Introduction
Os odontoideum is a rare cervical lesion. This unusual condition is sometimes associated with atlantoaxial subluxation, which is mostly anterior subluxation. Posterior atlantoaxial subluxation due to os odontoideum is extremely rare.
Case presentation
We report an unusual case of a 60-year-old Thai female, who was diagnosed as having chronic posterior atlantoaxial subluxation associated with os odontoideum with progressive myelopathy. The patient underwent posterior arch of C1 laminectomy and an occipito-C3 fusion using an occipital plate, C2 pedicle screws, C3 lateral mass screws and autologous iliac crest strut bone graft arthrodesis. During three years of follow-up, she was clinically significantly improved and postoperative radiographs showed a solid osseous fusion without loss of correction or implant failure.
Discussion
Chronic posterior atlantoaxial subluxation associated with os odontoideum is rare. This condition can cause occipital-cervical pain, myelopathy, intracranial symptoms, or death. Surgical decompression and stabilization is the treatment of choice. Principles of treatment are to prevent sudden death from neurological compromise, improve neurological status, stabilize the cervical spine, and improve quality of life. Surgical options include atlantoaxial fusion, occipito-C2 fusion, and occipito-C3 fusion. Decision making depends on the location of spinal cord compression, area for arthrodesis, and bone quality.
Similar content being viewed by others
Introduction
Os odontoideum, the separation of the odontoid process from the body of the axis, is a rare cervical lesion [1]. The etiology is still controversial, but there is now emerging consensus on the traumatic etiology rather than a congenital source [2, 3]. The incidence of os odontoideum is unknown because the lesion is usually asymptomatic. This unusual condition is sometimes associated with atlantoaxial subluxation, which is mostly anterior subluxation [4]. Posterior atlantoaxial subluxation due to os odontoideum is extremely rare. We present an unusual case of a 60-year-old Thai female, who was diagnosed with chronic posterior atlantoaxial subluxation associated with os odontoideum with progressive cervical myelopathy, which required surgical treatment. Therefore, the objectives are to report this rare condition, to increase awareness of the disease and to review the literatures.
Case presentation
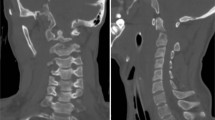
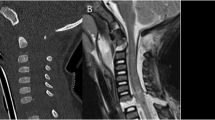
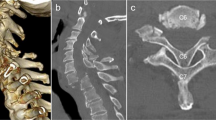
A 60-year-old Thai female was transferred and admitted to our institution with the chief complaint of progressive quadriparesis for 2 months. Three years prior, the patient had begun having posterior axial neck pain and numbness on both upper extremities. A few months later, the symptoms became worse. She had clumsiness on both hands and also difficulty in walking. At a previous hospital, a provisional diagnosis of cervical spondylotic myelopathy was made. She was initially treated with oral medications and physical therapy. The clinical signs were not resolved, therefore, she was subsequently referred to our institution. Physical examination revealed significantly decreased range of motion on her neck with axial neck pain. She developed spastic gait and required standard walkers for ambulation (Nurick scale was grade 4, defined as able to walk only with someone else’s help or with the aid of a frame, mJOA score was 11, defined as severe grading of myelopathy) [5, 6]. Manual muscle testing revealed bilateral generalized muscle weakness markedly at upper extremities (Table 1). Sensory examination showed hypoesthesia in the distribution of bilateral C6 to C8 dermatomes (AIS category C; motor incomplete with a level of injury of C4) [7, 8]. Hyperreflexia was observed. Scapulohumeral (Shimizu) reflex, Tromner reflex, Hoffmann reflex, and Babinski reflex were positive. Her bowel and bladder function were normal. Plain radiographs of the cervical spine revealed generalized osteoarthritis of the cervical spine with os odontoideum and posterior atlantoaxial subluxation (Fig. 1). In addition, dynamic flexion-extension plain radiographs of the cervical spine showed a partial reduction of C1 during flexion position (Fig. 2). Computed tomography scan demonstrated a dystopic type of os odontoideum with posterior atlantoaxial subluxation and generalized anterior osteophyte formation of the vertebral bodies with narrowing of intervertebral disc space. The measurement of posterior atlanto-dens interval (PADI), which is the predictor of the development of paralysis if less than 14, was 12 mm [9] (Fig. 3). Magnetic resonance imaging (MRI) showed high signal within the cord on T2WI from C1 to C2 level with significant spinal cord compression at the same level and generalized anterior osteophyte formation, intervertebral disc height narrowing, and vertebral endplate sclerosis from C2 to C7 levels (grade 3) (Fig. 4). Laboratory findings for serum, urine, and serological test for rheumatoid factor were within the normal limits. After preoperative planning was done, the patient was placed in the prone position with Mayfield’s stabilization and the reduction was carefully performed under the neuromonitoring and confirmed the position with fluoroscopy (Fig. 5). After the reduction was attempted, posterior subluxation was slightly reduced. The measurement of occiput-C3 angle, which is the setting angle for appropriate alignment in occipitocervical instrumentation, was 114 degrees (Occiput-C3 angle is defined as the angle formed by the line drawn from the external occipital protuberance to the tip of superior aspect of the posterior vertebral body of C3 intersection to the line drawn from the posterior aspect of the C3 vertebral body, the normal range of occiput-C3 angle was 94–120 degrees) [10] (Fig. 6). The patient underwent posterior decompression with posterior arch of C1 laminectomy and arthrodesis between occiput and C3 was performed using occipital plate, C2 pedicle screws (Goel’s technique) [11] and C3 lateral mass screws (Magerl’s technique) [12] (Fig. 7). An autologous iliac crest strut bone was harvested and placed between the occiput and C2 (Fig. 8). A four-poster brace was applied for 6 weeks postoperatively and then changed to a soft collar for the next 6 weeks. Three years afterward, the overall clinical and radiological outcomes were improved (Figs. 9 and 10). The patient could walk without support (Nurick scale was grade 1, defined as signs of spinal cord disease but no difficulty in walking, mJOA score was 14, defined as mild grading of myelopathy) [5, 6]. The overall motor power was significantly improved and her International Neurologic Classification of SCI AIS Scale was D [7, 8] (Table 1).
Computed tomographic scan of cervical spine in midsagittal view showed dystopic type of os odontoideum and posterior atlantoaxial subluxation. Anterior osteophyte formation of the vertebral bodies with narrowing of intervertebral disc space. The measurement of PADI, the distance from posterior surface of dens to anterior surface of posterior arch of C1, was 12 mm
Magnetic resonance imaging of T2-weight midsagittal view showed high signal within the cord on T2WI from C1 to C2 level with significant spinal cord compression at the same level and generalized anterior osteophyte formation, intervertebral disc height narrowing, and vertebral endplate sclerosis from C2 to C7 levels (grade 3)
Postoperative computed tomographic scan of cervical spine in midsagittal view (left panel) and postoperative magnetic resonance imaging of T2-weight midsagittal view (right panel) revealed no spinal cord compression at the atlantoaxial area after laminectomy of posterior arch of C1 and iliac crest graft was fused from occiput to the spinous process of axis
Discussion
Os odontoideum, an ossicle with smooth circumferential cortical margins representing the odontoid process that has no osseous continuity with the body of C2 [13], was first published by Giacomini in 1886 [14]. The origin of os odontoideum remains unclear in the literature with the evidence for both congenital and acquired (posttraumatic) causes [15]. The incidence of os odontoideum is unknown because the lesion is usually asymptomatic. Perdikakis et al. [16] retrospectively reviewed the MRI of the odontoid process configuration in 133 patients; and, the incidence of the os odontoideum in their study was 0.7%. Most of the patients with os odontoideum were discovered incidentally. However, specific characteristics or associated abnormalities of os odontoideum have been reported, including atlantoaxial instability, soft-tissue masses, a decrease in spinal canal diameter associated osseous anomalies, and vertebral artery compromise [17]. Atlantoaxial subluxation associated with os odontoideum is a rare condition, which is almost always anterior subluxation. This condition can cause various symptoms such as occipital-cervical pain, myelopathy, intracranial symptoms or signs from vertebrobasilar ischemia [18]. One of the most serious symptoms is cervical myelopathy. These symptoms are thought to be caused by static or dynamic compression of the spinal cord or repeated minor trauma to the spinal cord [19]. Principles of treatment for this condition are to prevent sudden death from neurological compromise, improve neurological status, stabilize the cervical spine, and improve quality of life. The surgical treatment is usually indicated in patients, who had one of the following conditions: neurologic involvement (even if this is transient), instability of more than 5 mm translation, progressive instability, persistent neck complaints associated with atlantoaxial instability and not relieved by conservative treatment [20]. The treatment strategies for this condition can be divided into four steps. First, the main pathology causing the symptoms of myelopathy (i.e., odontoid peg, posterior arch of C1) should be identified. Second, whether the atlantoaxial subluxation is reducible or not should be determined. Third, a decision is made whether the lesion needs to be decompressed or not. Fourth, the surgical option for stabilization and fusion is selected. In previous reports, surgical options treatment for posterior atlantoaxial subluxation due to os odontoideum included atlantoaxial fusion, occipito-C2 fusion, and occipito-C3 fusion [4, 19]. The surgical option depends on the location of spinal cord compression, fusion level, and bone quality. The advantage of atlantoaxial arthrodesis is to preserve the atlanto-occipital joint, which plays an important role of more than 50% of cervical flexion and extension. This procedure is suitable for cases in which complete reduction can be achieved; whereas, an occipitocervical fusion is indicated in the conditions such as occipitocervical instability or failed attempt of atlantoaxial arthrodesis [21, 22]. In this patient, neurological examination suggested the main pathology was cranial to the C3 vertebral level which corresponded to the image findings of os odontoideum with posterior atlantoaxial subluxation and spinal cord signal changes at the same level. First, the posterior atlantoaxial subluxation was restored by closed reduction but this was unsuccessful to obtain complete reduction. Therefore, a decompression at this level was essential and laminectomy of the posterior arch of C1 was performed. The occipito-C3 fusion using an occipital plate, C2 pedicle screws, C3 lateral mass screws and iliac strut bone graft, which is the gold standard for bone grafting in posterior atlantoaxial arthrodesis [23] was chosen for surgical repair. An extended fusion to the occiput was chosen due to the poor bone quality which is one of the risk factors for screw pull-out. By extending the fusion to the occiput instead of a C1–C3 fusion, we increased the stability of the construct. Another reason was, the occipitocervical fusion gave us a better chance of an adequate solid fusion compared to the C1–C3 fusion after laminectomy of the posterior arch of C1 was performed. The reason for extent of fusion to C3 vertebrae was to achieve more rigid construct due to the osteoporotic appearance of the bone. Three years post-surgery, clinical outcomes were significantly improved. The patient had no difficulty in walking (Nurick scale was grade 1, mJOA score was 14) and her overall motor power was significantly improved bilaterally (Table 1).
In conclusion, our case report highlights a rare condition of posterior atlantoaxial subluxation associated with os odontoideum. This condition can cause several serious complications. Surgery is the treatment of choice and selection of the surgical options depends on location of spinal cord compression, fusion level, and bone quality.
References
Robson KA. Os odontoideum: rare cervical lesion. West J Emerg Med. 2011;12:520–2.
Arvin B, Fournier-Gosselin MP, Fehlings M. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66:A22–31.
Klimo PJ, Coon V, Brockmeyer D. Incidental os odontoideum: current management strategies. Neurosurg Focus. 2011;31:E10.
Fielding JW, Hensinger RN, Hawkins RJ. Os Odontoideum. J Bone Jt Surg Am. 1980;62:376–83.
Revanappa KK, Rajshekhar V. Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur Spine J. 2011;20:1545–51.
Tetreault L, Kopjar B, Nouri A, Arnold P, Barbagallo G, Bartels R, et al. The modified Japanese Orthopaedic Association scale: establishing criteria for mild, moderate and severe impairment in patients with degenerative cervical myelopathy. Eur Spine J. 2017;26:78–84.
Kirshblum SC, Burns SP, Biering- Sørensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Krassioukov A, Biering- Sørensen F, Donovan W, Kennelly M, Kirshblum S, Krogh K. et al. International standards to document remaining autonomic function after spinal cord injury. J Spinal Cord Med. 2012;35:202–11.
Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Jt Surg Am. 1993;75:1282–97.
Kunakornsawat S, Pluemvitayaporn T, Pruttikul P, Punpichet S, Piyasakulkaew C, Arirachakaran A. et al. A new method for measurement of occipitocervical angle by occiput C3 angle. Eur J Orthop Surg Traumatol. 2017;27:1051–6.
Ebraheim NA, Rollins JR, Xu R, Jackson WT. Anatomic consideration of C2 pedicle screw placement. Spine. 1996;21:691–5.
Ebraheim NA, Klausner T, Xu R. Safe lateral-mass screw lengths in the Roy-Camille and Magerl techniques. An anatomical study. Spine. 1998;23:1739–42.
Spierings EL, Braakman R. The management of os odontoideum: analysis of 37 cases. J Bone Jt Surg Br. 1982;64:422–8.
Giacomini C. Sull’ esistenza del os odontoideum nell’ uomo. Gior D R Acad di Med Di Torino. 1886;49:24–38.
Stevens JM, Chong WK, Barber C, Kendall BE, Crockard HA. A new appraisal of abnormalities of the odontoid process associated with atlanto-axial subluxation and neurological disability. Brain. 1994;117:133–48.
Perdikakis E, Skoulikaris N. The odontoid process: various configuration types in MR examinations. Eur Spine J. 2014;23:1077–83.
Clements WD, Mezue W, Mathew B. Os odontoideum: congenital or acquired? That’s not the question. Injury. 1995;26:640–2.
Rozzelle CJ, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Ryken TC. et al. Os odontoideum. Neurosurg. 2013;72:159–69.
Shirasaki N, Okada K, Hosono N, Yonenobu K, Ono K. Os odontoideum with posterior atlantoaxial instability. Spine. 1991;16:706–15.
William C W Jr.. Pediatric cervical spine. Campbell’s Oper Orthop Thirteen Ed. 2017;43:1857–77.
Bourdillon P, Perrin G, Lucas F, Debarge R, Barrey C. C1-C2 stabilization by harms arthrodesis: indicaitons, technique, complications and outcomes in a prospective 26-case series. Orthop Traumatol Surg Res. 2014;100:221–7.
Stock GH, Vaccaro AR, Brown AK, Anderson PA. Contemporary posterior occipital fixation. Instr Course Lect. 2007;56:319–28.
Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of anterior and posterior iliac crest bone grafts in term of harvest site morbidity and functional outcomes. J Bone Jt Surg Am. 2002;84:716–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pluemvitayaporn, T., Kunakornsawat, S., Piyaskulkaew, C. et al. Chronic posterior atlantoaxial subluxation associated with os odontoideum: a rare condition. A case report and literature review. Spinal Cord Ser Cases 4, 110 (2018). https://doi.org/10.1038/s41394-018-0143-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-018-0143-y