in the urinary tract [7], which closely resembled the encrustations that block the catheters. Homeopathic drugs are produced by potentization, i.e., by succussing and diluting the original substance. The higher the potency, the higher the dilution; a C30 potency means that no molecule of the original substance can be traced in the remedy applied. Despite this fact, reproducible effects of these drugs have been demonstrated in numerous studies [23], and severe side effects are rare. In our series, three out of four patients otherwise awaiting major surgery (urinary diversion) benefitted from the treatment without any side effects.
Although the results of our case series are promising, several drawbacks are present. First of all, the number of included persons is small, and no control group is present; the patients serve as their own control. Furthermore, the duration of the treatment effect is unclear, and, as the exact mode of action of homeopathy needs to be further elucidated [24], there is no sound pathophysiologic explanation for the effect observed. As the treatment was well tolerated, the problem is frequent, and effective solutions are scarce, a prospective trial seems justified despite the mentioned limitations.
In conclusion, based on the results of our case series, the use of the homeopathic drug Hydrastis seems to be beneficial in the prevention of encrustations of indwelling catheters in patients with SCI. As the treatment was effective and well tolerated, the problem is frequent, and effective solutions are scarce, a prospective trial seems justified.
References
Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross T, Hamid R, et al. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur Urol. 2016;69:324–33.
Krebs J, Wöllner J, Pannek J. Bladder management in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord. 2016;54:609–13.
Nomura S, Ishido T, Teranishi J, Makiyama K. Long-term analysis of suprapubic cystostomy drainage in patients with neurogenic bladder. Urol Int. 2000;65:185–9.
Feneley RC, Kunin CM, Stickler DJ. An indwelling urinary catheter for the 21st century. BJU Int. 2012;109:1746–9.
Vaidyanathan S, Soni BM, Hughes PL, Oo T. Fatal cerebral hemorrhage in a tetraplegic patient due to autonomic dysreflexia triggered by delay in emptying urinary bladder after unsuccessful intermittent catheterization by carer: lessons learned. Int Med Case Rep J. 2018;11:53–8.
Sinclair L, Hagen S, Cross S. Washout policies in long-term indwelling urinary catheterization in adults: a short version cochrane review. Neurourol Urodyn. 2011;30:1208–12.
Jus MS. Hydrastis Canadensis. In: Jus MS, editor. Praktische Materia Medica. 3rd ed. Zug: Homöosana; 2009. p. 938–43.
Getliffe KA. Bladder instillations and bladder washouts in the management of catheterized patients. J Adv Nurs. 1996;23:548–54.
Jamal M, Ahmad W, Andleeb S, Jalil F, Imran M, Nawaz MA, et al. Bacterial biofilm and associated infections. J Chin Med Assoc. 2018;81:7–11.
Sabbuba NA, Stickler DJ, Long MJ, Dong Z, Short TD, Feneley RJC. Does the valve regulated release of urine from the bladder decrease encrustation and blockage of indwelling catheters by crystalline proteus mirabilis biofilms? J Urol. 2005;173:262–6.
Pannek J, Göcking K, Bersch U. To clamp or not to clamp? Bladder management by suprapubic catheterization in patients with neurogenic bladder dysfunction. World J Urol. 2010;28:637–41.
Getliffe KA. The use of bladder wash-outs to reduce urinary catheter encrustation. Br J Urol. 1994;73:696–700.
Stickler DJ, Feneley RCL. The encrustation and blockage of long-term indwelling bladder catheters: a way forward in prevention and control. Spinal Cord. 2010;48:784–90.
Warren JW, Anthony WC, Hoopes JM, Muncie HL. Cephalexin for susceptible bacteriuria in afebrile, long-term catheterized patients. JAMA. 1982;248:454–8.
Laxminarayan R, Duse A, Wattal C, Zaidi AKM, Wertheim HFL, Sumpradit N, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13:1057–98.
Belfield K, Betts H, Parkinson R, Bayston R. A tolerability and patient acceptability pilot study of a novel antimicrobial urinary catheter for long-term use. Neurourol Urodyn. 2019;38:338–45.
Westfall C, Flores-Mireles AL, Robinson JI, Lynch AJL, Hultgren S, Henderson JP, et al. The widely used antimicrobial Triclosan induces high levels of antibiotic tolerance in vitro and reduces antibiotic efficacy up to 100-fold in iivo. Antimicrob Agents Chemother. 2019;63:e02312–8.
Dinwiddie MT, Terry PD, Chen J. Recent evidence regarding triclosan and cancer risk. Int J Environ Res. Public Health. 2014;11:2209–17.
Milo S, Hathaway H, Nzakizwanayo J, Alves DR, Pérez Esteban P, Jones BV, et al. Prevention of encrustation and blockage of urinary catheters by Proteus mirabilis via pH-triggered release of bacteriophage. J Mater Chem B. 2017;5:5403–11.
Wang L, Zhang S, Keatch R, Corner G, Nabi G, Murdoch S, et al. In-vitro antibacterial and anti-encrustation performance of silver-polytetrafluoroethylene nanocomposite coated urinary catheters. J Hosp Infect. 2019;103:55–63.
Chakravarti A, Gangodawila S, Long MJ, Morris NS, Blacklock ARE, Stickler DJ. An electrified catheter to resist encrustation by Proteus mirabilis biofilm. J Urol. 2005;174:1129–32.
Smith JM. Indwelling catheter management: from habit-based to evidence-based practice. Ostomy Wound Manag. 2003;49:34–45.
Endler PC, Bellavite P, Bonamin L, Jäger T, Mazon S. Replications of fundamental research models in ultra high dilutions 1994 and 2015-update on a bibliometric study. Homeopathy. 2015;104:234–45.
Jonas WB, Kaptchuck TJ, Linde K. A critical overview of homeopathy. Ann Intern Med. 2003;138:393–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pannek, J., Pannek-Rademacher, S. Usefulness of Hydrastis for the prevention of encrustation of long-term indwelling catheters in persons with neurogenic bladder dysfunction: a case series. Spinal Cord Ser Cases 7, 66 (2021). https://doi.org/10.1038/s41394-021-00433-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00433-2