Abstract
Study design
Sub-study of a randomized controlled trial.
Objectives
To examine if hybrid cycling (cycling with the legs via electrical stimulation combined with voluntary handcycling) compared to handcycling leads to different systemic vascular adaptations in individuals with a long-term spinal cord injury (SCI).
Setting
Two rehabilitation centers in the Netherlands.
Methods
Ten individuals with a SCI trained on a hybrid bicycle (N = 5) or a handcycle (N = 5) for 16 weeks twice a week. Prior to and following the training the intima media thickness (IMT) of the common coronary artery (CCA) and superficial femoral artery (SFA) were measured and the flow-mediated dilation (FMD) of the brachial artery (BA) was analyzed.
Results
Before training, there were no significant differences in any of the outcome measures between the groups. We found no change in CCA IMT (pre: 0.616 mm, post: 0.586 mm), or in SFA (pre: 0.512 mm, post: 0.520 mm) after hybrid cycling. We also found no change in FMD % of BA after hybrid cycling (pre: 9.040%, post: 9.220%). There were no changes in CCA IMT, SFA IMT, and FMD% after handcycling either.
Conclusions
It appears that 16 weeks of twice-weekly training of up to 30 min on a hybrid bicycle or handcycle does not lead to systemic vascular adaptations. A larger sample size and training protocol with more frequent and higher intensity training (which might involve a home-based setting and an adapted period prior to the training) might show different results.
Similar content being viewed by others
Introduction
Provision of interventions that improve vascular adaptation is highly relevant given the high mortality and morbidity of cardiovascular disease (CVD) and cerebrovascular disease, particularly among individuals with spinal cord injury (SCI). The prevalence of the cardiovascular disease is 17% in people with a SCI compared to 5% in individuals without a SCI [1,2,3]. It is known that exercise plays an important and relevant role in vascular adaptations.
One way to measure vascular adaptations is through the intima media thickness (IMT), another is through flow-mediated dilation (FMD) with cuff inflation and deflation. In the case of able-bodied people with increased cardiovascular risk or disease demonstrating a priori impaired FMD, exercise training leads to improvement in FMD. In healthy able-bodied people, a temporary increase in FMD with normalization is expected after a period of training. Existing research recognizes the critical role played by exercise in able-bodied people in activated and nonactivated regions [4, 5]. Exercise three times a week of 30 min of cycling for 8 weeks resulted in a decrease of wall thickness and wall-to-lumen ratio in the superficial femoral artery and the carotid artery [6]. A study focusing on training for the marathon (four times a week for a period of 16 weeks) showed a decrease in brachial and popliteal total wall thickness and an increase in lumen diameters [7]. A 6-month training program consisting of either full-body resistance training or endurance training showed a decrease in carotid artery intima media thickness (IMT) [8].
In people with SCI, hybrid cycling, which includes cycling with the legs via electrical stimulation (ES) combined with voluntary handcycling, is the approach with the most potential for improving the endothelial function in the activated limbs of people with a SCI [9]. In people with SCI, despite the increased cardiovascular risk, FMD is higher than in healthy people but FMD decreases in the stimulated areas following a period of exercise training [10,11,12]. Previous studies in people with SCI [13,14,15,16] have only shown local vascular adaptations after a period of ES exercise, but not in the nonstimulated areas. Thijssen et al. [14] found that local vascular adaptations (diameter) occurred in the ES- stimulated areas, but not in the nonstimulated areas (calf and forearm) (diameter and FMD), in individuals with a SCI after 4 weeks of hybrid cycling (three times a week for 30 min). Measurements on the forearm, however, were biased by the fact that the arms were highly developed as a result of regular wheelchair exercise. In addition to that, this study was limited to a period of 4 weeks of hybrid cycling, which was probably not sufficient for vascular adaptations in the nonstimulated areas. It has previously been observed that the systemic effects of hybrid cycling result in increased cardiorespiratory fitness in people with a SCI . It was also demonstrated that hybrid cycling resulted in a higher metabolic rate and cardiorespiratory response than handcycling [17].
It is established that exercise in people with a SCI induces vascular adaptation in the stimulated area. The influence of exercise on the nonstimulated areas, however, remains unclear. To date, no study has investigated the effect of exercise for periods longer than 4 weeks on the nonstimulated areas in persons with a SCI.
The aim of this pilot study was to explore whether vascular adaptations occur in the nonactivated areas after a relatively long training period either with hybrid cycling or handcycling. The IMT and diameter at the common coronary artery (CCA) and superficial femoral artery (SFA) were used to measure nonstimulated areas. FMD at the brachial artery (BA) was a measure for nonstimulated areas in de hybrid group with the consideration of local muscle activity during hand and hybrid cycling. It was expected that training would reduce the intima media thickness (IMT) in the CCA and SFA. It was also expected that the difference in mainly the CCA and SFA would be larger with hybrid cycling compared to handcycling, due to the larger muscle mass involved.
Methods
This study is part of a larger study, which was described by Bakkum et al. [18] in 2013. Briefly, a 16-week Randomized Controlled Trial was performed in two Dutch rehabilitation centers (Amsterdam and Nijmegen) between November 2011 and November 2013. Participants were randomly assigned to either the experimental group (hybrid cycle training group) or the control group (handcycle training group). Participants in Nijmegen also provided vascular measurements as part of the present study in order to study vascular adaptations in nonstimulated areas during hybrid cycling as opposed to handcycling.
Participants
Ten men with a long-standing SCI of at least 8 years, aged between 28 and 65, wheelchair dependent and inactive (lower than the 75th percentile in the Physical Activities Scale for Individuals with Physical Disabilities (PASIPD) [19] of a Dutch cohort study population) were recruited from the database of the rehabilitation center in Nijmegen. Each received an information letter and signed an informed consent indicating voluntary participation in the study. The study was completed in accordance with the Medical Ethics Committee of the VU University Medical Centre Amsterdam. After screening by a rehabilitation physiatrist, patients with pressure sores, cardiovascular problems, severe musculoskeletal complaints, or psychiatric problems were excluded.
The handcycle
The handcycle (Speedy-Bike, Reha-Technik GmbH, Delbrück, Germany) was equipped with a wide synchronous bull-horn crank, and with 8 gears that can be changed manually. The handcycle was placed on a Tacx Flow ergotrainer (Tacx Flow, Technische Industrie, Tacx B.V., Wassenaar, The Netherlands).
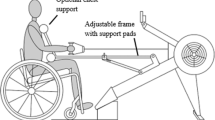
The hybrid cycle
The BerkelBike Pro (Berkelbike BV, Sint-Michielsgestel, the Netherlands) with a similar handbike and also placed on the Tacx Flow ergotrainer was used for hybrid cycling, combining synchronous handcycling with asynchronous ES-induced leg cycling. A six-channel stimulator (NeuroPro, Berkelbike) provided ES via self-adhesive 50 × 90 mm surface electrodes placed bilaterally over the quadriceps, hamstrings, and gluteal muscles. The pulse duration was 400 µs and the maximum current amplitude was 150 mA.
Training protocol
One week before the first training session, participants carried out a graded peak exercise test in their own handrim-propelled wheelchair and had their maximal exercise response measured. Participants performed 32 training sessions within a continuous period of 16 weeks. Each training session started with a warm-up, followed by a training session of between 18 and 32 min (rate of perceived exertion of 4–7 on the Borg’s 10-point scale and 65–75% heart rate reserve response during training). For the detailed training program see Bakkum et al. [18].
Outcome measurement
The primary outcomes were intima media thickness (IMT) at the carotid artery and FMD at the brachial artery. Secondary outcomes were IMT and FMD at the femoral artery.
At baseline (pre-test), we collected patient characteristics: age, gender, lesion level and completeness with the AIS scale, medical history, intoxication history, spasticity, body mass, height, body mass index (BMI), and PASIPD score (Physical Activities Scale for Individuals with Physical Disabilities) [19]. The IMT and diameter were measured at CCA, BA and SFA and FMD at BA was measured. During the training, we collected training time, stimulation (amplitude) of the ES, Borg scale and if there was any discomfort or pain. After the training program (post-test) IMT, diameter and FMD were measured again as soon as possible.
Intima media thickness (IMT) and diameter were measured under standardized conditions using high-resolution ultrasound (T3000, Terason, Burlington, MA) across arteries in the neck (common carotid artery) and leg (superficial femoral artery). With the AVI converter, the files were converted to Dicom files. Those files were analyzed in IMT software version 3.0. The program visualized the upper and lower lumen intima and the media adventitia (Fig. 1). Frames that were taken when the ultrasound was moved, frames where no media adventitia was found, and part of the frames where no media adventitia was found or placed wrong, were excluded. Then the program made a calculation of the mean, minimum, maximum, and standard deviation of the IMT and Diameter. The analysis was done by a different person than who performed the ultrasound measurement and was blinded for the training group. To gain experience with the computer program all ten analyses were done once without adding those results into the study result. When all measurements were done a second time, the analyses were viewed together with an expert and after receiving advice the analyses were done a third time. Those results were used in the study results.
Flow-mediated dilatation and nitroglycerine-mediated dilatation were measured under standardized conditions using high-resolution ultrasound across arteries in the arm (brachial artery) and leg (superficial femoral artery). The video was analyzed in Dicom encoder and FMD/blood flow analysis program version 3.0. The region of interest in the Doppler signal and in the artery was selected. The video was played while the artery and Doppler signal were visualized. The program transfers this into graphs; one with time on the x axis and diameter on the y axis, one with peak blow flow on the x axis and one with shear rate on the y axis. The peak blood flow graph is to inform when the constriction and dilatation took place. Irregularities of the signal were selected and the video of that part was shown again. If at that moment the ultrasound was moved, those areas were excluded. In FMD settings, the baseline area and dilatation area were selected and subsequently the program calculated baseline diameter, FMD peak diameter, FMD peak diameter percentage. The same was done with glyceryl trinitrate (GTN)-mediated dilatation with GTN settings, where baseline, GTN peak, GTN peak percentage were measured. Again to gain experience, all measurements were done three times and viewed with an expert, where only the third results were used for further analysis.
Statistical analysis
Statistical analysis was performed using the SPSS statistical software package version 23. The repeated measures ANOVA analysis was used and effect size (Cohen’s d) to examine the effect of 16 weeks of exercise either with hybrid cycling or handcycling on IMT and FMD of the different arteries. The handcycle and hybrid cycle training groups were equally analyzed. For Cohen’s d 0.2 is a small effect, 0.5 medium and 0.8 large [20]. To analyze the individual effects, graphs were made with the pre-test outcomes of IMT, diameter and FMD plotted against the post-test outcomes.
Results
Participants
Characteristics of the participants are shown in Table 1. Participants 5, 9, and 10 were smokers, and participants 3, 4, and 5 had mild spasticity. All ten participants finished the study but participant 8 missed one training session, participant 7 missed two sessions and participant 10 missed five sessions due to holidays. With participant 1 some measurements were incorrect. Participant 6 was too hypotensive post-test to complete the measurements. Half the participants (participants 3, 6, 7, 8, and 10) were measured more than one week after the last training session.
Vascular adaptations
In the whole test group (hybrid and/or handcycle), 32 handcycle or hybrid cycle training sessions did not result in significant changes in IMT in the CCA and in the SFA. No changes in diameter and FMD of the BA (Table 2 and Fig. 2) were found. When viewing the plots in which the individual pre- and post-test outcomes are visualized, group differences are not clearly shown and contradictory results between the individual participants appeared.
Discussion
The study showed that 16 weeks (twice a week for 18–30 min) of hybrid cycling or handcycling did not result in vascular changes at nonstimulated areas. Our hypothesis was that after hybrid cycling or handcycling IMT at the nonstimulated areas would get smaller but neither on a group level nor on an individual level were vascular changes found.
Pre-test results showed that the diameters of SFA and CCA were comparable to those previously reported [11], but the pre-test FMD was slightly higher [10, 21]. People with SCI use their arms more intensively than able-bodied people, which might show a local trained effect of the arm. Pre-test results of the three participants who smoke, were the same as the rest of the group, even though it is known that there is an inverse relationship between the intensity of tobacco smoke and FMD [2]. Pre-test results of the 3 participants with mild spasticity were the same as the rest of the group even though spasticity can simulate a small exercise effect. Two people with a cervical lesion (participants 3 and 5) were included, which could have influenced their FMD in the brachial artery with a larger pre-test FMD (due to atrophy of the arm muscles). They did, however, not show different values in their pre-test FMD (perhaps because one had a motor incomplete lesion and both had spasticity).
The 16 weeks, twice a week, up to 30 min, hybrid or handcycle training program did not result in any vascular adaptations of nonstimulated areas in people with a SCI. All except one participant finished their exercise schedule. Results contrast with several training studies (including able-bodied people) in which the training frequency was at least three times a week resulting in vascular changes in non-trained areas [8, 22]. Thijssen et al. [14] did not measure any change in vascular adaptation in the brachial artery in patients with SCI after 4 weeks of twice-weekly hybrid cycling for 25 min. Four weeks of hybrid cycling, and 16 weeks of twice a week 30 min training might, therefore, not have been long and/or frequent enough for vascular adaptation. To train for a 3-month period 3×/week for 60 min will be a challenge for this group. If people with a SCI want to achieve the benefits, lifelong training will probably be necessary to reduce their increased risk of cardiovascular diseases. It is a challenge to arrange frequent long-term training in a rehabilitation center with enough motivated sedentary participants. Training at home with a handcycle and Compex electrical stimulation might be an acceptable alternative.
The training intensity in our study was between 4 and 7 on the Borg’s 10-point perceived exertion scale and/or 65–75% heart rate reserve response during training. In our study, the time and intensity were gradually increased, while all the studies with able-bodied participants immediately started with training at least three times a week. People with a SCI need to gradually increase the intensity to adapt to hybrid cycling. It is known that exercise intensity is an important factor in remodeling endothelial function in healthy, obese, and heart failure patients [23,24,25,26,27,28]. Training at a higher intensity might have been more effective in people with SCI. To achieve a higher intensity, one may increase the resistance with handcycling. However, starting at a high intensity is prone to overuse injuries. Especially in the case of spinal cord injured people, who are limited in which muscles they can use. Adding more resistance might make the exercise more prone to overuse injuries in the arms, which can be a significant handicap for wheelchair users with SCI [29]. The balance between exercise with high intensity and low risk of overuse is important. It might be necessary to separate the adapting period from the intervention period and to start the actual intervention after the adapting period, resulting in a longer period of exercise with high intensity.
The limitations of our study include the small sample size and the heterogeneity within the sample. We were aware that it would be difficult to get significant results with such a small sample size in this pilot study, but we hoped to see a trend, which could be explored in a future study. Our recommendation for a future study would be more frequent training (>3 times a week) with a higher intensity in a home-based setting with an adaptation period prior to training.
Conclusion
Sixteen weeks of hybrid cycling or handcycling did not result in vascular adaptation in nonstimulated areas (such as brachial, coronary artery, and femoral superficialis artery). We cannot conclude that this does not happen either with a more intense and frequent training protocol with a larger sample size. This pilot study had its limitations, particularly the small sample size. To analyze if hybrid cycling or handcycling has an effect on the nonstimulated areas, a study design with more frequent training and higher intensity is needed, which might involve home-based training and an adaption period prior to training.
Data archiving
The datasets generated during and/or analyzed during the current study are not publicly available due to the fact that the study is part of a bigger study but are available from the corresponding author on reasonable request.
References
Cragg JJ, Noonan VK, Krassioukov A. Cardiovascular disease and spinal cord injury results from a national population health survey. Neurology. 2013;81:723–8.
Hadi HA, Carr CS, Al Suwaidi J. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vascular Health Risk Manage. 2005;1:183–98.
Widmer RJ, Lerman A. Review article Endothelial dysfunction and cardiovascular disease. Global Cardiol Sci. Practice 2014;2014:43.
Rowley NJ, Dawson EA, Hopman MTE, George KP, Whyte GP, Thijssen DHJ, et al. Conduit diameter and wall remodeling in elite athletes and spinal cord injury. Med Sci. Sports Exerc. 2012;44:844–9.
Mora S, Cook N, Buring JE. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007;116:2110–18.
Thijssen DHJ, Dawson EA, van den Munckhof ICL, Birk GK, Timothy Cable N, Green DJ. Local and systemic effects of leg cycling training on arterial wall thickness in healthy humans. Atherosclerosis. 2013;229:282–6.
Hafner NM, Womack CJ, Luden ND, Todd MK. Arterial adaptations to training among first time marathoners. Cardiovasc Ultrasound.2015;14:1–9.
Spence AL, Carter HH, Naylor LH, Green DJ. A prospective randomized longitudinal study involving 6 months of endurance or resistance exercise. Conduit artery adaptation in humans. J Physiol. 2013;591:1265–75.
Phillips AA, Cote AT, Warburton DER. A systematic review of exercise as a therapeutic intervention to improve arterial function in persons living with spinal cord injury. Spinal Cord. 2011;49:702–14.
de Groot PCE, Poelkens F, Kooijman M, Hopman MTE. Preserved flow-mediated dilation in the inactive legs of spinal cord-injured individuals. Am J Physiol Heart Circ Physiol. 2004;287:H374–80.
de Groot PC, Bleeker MW, van Kuppevelt DH, van der Woude LH, Hopman MT. Rapid and extensive arterial adaptations after spinal cord injury. Arch Phys Med Rehabil. 2006;87:688–96.
Raitakari OT, Celermajer DS. Flow-mediated dilatation. Br J Clin Pharm. 2000;50:397–404.
Gerrits HL, de Haan A, Sargeant AJ, van Langen H, Hopman MT. Peripheral vascular changes after electrically stimulated cycle training in people with spinal cord injury. Arch Phys Med Rehabil. 2001;82:832–9.
Thijssen DHJ, Heesterbeek P, Van Kuppervelt DJM. Local vascular adaptations after hybrid training in spinal cord-injured subjects. Med Sci Sports Exerc. 2005;37:1112–8.
De Groot P, Crozier J, Rakobowchuk M, Hopman M, Macdonald M. Electrical stimulation alters FMD and arterial compliance in extremely inactive legs. Med Sci Sports Exerc. 2005;37:1356–64.
Thijssen DH, Ellenkamp R, Smits P, Hopman MT. Rapid vascular adaptations to training and detraining in persons with spinal cord injury. Arch Phys Med Rehabil. 2006;87:474–81.
Bakkum AJT, De Groot S, Onderwater MQ, De Jong J, Janssen TWJ. Metabolic rate and cardiorespiratory response during hybrid cycling versus handcycling at equal subjective exercise intensity levels in people with spinal cord injury. J Spinal Cord Med. 2014;37:758–64.
Bakkum AJT, De Groot S, Van Der Woude LHV, Janssen TWJ. The effects of hybrid cycle training in inactive people with long-term spinal cord injury: design of a multicenter randomized controlled trial. Disabil Rehabil. 2013;35:1127–32.
Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83:193–200.
Nakagawa S, Cuthill IC. Effect size, confidence interval and statistical significance: a practical guide for biologists. Biol Rev. 2007;82:591–605.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart 2013;99:1837–42.
Tanaka H, Seals DR, Monahan KD, Clevenger CM, Souza CADE, Dinenno FA, et al. Regular aerobic exercise and the age-related increase in carotid artery intima-media thickness in healthy men. J Appl Physiol. 2020;2020:1458–64.
Ashor AW, Lara J, Siervo M, Oggioni CCC. Exercise modalities and endothelial function: a systematic review and dose- response meta-analysis of randomized controlled trials. Sports Med. 2015;45:279–96.
Slordahl SA, Lee SJ, Videm V, Bye A. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart. Circulation. 2007;115:3086–94.
Schjerve IE, Tyldum GA, Tjonna AE, Stolen T, Loennechen JP, Hansen HEM. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin Sci. 2008;293:283–93.
Covassin T, Cheng G, Nayar S, Heiden E. Epidemiology of overuse and acute injuries among competitive collegiate athletes. J Athletic Training. 2012;47:198–204.
Ristolainen L, Heinonen A, Turunen H, Mannstr”m H, Waller B, Kettunen JA. Type of sport is related to injury profile: a study on cross country skiers, swimmers, long-distance runners and soccer players. A retrospective 12-month study. Scandinavian J Med Sci Sports. 2010;20:384–93.
Ch‚ron C, Scanff C, Le, Leboeuf-yde C. Association between sports type and overuse injuries of extremities in adults: a systematic review. Chiropr Man Therap. 2016;24:1–10.
Fagher K, Lexell J Sports-related injuries in athletes with disabilities. 2014;24:320–31.
Funding
No financial assistance was received in support of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jansen, E., de Groot, S., Smit, C.A. et al. Vascular adaptations in nonstimulated areas during hybrid cycling or handcycling in people with a spinal cord injury: a pilot study of 10 cases. Spinal Cord Ser Cases 7, 54 (2021). https://doi.org/10.1038/s41394-021-00417-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00417-2