Abstract
Study design
Systematic review and meta-analysis. Spinal cord injury (SCI) is a pathological condition that provokes the loss of one or more body functions due to an injury to the spinal cord as a result of trauma or disease. Hydrotherapy plays a key role in the rehabilitation of neurological patients due to the properties of water environments.
Objectives
The goal of this study was to evaluate the efficacy of hydrotherapy in patients who suffer from SCIs.
Methods
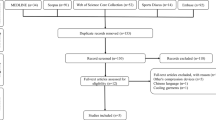
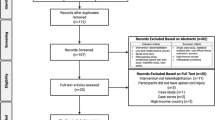
We searched 5 different databases: CINAHL, PubMed, Scopus, Web of Science, and PEDro for studies to include. Only randomized controlled trials (RCTs) published in English were considered. To evaluate the risk of bias, Jadad and PEDro scales were used.
Results
Eleven Randomized Controlled Trials were included, and 3 articles remained to be analyzed. According to the evaluation through Cochrane Risk of Bias tool, one study had a high level of quality. The remaining 2 studies achieved a score indicative of a low level of quality. A total of 71 individuals with SCI were included in the studies; age and level of injury varied in each study. The outcome measures used in the studies were: Functional Independence Measure (FIM), Ashworth scale, CardioTouch 3000 s in sitting position and Quark CPET.
Conclusion
The aquatic environment provides a rehabilitation tool able to facilitate movement, physical and cardiovascular exercise, resistance training, and body relaxation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Dimitrijevic MR, Kakulas BA. Spinal cord injuries, human neuropathology and neurophysiology. Acta Myol. 2020;39:353–8. https://doi.org/10.36185/2532-1900-039.
Ambrozaitis KV, Kontautas E, Spakauskas B, Vaitkaitis D. Pathophysiology of acute spinal cord injury. Med. Kaunas Lith. 2006;42:255–61.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil. 2003;84:1266–75. https://doi.org/10.1016/s0003-9993(03)00234-x.
Celani MG, Spizzichino L, Ricci S, Zampolini M, Franceschini M. Spinal cord injury in Italy: a multicenter retrospective study. Arch Phys Med Rehabil. 2001;82:589–96. https://doi.org/10.1053/apmr.2001.21948.
Laskin JJ, Waheed Z, Thorogood NP, Nightingale TE, and Noonan VK, Spinal cord stimulation research in the restoration of motor, sensory, and autonomic function for individuals living with spinal cord injuries: a scoping review, Arch Phys Med Rehabil. 2022:S0003-9993(22)00234–9. https://doi.org/10.1016/j.apmr.2022.01.161.
Mulroy SJ, Thompson L, Kemp B, Hatchett PP, Newsam CJ, Lupold DG, et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Phys Ther. 2011;91:305–24. https://doi.org/10.2522/ptj.20100182.
Berardi A, Galeoto G, Lucibello L, Panuccio F, Valente D, Tofani M. Athletes with disability’ satisfaction with sport wheelchairs: an Italian cross sectional study. Disabil Rehabil Assist Technol. 2021;16:420–4. https://doi.org/10.1080/17483107.2020.1800114.
Gómara-Toldrà N, Sliwinski M, Dijkers MP. Physical therapy after spinal cord injury: a systematic review of treatments focused on participation. J. Spinal Cord Med. 2014;37:371–9. https://doi.org/10.1179/2045772314Y.0000000194.
Behrman AL, Ardolino EM, Harkema SJ. Activity-based therapy: from basic science to clinical application for recovery after spinal cord injury. J. Neurol. Phys. Ther. 2017;41:S39–S45. https://doi.org/10.1097/NPT.0000000000000184.
Kornhaber R, Mclean L, Betihavas V, Cleary M. Resilience and the rehabilitation of adult spinal cord injury survivors: a qualitative systematic review. J. Adv. Nurs. 2018;74:23–33. https://doi.org/10.1111/jan.13396.
Berardi A, Regoli E, Tofani M, Valente D, Fabbrini G, Fabbrini A, et al. Tools to assess the quality of life in patients with Parkinson’s disease: a systematic review. Expert Rev. Pharmacoecon. Outcomes Res. 2021;21:55–68. https://doi.org/10.1080/14737167.2021.1841638.
Bai C, Ma X. The effects of sacral nerve root electrostimulation on the colon function and its mechanisms in a rat model of spinal cord injury. Zhongguo Ying Yong Sheng Li Xue Za Zhi 2016;32:34–38.
Bajd T, Kralj A, Turk R, Benko H, Sega J. Use of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injuries. J Biomed Eng. 1989;11:96–102. https://doi.org/10.1016/0141-5425(89)90115-5.
van der Scheer JW, Goosey-Tolfrey VL, Valentino SE, Davis GM, Ho CH. Functional electrical stimulation cycling exercise after spinal cord injury: a systematic review of health and fitness-related outcomes. J. Neuroeng Rehabil. 2021;18:99 https://doi.org/10.1186/s12984-021-00882-8.
Aach M, Meindl RC, Geßmann J, Schildhauer TA, Citak M, Cruciger O. [Exoskeletons for rehabilitation of patients with spinal cord injuries. Options and limitations]. Unfallchirurg. 2015;118:130–7. https://doi.org/10.1007/s00113-014-2616-1.
Galeoto G, Formica MC, Mercuri NB, Santilli V, Berardi A, Castiglia SF, et al. Evaluation of the psychometric properties of the Barthel Index in an Italian ischemic stroke population in the acute phase: a cross-sectional study. Funct Neurol. 2019;34:29–34.
Panuccio F, Galeoto G, Marquez MA, Tofani M, Nobilia M, Culicchia G, et al. Internal consistency and validity of the Italian version of the Jebsen–Taylor hand function test (JTHFT-IT) in people with tetraplegia. Spinal Cord. 2021;59:266–73. https://doi.org/10.1038/s41393-020-00602-4.
Amedoro A, Berardi A, Conte A, Pelosin E, Valente D, Maggi G, et al. The effect of aquatic physical therapy on patients with multiple sclerosis: a systematic review and meta-analysis. Mult Scler Relat Disord. 2020;41:102022 https://doi.org/10.1016/j.msard.2020.102022.
Corvillo I, Varela E, Armijo F, Alvarez-Badillo A, Armijo O, Maraver F. Efficacy of aquatic therapy for multiple sclerosis: a systematic review. Eur J Phys Rehabil Med. 2017;53:944–52. https://doi.org/10.23736/S1973-9087.17.04570-1.
Kim E-K, Lee D-K, Kim Y-M. Effects of aquatic PNF lower extremity patterns on balance and ADL of stroke patients. J Phys Ther Sci. 2015;27:213–5. https://doi.org/10.1589/jpts.27.213.
Cugusi L, Manca A, Bergamin M, Di Blasio A, Monticone M, Deriu F, et al. Aquatic exercise improves motor impairments in people with Parkinson’s disease, with similar or greater benefits than land-based exercise: a systematic review. J Physiother. 2019;65:65–74. https://doi.org/10.1016/j.jphys.2019.02.003.
Yadegaripour M, Sadeghi H, Shojaedin SS, Shamsehkohan P. Effects of a combined aquatic-nonaquatic training program on static and dynamic balance in elderly men. J Am Geriatr Soc. 2013;61:1417–9. https://doi.org/10.1111/jgs.12390.
Guthrie TC, Nelson DA. Influence of temperature changes on multiple sclerosis: critical review of mechanisms and research potential. J Neurol Sci. 1995;129:1–8. https://doi.org/10.1016/0022-510x(94)00248-m.
Jentoft ES, Kvalvik AG, Mengshoel AM. Effects of pool-based and land-based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Rheum. 2001;45:42–47. 10.1002/1529-0131(200102)45:1<42:AID-ANR82>3.0.CO;2-A
Veldema J, Jansen P. Aquatic therapy in stroke rehabilitation: systematic review and meta-analysis. Acta Neurol Scand. 2021;143:221–41. https://doi.org/10.1111/ane.13371.
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions, 2nd ed. Hoboken, NJ Chichester: Wiley Blackwell; 2019.
Clark HD, Wells GA, Huet C, McAlister FA, Salmi LR, Fergusson D, et al. Assessing the quality of randomized trials. Control Clin Trials. 1999;20:448–52. https://doi.org/10.1016/S0197-2456(99)00026-4. ott
Kesiktas N, Paker N, Erdogan N, Gülsen G, Biçki D, Yilmaz H. The use of hydrotherapy for the management of spasticity. Neurorehabil Neural Repair. 2004;18:268–73. https://doi.org/10.1177/1545968304270002.
Kidd D, Stewart G, Baldry J, Johnson J, Rossiter D, Petruckevitch A, et al. The functional independence measure: a comparative validity and reliability study. Disabil Rehabil. 1995;17:10–14. https://doi.org/10.3109/09638289509166622.
Kohan AH, Abootalebi S, Khoshnevisan A, Rahgozar M. Comparison of modified Ashworth scale and Hoffmann reflex in study of spasticity. Acta Med Iran. 2010;48:154–7.
Jung J, Chung E, Kim K, Lee B-H, Lee J. The effects of aquatic exercise on pulmonary function in patients with spinal cord injury. J Phys Ther Sci. 2014;26:707–9. https://doi.org/10.1589/jpts.26.707.
Nieman DC, Austin MD, Dew D, Utter AC. Validity of COSMED’s Quark CPET mixing chamber system in evaluating energy metabolism during aerobic exercise in healthy male adults. Res Sports Med. 2013;21:136–45. https://doi.org/10.1080/15438627.2012.757227.
Gorman PH, Scott W, VanHiel L, Tansey KE, Sweatman WM, Geigle PR. Comparison of peak oxygen consumption response to aquatic and robotic therapy in individuals with chronic motor incomplete spinal cord injury: a randomized controlled trial. Spinal Cord. 2019;57:471–81. https://doi.org/10.1038/s41393-019-0239-7.
Basmajian JV. Therapeutic exercise in the management of rheumatic diseases. J Rheumatol Suppl. 1987;14:22–25.
McNeal RL. Aquatic therapy for patients with rheumatic disease. Rheum Dis Clin N Am. 1990;16:915–29.
Li D, Chen P. Effects of aquatic exercise and land-based exercise on cardiorespiratory fitness, motor function, balance, and functional independence in stroke patients-a meta-analysis of randomized controlled trials. Brain Sci. 2021;11:1097 https://doi.org/10.3390/brainsci11081097.
Van Houtte S, Vanlandewijck Y, Gosselink R. Respiratory muscle training in persons with spinal cord injury: a systematic review. Respir Med. 2006;100:1886–95. https://doi.org/10.1016/j.rmed.2006.02.029.
Sheel AW, Reid WD, Townson AF, Ayas NT, Konnyu KJ, Spinal Cord Rehabilitation Evidence Research Team. Effects of exercise training and inspiratory muscle training in spinal cord injury: a systematic review. J. Spinal Cord Med. 2008;31:500–8. https://doi.org/10.1080/10790268.2008.11753645.
Thomaz SR, Cipriano G Jr, Ferreira Formiga M, Fachin-Martins E, Bernardelli Cipriano GF, Rodrigues Martins W, et al. Effect of electrical stimulation on muscle atrophy and spasticity in patients with spinal cord injury - a systematic review with meta-analysis. Spinal Cord. 2019;57:258–66. https://doi.org/10.1038/s41393-019-0250-z.
Stampas A, Hook M, Korupolu R, Jethani L, Kaner MT, Pemberton E, et al. Evidence of treating spasticity before it develops: a systematic review of spasticity outcomes in acute spinal cord injury interventional trials. Ther Adv Neurol Disord. 2022;15:17562864211070656 https://doi.org/10.1177/17562864211070657.
Zughbor N, Alwahshi A, Abdelrahman R, Elnekiti Z, Elkareish H, Gabor MG, et al. The effect of water-based therapy compared to land-based therapy on balance and gait parameters of patients with stroke: a systematic review. Eur Neurol. 2021;84:409–17. https://doi.org/10.1159/000517377.
de A. Barbosa PHF, Glinsky JV, Fachin-Martins E, Harvey LA. Physiotherapy interventions for the treatment of spasticity in people with spinal cord injury: a systematic review. Spinal Cord. 2021;59:236–47. https://doi.org/10.1038/s41393-020-00610-4.
Iatridou G, Pelidou HS, Varvarousis D, Stergiou A, Beris A, Givissis P, et al. The effectiveness of hydrokinesiotherapy on postural balance of hemiplegic patients after stroke: a systematic review and meta-analysis. Clin Rehabil. 2018;32:583–93. https://doi.org/10.1177/0269215517748454.
Furlan JC, Noonan V, Singh A, Fehlings MG. Assessment of disability in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma. 2011;28:1413–30. https://doi.org/10.1089/neu.2009.1148.
Platz T, Eickhof C, Nuyens G, Vuadens P. Clinical scales for the assessment of spasticity, associated phenomena, and function: a systematic review of the literature. Disabil Rehabil. 2005;27:7–18. https://doi.org/10.1080/09638280400014634.
Ellapen TJ, Hammill HV, Swanepoel M, Strydom GL. The benefits of hydrotherapy to patients with spinal cord injuries. Afr J Disabil. 2018;7:450 https://doi.org/10.4102/ajod.v7i0.450.
Author information
Authors and Affiliations
Contributions
LP and IR were responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analyzing data, interpreting results, updating reference lists, and creating tables. GG and AB were responsible for designing the review protocol and screening potentially eligible studies. They contributed to writing the report, extracting and analyzing data, interpreting results and creating tables. AC contributed to data extraction and provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palladino, L., Ruotolo, I., Berardi, A. et al. Efficacy of aquatic therapy in people with spinal cord injury: a systematic review and meta-analysis. Spinal Cord 61, 317–322 (2023). https://doi.org/10.1038/s41393-023-00892-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00892-4