Abstract
Introduction
Sexual functioning is a high priority for people with a spinal cord injury (SCI) yet this area has received little attention. Two SCI case reports are presented which suggests there may be greater potential for the recovery of sexual functioning than previously recognised.
Case presentation
A 74-year-old SCI male (AIS D, C5/C6) and a 36-year-old SCI male (AIS A, T4/T5) were treated for neurogenic bowel using 6 weeks of abdominal FES (ABFES) (40 Hz, 300 µ pulse width (current typically 30–60 MA) simultaneously delivered (8 s contraction with 2 s ramps and 3 s off period) from both channels). The 74-year-old AIS D, C5/C6 participant reported improved strength and duration of erectile function after using ABFES for 3 weeks. The 36-year-old AIS A, T4/T5 participant reported improvements in ejaculatory function and urine flow. Both reported a reduction in time required for bowel management.
Discussion
The findings could be attributed to an improved vascularisation of the abdominal area, an improved body image and self-esteem, direct innervation of nerves involved in parasympathetic pathways or innervation of the T11/T1 area implicated in the alternative psychogenic pathway. Both participants reported they had not used ABFES during sexual activity suggesting a therapeutic effect from the treatment.
Similar content being viewed by others
Introduction
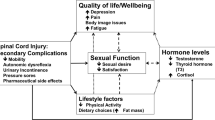
Sexual functioning is one of the highest priorities for individuals living with a spinal cord injury (SCI) [1]. Following a SCI, the majority of males report some issues with sexual functioning. While up to 95% of men will have ejaculatory problems, it has been reported that by 2 years post injury, 80% of men recover at least partial erectile function but require additional interventions due to issues with reliability and duration of function [2]. The majority of research examining treatments for sexual functioning have focused on erectile and ejaculatory dysfunction. There are a number of other issues which may influence sexual functioning including premorbid medical issues, medications, partner issues, bladder and bowel management, physical functioning due to weakness and full or partial paralysis, adjustment and self-esteem issues from body perception [2]. The current case reports focus on the use of abdominal functional electrical stimulation (ABFES) as a potential treatment for erectile and ejaculatory dysfunction. ABFES may also have positive benefits for bladder and bowel management, physical functioning, and body perception [3,4,5].
The impact of a SCI on male erection is dependent on the level and degree of injury, whether the injury is upper motor neuron (UMN) or lower motor neuron and whether the sacral reflex arc is intact or not. Erectile function can occur reflexively through sacral stimulation and a parasympathetic neurological pathway. It can also occur psychogenically under control of the hypogastric plexus originating at T11-L2 and involve the sacral segments [6]. Males who have a complete UMN injury (above T11) are able to have reflex erections but not psychogenic erections. In contrast, those with a complete lower motor neuron lesion, will often be able to have psychogenic erections but not reflex erections, dependent on preserved neurological function between T11-L2 regions. Males with an incomplete UMN lesion, should retain the capacity for reflexive erections and may retain the capacity for psychogenic erectile function, depending on the degree of preserved function in the T11-L2 area [6, 7].
A systematic review in the area for the treatment of erectile dysfunction for central nervous system diagnoses, found little high level evidence, the majority of which predominantly focused on the use of phosphodiesterase type 5 inhibitors treatment [8]. While PDE-5Is have been successfully used to treat erectile dysfunction, particularly in people with an UMN SCI; there are side effects associated with the medication including headaches, facial flushing hypotension and dizziness [9]. Treatments that are able to recover erectile dysfunction with a reduced need for medication and the associated side effects would be preferable. It would also be of value, to conduct further research into the other factors that may have an influence on sexual functioning, such as reduced vascularisation of sub-lesional tissue and muscle atrophy.
Following a SCI, there are a number of central cardiovascular adaptions as well as sub-lesional peripheral vascular adaptations that occur, such as a reduction in conduit artery diameter and blood flow. It is well established that vascular function in non-neurological populations is strongly associated with male erectile dysfunction [10]. A systematic review of treatments targeted at improving vascular function, suggests increased activity and exercise may be used to improve sexual functioning [10]. Concomitant with reduced vascularity and sedentary behaviour, there is also dramatic sub-lesional muscle atrophy observed in the first few months following a SCI [11]. These changes may have an impact on physical positioning, ability and movements for sexual activity, additionally, changes to physical appearance may lead to reduced self-esteem.
Functional electrical stimulation
Functional electrical stimulation (FES) is well established as a treatment method for improving muscle atrophy and vascularity of sub-lesional tissue [11,12,13,14,15]. ABFES could provide a potential tool to improve vascularity of the pelvic region of the trunk which may improve sexual functioning for males with SCI. ABFES is commonly used by FES physiotherapists to improve strength in weakened muscles to help with core stability. It has also been associated with improvements in aesthetic appearance of the abdominal wall for people with SCI [4]. Improved strength and aesthetic appearance of the abdominal area may contribute to improved self-esteem and physical functioning. There are also some initial small studies that have examined ABFES as a bowel management treatment for people with SCI [3, 4]. Therapeutic benefits have additionally been reported for those with neurogenic bowel and multiple sclerosis [5]. An improvement in bowel management may improve sexual functioning, through a reduction in bloating, discomfort, improved energy and quality of life and a reduction in depression and anxiety.
Spinal stimulation and sexual function
Implanted sacral route electrical stimulation has previously been used for sexual functioning in males [16]. In particular, stimulation of the S2 level produces an erection which continues as long as stimulation is applied [17]. While the technique has been found to be successful; the invasive nature of the procedure with the risk of potential complications arising post surgery; may have contributed to the reduced popularity of the procedure in recent times. The use of epidural electrical stimulation of the L1-S1 level using a 16 array implanted electrode, [18] was reported to be associated with improvements in temperature regulation, bladder function and sexual functioning in terms of sexual response and sexual performance. The researchers attribute the observed recovery, to residual supraspinal connections that existed but could not be detected clinically, being reactivated or new supraspinal connections to the spinal networks being formed [18].
Direct stimulation of the spine using implanted electrodes, is advantageous for targeting specific areas for neuromodulation, particularly for those with clinically complete SCIs. However, the invasive and permanent nature of implanted electrodes, is rejected by many people with SCIs [19], therefore, the development of effective less invasive treatments would be preferable.
ABFES and ejaculatory function case reports
In the literature there are two articles describing case reports of ABFES being used for ejaculatory function. The first case report of a 37-year-old male with a T3 complete SCI presented with the ability to obtain reflex erections easily, although these were poorly maintained without continuous stimulation [20]. The participant discovered serendipitously, that using vibratory penile stimulation (VBS) at the same time as ABFES, appeared to facilitate ejaculation. This led to an investigation of the consistency of these observations. Researchers found that using VBS alone, the subject achieved ejaculation in 4 out of 30 trials. In contrast, using VBS and ABFES together led to effectiveness in 31 out of 34 trials. A further article from the same group found similar support in two further case studies [21]. The researchers attribute the likely mechanism to direct nociception from the electrical stimulation, combined with abdominal muscle afferent input into the spinal cord reflex circuits, which increased the excitability of reflex circuits. They also postulate that intra-abdominal pressure may have contributed [20]. These initial case studies suggest ABFES should be explored further as a potential treatment for sexual functioning in males with a SCI.
Case presentations
A 74-year-old male who was injured 46 years ago with a SCI AIS D, C5/C6 was originally assessed for bowel management treatment using ABFES. The participant had been using FES for his lower limbs and gluteal muscles for 17 years to aid his walking. He had also received upper limb FES for 16 years. He was not receiving any medication for sexual functioning at the time of treatment and had reduced strength and duration of erectile function.
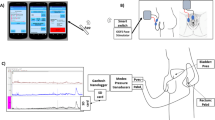
Electrical stimulation was delivered at 40 Hz, 300 µ pulse width, and 40–50 mA simultaneously (8 s contraction with 2 s ramps and 3 s off period) from both channels. A precheck confirmed autonomic dysreflexia was not elicited from the use of the electrical stimulation. The participant was instructed on electrode placement over the external oblique and transverse abdominis (Fig. 1) and the level of stimulation was set to achieve a visible contraction of the abdominal muscles. The participant was instructed to perform home administered stimulation of 2 × 30 min sessions each day for 6 weeks.
The 74-year-old participant reported an unexpected improvement, specifically in strength and duration of erectile function. He also reported an improvement in aesthetic appearance of the abdominal area and an improvement in bowel function. He attributed the improvements to using the ABFES for 3 weeks and reported that he was not using the electrical stimulation during sexual activity. The participant also experienced an improvement in bowel management with improved comfort, reduced straining and decreased duration in time required for defecation. When researchers explored further, it was found that the electrode positioning used, was altered from the initial proposed set-up for bowel management (Fig. 1). The two lower electrodes were positioned further down adjacent to the bladder area.
A 36-year-old male who sustained a SCI AIS A, T4/T5 in a road traffic accident 24 months previously, had experienced frequent urinary tract infections in the past and had issues with incomplete emptying of urine. He had received electrical stimulation treatment for 5 months previously. This included upper limb electrical stimulation and lower limb electrical stimulation to elicit dorsiflexion to improve blood flow, build muscle bulk, reduce spasms and improve cosmetic appearance. The 36-year-old had also received electrical stimulation of the quadriceps and gluteal muscles to build up muscle bulk, assist with sitting, improve cosmetic appearance and improve and maintain tissue viability. At the time of treatment with ABFES, he had not received any treatment to improve his sexual functioning.
The 36-year-old was set-up with ABFES using the standard parameters as detailed above and electrode positioning (Fig. 1) to improve bowel transit time, reduce bloating and improve muscle tone and cosmetic appearance. A precheck confirmed autonomic dysreflexia was not elicited from the use of the electrical stimulation.
The 36-year-old reported unexpected improvements in sexual functioning from using ABFES for 26 months. Specifically, he reported an improvement in ejaculation and a tightening of the abdominal muscles and appearance which he felt contributed to his sexual body image. He also reported improvements in bowel transit time and improved urine flow. When researchers explored further, the participant was found to be using the standard electrode positioning and did not report using ABFES during sexual activity.
Discussion
The reported improvements in sexual functioning following the use of ABFES were unexpected and the reasons remain unclear as these were not formally measured. Both participants, reported that they did not use the ABFES treatment during sexual activity; indicating the ABFES was not a direct sexual stimulus. The reported improvements in ejaculatory function for the 36-year-old participant and erectile functioning for the 74-year-old, alongside improvements in bowel and bladder; suggest it is possible that residual supraspinal connections could have been reactivated and strengthened by the electrical stimulation.
Both participants had previously used gluteal electrical stimulation in the past. Gluteal electrical stimulation is consistent with innervation of the S2 level frequently implicated in erectile function. We believe this was not related to current improvements. The 74-year-old had used gluteal electrical stimulation for the last 17 years without any reported benefit to erectile functioning. The 36-year-old had also used gluteal stimulation and reported issues with usability: therefore, he had stopped using it following intermittent use, suggesting that gluteal stimulation may not have been a contributory factor. A further controlled trial is necessary to determine the relative contributions of different interventions.
A further potential explanation is the innervation of the neurologic pathways involved in erectile functioning either directly or e.g. through the pelvic splanchnic nerves or hypogastric plexus originating around T11-L2. The non-standard altered electrode positioning used by the 74-year-old, with the two lower electrodes being positioned further down adjacent to the bladder area, is of interest. While this anterior position may appear far removed from the route of the sacral nerves; with a body of sodium liquid in the bladder and the path of least resistance, the electric field generated may potentially have served to innervate neurologic pathways involved in erectile functioning, either directly or e.g. through the pelvic splanchnic nerves. In contrast, the 36-year-old reported improvements in ejaculatory function and used the standard electrode positioning (Fig. 1). The standard and non-standard electrode set-up are both consistent with innervation of the hypogastric plexus originating around T11-L2. A similar set-up was found to be effective for improved ejaculation in previous case reports during sexual activity [20, 21]. The reported improvements suggest that frequent intensive treatment with ABFES, rather than solely during sexual activity, could potentially lead to a therapeutic effect for erectile as well as ejaculatory functioning.
Further explanations include an improved aesthetic appearance of the abdominal area promoting improved self-esteem and an improved vascularisation of the abdominal area. Both participants attributed the improvements to a strengthening of the muscles in the abdominal area and improved body image. This could be used to suggest that reported improvements could potentially be partially attributed to a combination of improved strengthening and vascularisation of the abdominal area and improved self-esteem.
There is no available data to suggest whether ABFES would be of benefit to women with SCI and sexual dysfunction. Potential benefit to women would be dependent on the presumed underlying mechanism. If improvements reported here can be verified and attributed to e.g. aesthetic appearance and self-image, re-activation of residual networks or improved vascularisation, treatment could be considered and perhaps adapted for women. Further research involving women may also begin to facilitate an understanding of any presumed underlying mechanism due to anatomical differences.
These preliminary findings of reported improved ejaculatory function and erectile function suggest a potential therapeutic effect from ABFES treatment. A controlled trial using standardised measures to assess the use of ABFES, as a tool alongside other interventions for recovery of sexual function is required. Further work is required to assess the use of ABFES as a tool alongside other interventions for recovery of sexual function in SCI. Standardised measures [22,23,24] for sexual and autonomic function should be included in a future controlled trial.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this work.
References
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Hess MJ, Hough S. Impact of spinal cord injury on sexuality: broad-based clinical practice intervention and practical application. J Spinal Cord Med. 2012;35:211–8.
Korsten MA, Fajardo NR, Rosman AS, Creasey GH, Spungen AM, Bauman WA. Difficulty with evacuation after spinal cord injury: colonic motility during sleep and effects of abdominal wall stimulation. J Rehabil Res Dev. 2004;41:95–100.
Hascakova-Bartova R, Dinant J-F, Parent A, Ventura M. Neuromuscular electrical stimulation of completely paralyzed abdominal muscles in spinal cord-injured patients: a pilot study. Spinal Cord. 2008;46:445–50.
Street T, Peace C, Padfield E, Singleton C. Abdominal functional electrical stimulation for bowel management in multiple sclerosis. Neurodegener Dis Manag. 2019;9:83–9.
Benevento T, Sipski M. B. Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther. 2002;82:601–12.
Alexander MS, Marson L. The neurologic control of arousal and orgasm with specific attention to spinal cord lesions: Integrating preclinical and clinical sciences. Auton Neurosci. 2018;209:90–9.
Lombardi G, Musco S, Kessler TM, Li Marzi V, Lanciotti M, Del Popolo G. Management of sexual dysfunction due to central nervous system disorders: a systematic review. BJU Int. 2015;115(Suppl 6):47–56.
Sinha V, Elliott S, Ibrahim E, Lynne CM, Brackett NL. Reproductive health of men with spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23:31–41.
Silva AB, Sousa N, Azevedo LF, Martins C. Physical activity and exercise for erectile dysfunction: systematic review and meta-analysis. Br J Sports Med. 2017;51:1419.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Gater DR. The effects of electrical stimulation on body composition and metabolic profile after spinal cord injury—Part II. J Spinal Cord Med. 2015;38:23–37.
Phillips W, Burkett LN, Munro R, Davis M, Pomeroy K. Relative changes in blood flow with functional electrical stimulation during exercise of the paralyzed lower limbs. Spinal Cord. 1995;33:90–3.
Chilibeck PD, Jeon J, Weiss C, Bell G, Burnham R. Histochemical changes in muscle of individuals with spinal cord injury following functional electrical stimulated exercise training. Spinal Cord. 1999;37:264–8.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR. Effects of spinal cord injury on body composition and metabolic profile—Part I. J Spinal Cord Med. 2014;37:693–702.
Barton TJ, Low DA, Janssen TWJ, Sloots M, Smit CAJ, Thijssen DHJ. Femoral artery blood flow and microcirculatory perfusion during acute, low-level functional electrical stimulation in spinal cord injury. Am J Phys Med Rehabil. 2018;97:721–6.
Creasey GH, Craggs MD. Functional electrical stimulation for bladder, bowel, and sexual function. Handb Clin Neurol. 2012;109:247–57.
Creasey G. Lecture 6 restoration of male sexual function following spinal cord injury. Int J Impot Res. 2000;12:S54–S55.
Harkema S, Gerasimenko Y, Hodes J, Burdick J, Angeli C, Chen Y, et al. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: a case study. Lancet. 2011;377:1938–47.
Adams M, Carlstedt T, Cavanagh J, Lemon RN, McKernan R, Priestley JV, et al. International spinal research trust research strategy. III: a discussion document. Spinal Cord. 2006;45:2.
Goetz LL, Stiens SA. Abdominal electric stimulation facilitates penile vibratory stimulation for ejaculation after spinal cord injury: a single-subject trial. Arch Phys Med Rehab. 2005;86:1879–83.
Kafetsoulis A, Ibrahim E, C Aballa T, Goetz L, Lynne C, Brackett N. Abdominal electrical stimulation rescues failures to penile vibratory stimulation in men with spinal cord injury: a report of two cases. Urology. 2006;204:9–11.
Previnaire JG, Soler JM, Alexander MS, Courtois F, Elliott S, McLain A. Prediction of sexual function following spinal cord injury: a case series. Spinal Cord Ser Cases. 2017;3:17096.
Alexander MS, New PW, Biering-Sørensen F, Courtois F, Popolo GD, Elliott S, et al. International spinal cord injury male sexual function and female sexual and reproductive function basic data sets-version 2.0. Spinal Cord Ser Cases. 2017;3:17050.
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S, et al. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 2009;47:36–43.
Acknowledgements
The authors acknowledge the contribution of Joe Green, Mary Fenn and Earl Merson from the National Clinical FES Centre, Salisbury, UK for administering the ABFES treatment for one of the participants. With thanks to Odstock Medical for providing the use of an electrical stimulator and consumables for treatment of one of the participants. All other treatment was funded by the UK National Health Service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Street, T., Padfield, E. A therapeutic effect for males with spinal cord injury using abdominal functional electrical stimulation for sexual functioning. Spinal Cord Ser Cases 6, 24 (2020). https://doi.org/10.1038/s41394-020-0273-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-020-0273-x