Abstract
Introduction
There have been 30 clinically suspected cases and 41 histopathologically confirmed cases of fibrocartilaginous embolism (FCE) reported in the literature. FCE often has a poor prognosis and is estimated to represent 5.5% of spinal cord infarctions, but may be more common than initially presumed given underdiagnosis due to its vague clinical presentation.
Case presentation
We report two cases, a 15-year-old male and a 15-year-old female, whose clinical history, examination, and imaging findings were consistent with spinal cord infarction secondary to FCE.
Discussion
These cases were unique given our patients’ neurologic improvement; however, the commonly held assumption of poor prognosis may in part be fueled by the preferential case ascertainment via biopsy on autopsy. These cases highlight the importance of recognizing rare causes of spinal cord pathology and considering FCE in the differential diagnosis of acute myelopathy.
Similar content being viewed by others
Introduction
Spinal cord infarction is rare in the pediatric population [1,2,3]. The pathogenesis differs from adults in whom spinal cord infarcts are most commonly reported in the context of aortic surgery, whereas in children the etiology is often unknown [4,5,6]. Fibrocartilaginous embolism (FCE) refers to the migration of fibrocartilaginous nucleus pulposus material through the nearby vasculature to embolize into one of the spinal cord vessels [7, 8]. The intervertebral disc is largely avascular, but can be the source of embolic material as evidenced by histopathologic sectioning and staining in case reports of FCE [6,7,8,9].
FCE is a rare cause of spinal cord infarction, first reported in 1961 in a 15-year-old boy who developed tetraplegia shortly after suffering a trivial fall on his back [8, 10]. There have been 30 clinically suspected cases and 41 histopathologically confirmed cases of FCE [6, 9, 11]. FCE often has a poor prognosis and is estimated to represent 5.5% of spinal cord infarctions, but may be more common than initially presumed if underdiagnosed due to its vague clinical presentation [8, 12, 13]. It is theorized that the initial trigger for disruption of the fibrocartilaginous nucleus pulposus material is increased intra-vertebral body pressure by axial loading forces applied to the spine, such as falls, straining, or lifting [14, 15]. We report two cases, a 15-year-old male and a 15-year-old female, whose clinical history, examination, and imaging findings were consistent with spinal cord infarction secondary to FCE.
Case 1 presentation
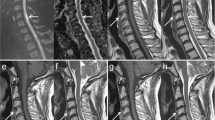
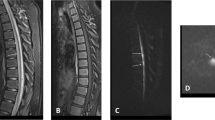
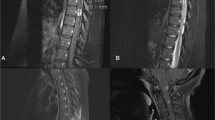
A 15-year-old male with no significant past medical history presented with acute onset tetraplegia after lifting 30 lbs in a seated overhead press. He suddenly felt a pop and pain in his neck and back followed by numbness and tingling in his upper limbs with progressive weakness. Within 15 min of symptom onset, he was unable to walk and only had trace movement in bilateral grip strength. Workup in the acute hospital revealed C5–C7 anterior cervical cord infarct on MRI and associated Schmorl’s nodes (Fig. 1). Differential diagnosis included arterial dissection, cardioembolic disease, hypercoagulable state, vasculitis, and drug induced infarction. The patient had not undergone any recent procedures or surgeries and was not on anticoagulation. CTA of the head and neck did not reveal aneurysms, dissections, or significant stenosis. Echocardiogram did not show any valvular disease, patent foramen ovale, or atrial abnormality. EKG and telemetry did not reveal any cardiac arrhythmia. Hypercoagulable workup, urine tox screen, and vasculitis workup were negative. Given the patient’s temporal correlation with an axial loading activity, characteristic imaging findings of anterior spinal cord infarction with associated Schmorl’s nodes, and workup negative for alternative causes, the patient was presumed to have spinal cord infarction secondary to FCE. The patient was placed on low-dose aspirin as well as medication for his neuropathic pain. On admission to inpatient rehab, his diagnosis was C5 AIS D tetraplegia with associated neuropathic pain as well as neurogenic bowel and bladder. He required moderate assistance with his ADLs, minimal assistance with level transfers, and minimal assistance with gait. During his hospitalization, he was managed with an indwelling catheter and then intermittent catheter program, bowel program with suppository, and medication for neuropathic pain. Upon discharge from inpatient rehab, his strength had improved, but he was still weak in his upper extremities. He was voiding and defecating independently and had regained the ability to ambulate independently in the community.
Case 2 presentation
A 15-year-old female with mild scoliosis developed sudden onset numbness and weakness of her upper extremities after recreational golfing. Initially, her arms began hurting after swinging a golf club and then after arriving home her arms and fingers began to weaken. She presented to urgent care 4 h later and then to the emergency department due to progressive leg numbness and weakness. Initial impression was functional neurologic symptom disorder; however, MRI showed an acute spinal cord infarction concerning for fibrocartilaginous embolus to the anterior spinal artery given the proximity of the degenerate intervertebral disc space at C6–7 to the anterior spinal cord infarct extending from C4 down to C7. Differential diagnosis included arterial dissection and cardioembolic disease. Complete neurologic workup including CTA head and neck, MRA head and neck, EKG, and telemetry were without acute abnormalities. The patient had not had any surgeries or procedures predisposing her to hypoperfusion. Given the temporal correlation with an axial loading activity, characteristic imaging, and workup negative for alternative causes, the etiology of the patient’s spinal cord infarction was thought to be secondary to FCE. The patient initially experienced shortness of breath and urinary retention and required transfer to the ICU where she received steroids and required norepinephrine to aid with spinal cord perfusion. Angiogram and lumbar puncture were negative, so the patient was also started on heparin. On admission to inpatient rehabilitation, she was found to have a C4 AIS D SCI with associated orthostatic hypotension and neurogenic bladder and bowel. She required significant assistance with most of her ADLs, moderate assistance with level transfers, and total assistance of gait. During her hospitalization, she was managed with an intermittent catheter program as well as a bowel program with suppository. Her orthostatic hypotension was managed with midodrine, hydration, compression hose, and abdominal binder. At discharge 3 weeks later she was able to ambulate without an assistive device and required only supervision from a therapist or family member to maintain safety. At 5-month follow-up patient strength was improved, but she was still weak most notably in her hands. She still had urinary incontinence requiring medications, but had regained control of her bowels only requiring oral medications, returned successfully to school, returned to community ambulation without an assistive device, was referred to driving rehabilitation, and was restarting her martial arts practice.
Discussion
Classical clinical presentation of FCE is onset of dull transient neck or back pain followed by a syndrome of myelopathy that bears temporal correlation to a minor incident [8, 16]. Examination typically reveals a sensory level and bowel/bladder dysfunction in conjunction with paraplegia or tetraplegia [8, 16]. Imaging classically reveals Schmorl’s nodes and anterior spinal cord infarction [17,18,19,20]. Thus, these patients’ clinical presentations, examinations, and imaging findings were characteristic of FCE. Furthermore, FCE typically exhibits a rapid course of symptoms with time from trigger to symptom onset in the course of minutes to hours as was seen in our patients [7, 8]. FCE also usually presents with numbness that progresses to weakness as was seen in our patients [8, 21]. Interestingly, both patients exhibited persisting upper extremity weakness, which has also been seen in prior cases noted in the literature [8].
Forty-one pathologically proven cases of spinal cord infarction secondary to FCE have been reported in the literature, including 15 men and 26 women ranging from 14 to 78 years in age with half the patients under 40 years of age [8]. Sixty-one percent of cases presented following an incident that triggered increased intra-disc or intra-vertebral body pressure with the duration between this trigger event and the onset of symptoms varying from minutes to days, but averaging 2.4 days [8]. There was associated neck or back pain in 76% of cases with asymmetric weakness in 15% of cases [8]. Forty out of the 41 patients died leading to autopsy allowing for histopathologic confirmation of FCE, and nearly 40% of deaths were due to preventable respiratory complications (pulmonary embolism 20%, pneumonia 17%, aspiration 2%) [8]. In one case, a laminectomy was performed in a living patient and histologic examination of necrotic tissue revealed staining characteristic of degenerative fibrocartilage [8, 16].
There have been 30 clinically suspected cases of FCE including the cases presented here. The majority of cases evidenced significant ongoing neurologic deficits [8, 16]. However, two clinically suspected cases of FCE in previously healthy 16-year-old and 17-year-old males showed similar neurologic improvement [7]. Both individuals experienced acute myelopathy with spinal cord imaging significant for infarction after performing lifting exercises in squat positions. Workup for other etiologies of spinal cord infarction was negative [7]. Neither patient received steroids nor blood pressure support and both received early acute intervention and rehabilitation [7].
The cases presented here were relatively unique given our patients’ neurologic improvement; however, the commonly held assumption of poor prognosis may in part be fueled by the preferential case ascertainment via biopsy on autopsy. Diagnosis is typically clinical since confirmation requires biopsy for histopathologic analysis that has almost exclusively been obtained in fatal cases [16]. Given the vague clinical presentation and difficulty with histopathologic confirmation, many cases have initially been misdiagnosed as functional neurologic disorder or transverse myelitis [8]. Thus, a disproportionate number of FCE cases may be characterized as severe given that many of the less severe cases may have been misdiagnosed.
In addition, early acute intervention and rehabilitation intervention may have contributed to our patients’ neurologic recovery. Both patients initially presented to a pediatric level 1 hospital staffed by neurology that led to their timely identification and treatment. In the case of our 15-year-old female, steroids and timely blood pressure management may have contributed to her recovery, although our 15-year-old male did not require steroid and blood pressure management. Little research has been conducted on specific treatment options for FCE; however, previous research has shown treatments such as steroids, intravenous immunoglobulin, plasma exchange, and heparin to be ineffective [8]. No research has been performed to study the effect of blood pressure management on recovery in FCE. Both patients likely benefited from targeted rehabilitation with a short time frame from injury to admission to rehabilitation.
Ultimately, these cases highlight the importance of recognizing rare causes of spinal cord pathology and considering FCE in the differential diagnosis of acute myelopathy. More research is needed to identify early interventions for spinal cord infarction caused by FCE and it is important that patients with presumed FCE be enrolled into early targeted rehabilitation.
References
de Seze J. Acute myelopathies: clinical, laboratory and outcome profiles in 79 cases. Brain. 2001;124:1509–21. https://doi.org/10.1093/brain/124.8.1509.
Shah S, Bryant P. Fibrocartilaginous emboli in the pediatric population: the role of rehabilitation in facilitating functional recovery. J Pediatr Rehabil Med. 2018;11:53–6. https://doi.org/10.3233/PRM-170502.
Nance JR, Golomb MR. Ischemic spinal cord infarction in children without vertebral fracture. Pediatr Neurol. 2007;36:209–16. https://doi.org/10.1016/j.pediatrneurol.2007.01.006.
Romi F, Naess H. Spinal cord infarction in clinical neurology: a review of characteristics and long-term prognosis in comparison to cerebral infarction. Eur Neurol. 2016;76:95–8. https://doi.org/10.1159/000446700.
Robertson CE, Brown RD, Wijdicks EFM, Rabinstein AA. Recovery after spinal cord infarcts: long-term outcome in 115 patients. Neurology. 2012;78:114–21. https://doi.org/10.1212/WNL.0b013e31823efc93.
Cheshire WP, Santos CC, Massey EW, Howard JF. Spinal cord infarction: etiology and outcome. Neurology. 1996;47:321–30. https://doi.org/10.1212/WNL.47.2.321.
Han JJ, Massagli TL, Jaffe KM. Fibrocartilaginous embolism—an uncommon cause of spinal cord infarction: a case report and review of the literature. Arch Phys Med Rehabil. 2004;85:153–7. https://doi.org/10.1016/S0003-9993(03)00289-2.
AbdelRazek MA, Mowla A, Farooq S, Silvestri N, Sawyer R, Wolfe G. Fibrocartilaginous embolism: a comprehensive review of an under-studied cause of spinal cord infarction and proposed diagnostic criteria. J Spinal Cord Med. 2016;39:146–54. https://doi.org/10.1080/10790268.2015.1116726.
Bansal S, Brown W, Dayal A, Carpenter JL. Posterior spinal cord infarction due to fibrocartilaginous embolization in a 16-year-old athlete. Pediatrics. 2014;134:e289–92. https://doi.org/10.1542/peds.2013-2468.
Reisner A, Gary MF, Chern JJ, Grattan-Smith JD. Spinal cord infarction following minor trauma in children: fibrocartilaginous embolism as a putative cause. J Neurosurg Pediatr. 2013;11:445–50. https://doi.org/10.3171/2013.1.PEDS12382.
Alkhachroum AM, Weiss D, Lerner A, De Georgia MA. Spinal cord infarct caused from suspected fibrocartilaginous embolism. Spinal Cord Ser Cases. 2017;3:17027. https://doi.org/10.1038/scsandc.2017.27.
AbdelRazek M, Elsadek R, Elsadek L. Case series of two patients with fibrocartilaginous embolism mimicking transverse myelitis of the spinal cord. J Clin Neurosci. 2017;40:66–8. https://doi.org/10.1016/j.jocn.2017.02.003.
Nagata K, Tanaka Y, Kanai H, Oshima Y. Acute complete paraplegia of 8-year-old girl caused by spinal cord infarction following minor trauma complicated with longitudinal signal change of spinal cord. Eur Spine J. 2017;26:1432–5. https://doi.org/10.1007/s00586-017-4995-9.
Suetsuna F. Spinal cord injury due to cervical disc herniation caused by bench pressing. J Spine. 2013;3. https://doi.org/10.4172/2165-7939.1000154.
Millichap JJ, Sy BT, Leacock RO. Spinal cord infarction with multiple etiologic factors. J Gen Intern Med. 2007;22:151–4. https://doi.org/10.1007/s11606-006-0029-8.
Mateen FJ, Monrad PA, Leep Hunderfund AN, Robertson CE, Sorenson EJ. Clinically suspected fibrocartilaginous embolism: clinical characteristics, treatments, and outcomes: fibrocartilaginous embolism: a case series. Eur J Neurol. 2011;18:218–25. https://doi.org/10.1111/j.1468-1331.2010.03200.x.
Samartzis D, Karppinen J, Mok F, Fong DY, Luk KD, Cheung KM. A population-based study of juvenile disc degeneration and its association with overweight and obesity, low back pain, and diminished functional status. J Bone Joint Surg Am. 2011;93:662–70. https://doi.org/10.2106/JBJS.I.01568.
Matsumoto M, Okada E, Toyama Y, Fujiwara H, Momoshima S, Takahata T. Tandem age-related lumbar and cervical intervertebral disc changes in asymptomatic subjects. Eur Spine J. 2013;22:708–13. https://doi.org/10.1007/s00586-012-2500-z.
Cheng M-Y, Lyu R-K, Chang Y-J, et al. Concomitant spinal cord and vertebral body infarction is highly associated with aortic pathology: a clinical and magnetic resonance imaging study. J Neurol. 2009;256:1418–26. https://doi.org/10.1007/s00415-009-5126-2.
Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36:811–6. https://doi.org/10.3174/ajnr.A4173.
Mikulis D, Ogilvy C, McKee A, Davis K, Ojeman R. Spinal cord infarction and fibrocartilagenous emboli. Am J Neuroradiol. 1992;13.
Acknowledgements
We would like to acknowledge the patients, families, and staff of TIRR Memorial Hermann Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Draganich, C., Wenzel, L.R. Fibrocartilagenous embolism case series: is it a zebra?. Spinal Cord Ser Cases 7, 28 (2021). https://doi.org/10.1038/s41394-021-00395-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00395-5