Abstract
Study design
Online survey distributed to healthcare professionals (HCPs) involved in care of spinal cord injury (SCI) patients with neurogenic lower urinary tract dysfunction (NLUTD).
Objectives
Identify and bring awareness to the variation of neurogenic bladder management in around the world.
Setting
International online questionnaire.
Methods
A 32-question survey was drafted and circulated among a global network of SCI experts for review. The survey was disseminated to healthcare professionals involved in the care of NLUTD in SCI patients via social media, grassroots methods, and international societies. The survey was available for 6 weeks and respondents answered questions regarding SCI population demographics, access to care, common neurogenic bladder management, diagnostic and imaging methods, complications, and follow up.
Results
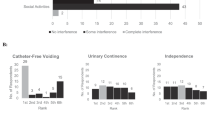
A total of 296 healthcare professionals, 132 from North America, 87 from Europe, 27 from Asia, 24 from Australia, 14 from South America, and 6 from Africa, responded to the survey. Global concurrence was noted among management method for patients without adequate hand function, first-line treatment for neurogenic detrusor overactivity, and common complications. Continents highly differed in responses regarding management method for patients with adequate hand function, frequency of patients reusing catheters, timing of urodynamics, and duration of antibiotic therapy for urinary tract infections.
Conclusions
The results of this international survey demonstrate the variability and uniqueness in neurogenic bladder management in SCI patients around the world. Increased international discourse and education will improve global communication and transparency with the efforts of reducing discrepancies in care.
Similar content being viewed by others
Introduction
Neurogenic bladder (NGB), the presence of lower urinary tract dysfunction as a result of central or peripheral nervous system damage, is common with many neurologic diseases and notably in patients with spinal cord injury (SCI) [1]. The prevalence of traumatic SCI across various continents has been summarized through various literature reviews, however, data for major populations is still missing. Regions of Asia estimate 236–464 per million, while Australia and Western Europe report 370–681 and 240–365 cases of SCI per million respectively [2,3,4,5,6,7,8,9,10,11]. The majority of published data regarding North American SCI prevalence is from the United States with a broad range of 473–4187 per million [2, 12, 13]. No current published data was found for prevalence in both Africa and South America, however, extrapolated data estimates incidence rates to be 21–29 and 19–25 per million respectively [2]. While the prevalence of neurogenic bladder for the general population is unknown, it is estimated that 70–84% of SCI patients are impacted by some degree of bladder dysfunction [14, 15].
Common symptoms associated with neurogenic lower urinary tract dysfunction (NLUTD) include urinary urgency, frequency, hesitancy, intermittency, incomplete bladder emptying, and incontinence, however, the type is dependent on the location and extent of the neurologic lesion [1]. Supra-pontine lesions, classified as lesions above the pontine micturition center, are associated with storage dysfunction and detrusor overactivity. In contrast, sacral and infrasacral lesions result predominantly voiding symptoms due to detrusor areflexia. Lesions in between these two areas (infra-pontine supra-sacral) produce detrusor-sphincter dyssynergia [14, 16, 17]. Furthermore, these symptoms of NLUTD can lead to embarrassment, social isolation, and ultimately cause a substantial negative impact on patient quality of life.
Evaluation of NLUTD typically includes patient history, physical examination, laboratory assessment including post void residual, and urodynamic evaluation. Collection of lower urinary tract function and initial assessment in SCI patients via data sets such as the International Spinal Cord Injury Lower Urinary Tract Function Basic Data Set allows for universal, standardized data reporting of NGB evaluation [18]. Furthermore, the International Standards to document remaining Autonomic Function after SCI (ISAFSCI) in combination with the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) are universal frameworks for reporting level and completeness of spinal lesion, as well as to assess remaining autonomic function [19, 20]. To our knowledge, there is no global reporting consensus for management of neurogenic bladder. This survey was designed to obtain information regarding variation in neurogenic bladder management around the world in order to understand global and cultural differences, with hopes that it will serve to create a foundation upon which to build universal guidelines for NGB care.
Methods
A 32-question survey was initially drafted by the authors and circulated among a network of 32 SCI experts across 5 continents for review and comments. Following edits, a consensus was achieved and the finalized survey was distributed to healthcare professionals (HCPs) involved in the care of NLUTD in SCI patients via social media, grassroots methods, and regional, national, and international spinal cord societies including the International Spinal Cord Society, the Society of Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction, the Academy of Spinal Cord Injury Professionals, and the non-profit group Sustain Our Abilities. The survey was available online through SurveyMonkey® for 6 weeks for participants to complete.
Survey questions were divided into the following subsections. The initial five introductory questions focused on demographics of survey participants, including the type of economy and healthcare system, continent and country, and primary profession of respondents. Two questions determined the ease of access to specialized care of neurogenic bladder dysfunction in both the acute care and outpatient settings. Demographics of the SCI populations treated were described by age range, frequency, and professionals involved in care. Eight survey question focused on the most common neurogenic bladder management methods used and were subdivided into acute and outpatient care, male and female patients, as well as the presence or absence of adequate hand dexterity. Four standalone questions asked about percentage of patients reusing catheters, first-line treatment of neurogenic detrusor overactivity, antibiotic duration for cystitis, and diagnosis of asymptomatic bacteriuria. Questions regarding common complications were broken down between male and female patients, as well as specific patient education on autonomic dysreflexia. The final sections consisted of manner of imaging and diagnostics in both the acute care and outpatient settings, as well as frequency of neurogenic bladder dysfunction follow-up care.
Results
Participant demographics
A total of 296 healthcare professionals responded to the survey over the course of 6 weeks. Not every survey participant responded to every question, resulting in varying sample sizes for each question. Of the respondents, 152 (54.9%) were rehabilitation physicians, 85 (30.7%) were other physician specialists including urologists, and 22 (7.9%) were nurses (Fig. 1A). Primary care physicians, mental health professionals, researchers, and therapists comprised the remaining 6.5%. The survey reached healthcare professionals over 6 continents, with 132 (45.5%) of respondents from North America, 87 (30%) from Europe, 27 (9.3%) from Asia, 24 (8.3%) from Australia, 14 (4.8%) from South America, and 6 (2.1%) from Africa (Fig. 1B). Data from certain continents, such as South America and Africa, is limited due to a smaller number of respondents, while no data was obtained from Middle Eastern regions.
Access to specialized care
HCPs were asked the ease of access to specialized care for NLUTD in both acute and outpatient settings. In the acute setting, the majority of respondents from Africa, Asia, Australia, Europe, and North America indicated care for NLUTD was easily accessible. Respondents from South America were split evenly between easily accessible and not easily accessible. In the outpatient setting, the majority of participants from Africa, Australia, Europe, as well as North and South America indicated specialized care for NLUTD to be easily accessible. In contrast, the majority of participants from Asia reported specialized care for NLUTD in the outpatient setting was not accessible.
SCI population demographics
Survey respondents were asked about patient age and frequency of patients with neurogenic bladder dysfunction. In total, 77.4% treat only adults, with 21.2% treating both pediatric and adult patients. Patients with neurogenic bladder dysfunction were seen daily by 60.4% of participants, weekly by 27.2% and monthly by 11.3%. Furthermore, participants reported which healthcare professionals at their location were involved in care of patients with neurogenic bladder. The most commonly reported answer was urologist (86.2%), followed by rehabilitation physician (74.6%), continence nurse (36.6%), general practitioner (26.8%), and family doctor (17.8%).
Management of neurogenic bladder in SCI
A large portion of the survey focused on most common forms of NGB management in SCI and results are described below and depicted in Figs. 3 and 4. Respondents chose between various catheterization methods which were defined in the survey as follows: clean intermittent catherization (ordinary hand and genital washing and use of disposable or reusable catheter); aseptic intermittent catheterization (genital antiseptic prep and single-use catheter); sterile intermittent catheterization (completely sterile setting); no- touch technique intermittent catheterization (ready-to-use, pre-lubricated catheter); indwelling catheter (Foley or suprapubic tube); or reflex voiding with use of collection device.
Acute care: hand dexterity
The majority of HCPs from Asia and Africa indicated indwelling catheter to be the most common form of bladder management for females with hand dexterity, while South American and North American participants favored clean intermittent catheterization (CIC). Australian and European HCPs were split between indwelling catheter, and CIC and no-touch IC respectively (Fig. 2A). Similarly, respondents from Africa, Asia, and Australia favored indwelling catheter as bladder management for males in acute care with hand dexterity, while North and South Americans preferred CIC (Fig. 2C).
Acute care: no hand dexterity
Healthcare professionals from all continents with the exception of South America indicated indwelling catheter to be the most common bladder management for both male and female patients in acute care without adequate hand dexterity (Fig. 2B, D). Respondents from South America were split between CIC (40%) and indwelling catheter (40%; n = 10).
Outpatient: hand dexterity
For both male and female patients with adequate hand dexterity in the outpatient setting, CIC was most commonly reported method used in Asia, Australia, and North and South America while Europe reported no-touch technique IC to be most common as seen in Fig. 3A, C. Africa was evenly divided between CIC (25%, n = 4), no-touch technique IC (25%), indwelling catheter (25%), and reflex voiding into a collection device (25%) for females. For male patients, 50% of HCPs from Africa indicated indwelling catheter to be most common (n = 4), followed by CIC (25%) and no-touch technique IC (25%).
Outpatient: no dexterity
Consistent with acute care responses, all continents but South America reported the most common bladder management for patients without adequate hand dexterity to be indwelling catheters (Fig. 3B, D). The majority of South American respondents indicated CIC to be most common (53.9%, n = 13) followed by indwelling catheter (30.8%, n = 13).
Reusable catheters in CIC patients
A follow-up question for outpatient healthcare professionals asked HCPs to indicate what percentage of their CIC patient population uses reusable catheters. This reuse practice appears to be more common in Africa, South America, and Asia with the majority of respondents indicating that 75%+ of their patients reuse catheters compared to providers in Australia, Europe, and North America who reported 0–10% of their CIC population used reusable catheters.
Neurogenic detrusor overactivity treatment
Other neurogenic bladder care questions for HCPs referred to first-line treatment of neurogenic detrusor overactivity, with the majority from all continents reporting β3 adrenergic agonist (88.3% of total respondents, n = 231), followed by beta 3 medication therapy (7.4%), and botulinum toxin therapy (1.7%).
Antibiotic therapy for symptomatic cystitis
Healthcare professionals were also asked their routine duration of antibiotic oral therapy for treating symptomatic cystitis in neurogenic bladder patients. The majority of respondents from Australia (58.8%), Europe (32.9%), North America (57.9%), and South America (83.3%) indicated 7 days as the average length of treatment. In total, 36.8% of participants from Asia responded 14 days as routine duration, while Africa was evenly split amongst 5, 7, and 10 days.
Diagnostics and imaging
Multiple survey questions asked HCPs about their routine imaging and diagnostics, as well as timing of urodynamics. The most commonly reported acute care diagnostic for NLUTD in SCI patients in all continents was renal ultrasound (62.8% total respondents), followed by blood work (58.6%) and urodynamics (43.9%). Similarly, in the outpatient setting, 89.9% of all HCPs indicated renal ultrasound was routinely performed, as well as urodynamics (78.1%) and blood work (67.9%). The timing of urodynamics varied widely among all continents for both care settings. In acute care, 23.4% of all respondents performed urodynamics 0–6 weeks post SCI, 18.6% upon development of incontinence complications, 17.7% prior to acute care discharge, and 22.9% indicated “other” timing. In the outpatient setting, 34.5% of HCPs reported performing urodynamics upon initial evaluation, 29.7% at symptom development, and 21.8% annually.
Complications
Survey respondents were asked to rank the most common complications seen as a result of poor bladder management in both male and female neurogenic bladder patients. Most HCPs ranked urinary tract infection first for both men (134 responses) and women (128 responses). Urinary incontinence followed closely behind, consistently reported as first or second most common in both men and women. Complications were not separated by continent of responded due to the weighted nature of the scoring. A known complication in patients with SCI above T6 is autonomic dysreflexia. When asked the timing of patient autonomic dysreflexia education, the majority of respondents in all continents indicated patients were informed in the acute care setting. To further patient education, the majority of respondents from Australia report distributing a card with general autonomic dysreflexia card to patients, while Asia, Europe, North America, and South America all most commonly reported not providing an autonomic dysreflexia card. Africa was split between providing a general card, a personalized card, and not providing a card at all.
Follow-up care
Outpatient respondents were asked to indicate how often they perform dedicated follow up for neurogenic bladder dysfunction in patients with neurogenic bladder function. The majority of participants from Africa (66.7%), Asia (63.2%), Australia (56.3%), Europe (64.9%), and North America (68.5%) reported following up with patients yearly. Respondents from South America mainly responded as performing dedicated follow up every 6 months.
Discussion
The result of this survey brings awareness to variations in management of NLUTD in patients with SCI across continents. For patients with adequate hand dexterity in acute care, indwelling catheter was much more common in Africa, Asia, and Australia than in North and South America, where clean intermittent catheterization was preferred. These differences continued into the outpatient setting, where CIC was highly reported in Asia, Australia, and North and South America in contrast to no-touch technique intermittent catheterization in Europe for patients with hand dexterity. One reason for the noted discrepancies amongst continents may be due to lack of awareness and adherence to current local neurogenic bladder management guidelines, as well as lack of global, unified guidelines. While some countries may not be aware of international society guidelines, others may have developed their own recommendations for management [21,22,23,24,25,26,27]. Furthermore, compliance to such guidelines may not be followed strictly or consistently [28]. Previous studies indicate routine use of CIC in developing Asian and South American countries, including China, Turkey, Pakistan, India, Malaysia, Brazil, and Mexico, which is consistent with the majority of survey respondents from these continents in the outpatient setting [21, 22, 29,30,31,32,33,34].
Survey results regarding percentage of patients reusing catheters for CIC reflected this as well, with the majority of respondents from Africa, Asia, and South America reporting >75% of patients reuse catheters in contrast to the responses from Australia, Europe, and North America where only 0–10% of patients reuse catheters. Other studies have also noted that certain countries in Africa, Asia, and South America have patients who reuse silicone catheters, with one study in Thailand reporting 3 years as the average reuse time [21, 29, 35,36,37]. Lack of access to specialized care for neurogenic bladder dysfunction, as well as lack of insurance coverage for supplies can also explain these variations in neurogenic bladder management for SCI patients. Half of survey respondents from South America indicated NLUTD care in acute care was not easily accessible, while almost 80% of respondents form Asia responded specialized NLUTD care in the outpatient setting was not easily accessible. Furthermore, the majority of respondents from Africa, Asia, and South America indicated that the economy of their country was either transitional or developing, compared to the other continents which mainly indicated their country was developed. These results could explain the higher frequency of patients reusing catheters in these locations, as well as the slightly higher reports of indwelling catheter use in these continents. Furthermore, governmental regulations and national healthcare policy, insurance coverage and access, as well as developed status of countries impact management decisions. Religious and cultural beliefs may also explain differences in bladder care around the world [28].
Conclusion
The results of this 32-questions survey distributed to healthcare professionals involved in the care of neurogenic bladder patients demonstrate the variability and uniqueness in management decisions, especially those related to catheterization methods, around the world. Increased access to care of neurogenic bladder dysfunction and increased dissemination of management guidelines may help to reduce the discrepancies noted among continents. Given various limitations in certain areas, a universal, global consensus for NLUTD management guidelines may be challenging, however, the results of the final survey question indicate that HCPs can agree that increased provider and patient education would improve the quality of care for neurogenic bladder dysfunction at their institution. One such educational event which drew attention to neurogenic bladder care variability is the recent global webinar on 7 November 2020 “What is the Best Bladder Care? A Round-The-World Discussion of Best Practices in SCI (https://www.youtube.com/watch?v=VEXLOBnbbLQ) hosted by Sustain our Abilities. We believe that increased international educational events such as this will improve transparency, communication, and provider education globally in order to reduce the discrepancies in care. The authors hope the results of this survey will increase awareness to variation in care and provide the building blocks for possible consensus and guidelines in NLUTD SCI care, similar to the frameworks of the International Data Sets and standards documents used during evaluation.
Data archiving
Survey data are available upon request to authors.
References
Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care 2013;19:s191–6.
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 2014;52:110–6.
Razdan S, Kaul RL, Motta A, Kaul S, Bhatt RK. Prevalence and pattern of major neurological disorders in rural Kashmir (India) in 1986. Neuroepidemiology 1994;13:113–9.
Weerts E. Prevention of spinal cord injury accidents. What does it mean? How can I avoid it? How can I help?. Hanoi: Vietnam; 2008.
Walsh J. Costs of spinal cord injury in Australia. Paraplegia 1988;26:380–8.
O’Connor PJ. Prevalence of spinal cord injury in Australia. Spinal Cord 2005;43:42–6.
Yeo JD, Walsh J, Rutkowski S, Soden R, Craven M, Middleton J. Mortality following spinal cord injury. Spinal Cord 1998;36:329–36.
Dahlberg A, Kotila M, Leppänen P, Kautiainen H, Alaranta H. Prevalence of spinal cord injury in Helsinki. Spinal Cord 2005;43:47–50.
Knútsdóttir S. Spinal cord injuries in Iceland 1973–1989. A follow up study. Paraplegia 1993;31:68–72.
Hagen EM, Eide GE, Rekand T, Gilhus NE, Gronning M. A 50-year follow-up of the incidence of traumatic spinal cord injuries in Western Norway. Spinal Cord 2010;48:313–8.
Levi R, Hultling C, Nash MS, Seiger A. The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995;33:308–15.
Griffin MR, O’Fallon WM, Opitz JL, Kurland LT. Mortality, survival and prevalence: traumatic spinal cord injury in Olmsted County, Minnesota, 1935–1981. J Chronic Dis 1985;38:643–53.
Cahill A, Fredine H, Zilberman L. Initial briefing: prevalence of paralysis including spinal cord injuries in the United States, 2008. Christopher and Dana Reeve Foundation, Paralysis Resource Foundation, The University of New Mexico, School of Medicine; 2009.
Dorsher PT, McIntosh PM. Neurogenic bladder. Adv. Urol. 2012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3287034/.
Manack A, Motsko SP, Haag-Molkenteller C, Dmochowski RR, Goehring EL, Nguyen-Khoa B-A, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn 2011;30:395–401.
Panicker JN, Fowler CJ, Kessler TM. Lower urinary tract dysfunction in the neurological patient: clinical assessment and management. Lancet Neurol 2015;14:720–32.
Alsulihem A, Corcos J. Evaluation, treatment, and surveillance of neurogenic detrusor overactivity in spinal cord injury patients. Neuroimmunol Neuroinflammation. 2019. https://nnjournal.net/article/view/3252.
Biering-Sørensen F, Craggs M, Kennelly M, Schick E, Wyndaele J-J. International lower urinary tract function basic spinal cord injury data set. Spinal Cord 2008;46:325–30.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2011;34:535–46.
Krassioukov A, Biering-Sorensen CF, Donovan W, Kennelly M, Kirshblum S, Krogh K, et al. International Standards to document remaining Autonomic Function after Spinal Cord Injury (ISAFSCI), First Edition 2012. Top Spinal Cord Inj Rehabil 2012;18:282–96.
Przydacz M, Denys P, Corcos J. What do we know about neurogenic bladder prevalence and management in developing countries and emerging regions of the world? Ann Phys Rehabil Med 2017;60:341–6.
Liao L. Evaluation and management of neurogenic bladder: what is new in China? Int J Mol Sci 2015;16:18580–600.
Gupta A, Taly AB, Srivastava A, Thyloth M. Urodynamic profile in myelopathies: a follow-up study. Ann Indian Acad Neurol 2009;12:35–9.
Roshanzamir F, Rouzrokh M, Mirshemirani A, Khaleghnejad A, Mohajerzadeh L, Dalirani R. Treatment outcome of neurogenic bladder dysfunction in children; a five-year experience. Iran J Pediatr 2014;24:323–6.
Çetinel B, Tarcan T, Demirkesen O, Özyurt C, Şen İ, Erdoğan S, et al. Management of lower urinary tract dysfunction in multiple sclerosis: a systematic review and Turkish consensus report. Neurourol Urodyn 2013;32:1047–57.
Theron F, Wilson V, Scriba E, et al. Best practice recommendations for bladder management in spinal cord-afflicted patients in South Africa. South African Med J. 2019;109(2b). Accessed 4 Mar 2021. http://www.samj.org.za/index.php/samj/article/view/12569.
Hussain M. Malaysian Paediatric Association (MPA): Paediatric Protocols for Malaysian Hospitals. Kementerian Kesihatan Malaysia: Malaysia; 2012.
Gomelsky A, Lemack GE, Castano Botero JC, Lee RK, Myers JB, Granitsiotis P, et al. Current and future international patterns of care of neurogenic bladder after spinal cord injury. World J Urol 2018;36:1613–9.
Singh R, Rohilla RK, Sangwan K, Siwach R, Magu NK, Sangwan SS. Bladder management methods and urological complications in spinal cord injury patients. Indian J Orthop 2011;45:141–7.
Rathore MFA, Rashid P, Butt AW, Malik AA, Gill ZA, Haig AJ. Epidemiology of spinal cord injuries in the 2005 Pakistan earthquake. Spinal Cord 2007;45:658–63.
Ersoz M, Erhan B, Akkoc Y, Zinnuroglu M, Yildiz N, Gok H, et al. An evaluation of bladder emptying methods and the effect of demographic and clinical factors on spontaneous voiding frequency in stroke patients. Neurol Sci 2013;34:729–34.
Engkasan JP, Ng CJ, Low WY. Factors influencing bladder management in male patients with spinal cord injury: a qualitative study. Spinal Cord 2014;52:157–62.
Martins G, Soler ZASG, Batigalia F, Moore KN. Clean intermittent catheterization: educational booklet directed to caregivers of children with neurogenic bladder dysfunction. J Wound Ostomy Continence Nurs 2009;36:545–9.
Landa-Juárez S, Montes de Oca-Muñoz LE, Castillo-Fernández AM, de la Cruz-Yañez H, García-Hernández C, Andraca-Dumit R. Laparoscopic vs opened appendicovesicostomy in pediatric patients. Cirugía y Cirujanos. 2014. https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=51963.
Augenstein K, Nelson VS, Kogei AJ, Hurvitz EA. Development of a bladder management protocol as part of a comprehensive care program for spina bifida in Kenya. J Pediatr Rehabil Med 2008;1:285–90.
Mazzo A, Souza-Junior VD, Jorge BM, Nassif A, Biaziolo CFB, Cassini MF, et al. Intermittent urethral catheterization—descriptive study at a Brazilian service. Appl Nurs Res 2014;27:170–4.
Kovindha A, Mai WNC, Madersbacher H. Reused silicone catheter for clean intermittent catheterization (CIC): is it safe for spinal cord-injured (SCI) men? Spinal Cord 2004;42:638–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miller, C.A., Kennelly, M.J. Pulse article: survey of neurogenic bladder management in spinal cord injury patients around the world. Spinal Cord Ser Cases 7, 16 (2021). https://doi.org/10.1038/s41394-021-00388-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00388-4
This article is cited by
-
Recently Described Innovative Reconstruction in Neurogenic Bladder: a Review
Current Bladder Dysfunction Reports (2022)