Abstract
Study design
Longitudinal cohort study.
Objectives
To investigate the longitudinal effects of time since injury and age at injury on outcomes of quality of life, physical function, secondary conditions and participation, in people with traumatic spinal cord injury (SCI).
Setting
Community resident people with spinal cord injury in Queensland, Australia.
Methods
A baseline sample of 270 people with SCI was recruited. Telephone surveys on measures of quality of life (WHOQOL-Bref), secondary conditions (Secondary Conditions Surveillance Instrument, subset), physical functioning (Functional Independence Measure motor subscale) and participation (Community Integration Measure) were conducted each year between 2004 and 2008, and again in 2018. Random-effect within-between models were used to determine the effect of time since injury and age at injury on each outcome variable. Inverse probability-of-censoring weights were used to correct for selection bias.
Results
There was an effect of time since injury on secondary conditions, with a one-year change associated with 9% higher odds of having worse Secondary Conditions Surveillance Instrument scores (odds ratio = 1.09, 95% confidence interval = 1.02, 1.17; p = 0.006). We did not find any evidence of a time since injury effect on quality of life, physical function, or participation. Similarly, we did not find any evidence of an age at injury effect on any outcome variable.
Conclusions
Secondary conditions may increase with longer time since injury among people with SCI, suggesting appropriate formal and informal supports are required to minimise the impact of these emerging health problems as individuals age.
Similar content being viewed by others
Introduction
Human function is described in the International Classification of Functioning Disability and Health (ICF) as a ‘dynamic interaction between a person’s health condition, environmental factors and personal factors’ [1]. Thus, a person with a persisting condition such as traumatic spinal cord injury (SCI) may experience a change in function over time as the intrinsic and extrinsic influencing factors are unlikely to remain constant. Several research groups have endeavoured to uncover patterns of change over time, to help predict and comprehensively plan for the needs of people with SCI as they age [2,3,4,5].
Researchers have highlighted that the interactions between physiological ageing and SCI are complex [3, 5]. Still, there are suggestions that people with SCI may age more rapidly both biologically and functionally [6]. Adding to the complexity is a broad trend suggesting that the age of SCI onset is also shifting, trending towards older age at the time of injury [7]. Some research suggests that people who experience SCI onset at an advanced age are more likely to experience a more rapid decline in function [8], possibly due to decreased capacity for physical adaptability when age related changes are already present [9]. Others suggest that age at onset may have a greater influence on participation than physical function or secondary conditions [10].
Equally, time since injury is an important factor to consider. Research suggests that quality of life for people with SCI remains comparatively stable over time [4, 10, 11], albeit at a level which is significantly lower than population norms [11]. Physical function however may display a more varied trajectory. Some research suggests that physical function remains quite stable or improves during the first 20 to 25 years following injury, followed by a decline in function during latter years [3, 4]. A study by Gerhart et al. [12] examining self-reported changes in physical function over time in a British cohort of 279 individuals, found that participants with cervical level injuries required increased care support at a younger age than those with lower-level injuries. In a retrospective study conducted with an Australian cohort of people with long duration SCI, 27% reported a decline in mobility and 26% reported a decrease in their ability to perform self-care over time [13]. This study also suggested that those with tetraplegia and those with neurologically incomplete injuries showed a more marked decrease in physical function compared with participants with paraplegia [13].
Secondary health conditions following SCI have rarely been investigated as an outcome per se and there is a need to track the course of these conditions over time and the implications for people’s experience of disability over the long term [14]. Studies have generally described the negative influence of secondary conditions on long-term outcomes for people with SCI [9, 15, 16]. The contributory impact of age on the severity and functional consequences of secondary conditions after SCI has also been noted [9, 15, 17]. Indeed, secondary conditions associated with SCI, such as musculoskeletal pain, pressure injuries, spasticity and bowel management issues have been associated with a lower quality of life [15].
While a subtle decline in (objective) participation seems to be a feature of ageing with SCI, the subjective experience is more mixed [18]. Previous research has revealed an increase in participation with increasing time since injury but not when adjusted for impairment, income, and social situation [4]. It is likely that participation will increase with time, as knowledge, skills and networks of support are developed. However, declining health and increasing secondary conditions [4] compounded by the presence of barriers to community access [19] may be compromising factors.
To ensure appropriate timing and availability of services and supports across the lifespan for people with traumatic SCI, accurate information regarding how outcomes change over time and in relation to age at onset is needed [20]. Therefore, the purpose of the current study was to investigate the longitudinal effects of time since injury and age at injury on change in outcomes of quality of life, physical function, secondary conditions, and participation.
Methods
Design
The study followed a longitudinal cohort design, with people with SCI followed over a 15-year period. Building on an initial 5-year data collection between 2004 and 2008 [4], participants were contacted in 2018, 10 years after the initial data collection period. Participants were invited to take part in a telephone survey, focusing on measures of quality of life, secondary conditions, physical functioning, and participation. These survey tools are described below. The same research assistant (physiotherapist) who collected most of the original survey data between 2004 and 2008 was responsible for data collection in 2018. The 2018 surveys were completed over a period of 35 weeks, with each telephone call taking between 10 and 35 min to complete. The protocol for this study was approved by the Metro South Health Human Research Ethics Committee (HREC/17/QPAH/819). As this was a cohort study, the STROBE guidelines for cohort studies were followed for reporting purposes.
Setting
The study was conducted with community resident persons with traumatic SCI in Queensland, Australia.
Participants
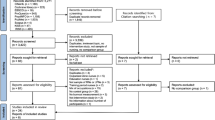
A longitudinal survey of people with traumatic SCI was conducted from 2004 to 2008 with data collected annually. The sample for the preliminary study has been reported in previous articles [4, 11]. It used a wave panel design, with 270 participants with SCI randomly selected from archival records of the Queensland Spinal Cord Injuries Service (QSCIS). In the initial study, participants were recruited in time since injury strata. This approach ensured a representative distribution of participants with a time since injury, ranging from 0 years to more than 25 years. In the current study, we treated time since injury as a continuous variable, rather than according to the six strata used in the original investigation [4, 11].
Participant demographic and injury-related characteristics are reported in Table 1. Over the course of the study, the total attrition rate was 42.6% (115/270) with 14.4% (39/270) due to death. The attrition rate during the period of yearly data collection between 2004 and 2008 was 13.3% (n = 36/270; 2.6% due to death). Of the 234 individuals who completed the surveys in 2008, 222 agreed to future contact from the researchers with 155 completing the final survey in 2018. The attrition rate between 2008 and 2018 was 29.3% (79/270) with 11.8% (32/270) deceased. Of those deceased, the majority (28/32) had a time since injury of 15 years or more.
Measures
Demographic details were drawn from self-report within the survey and injury characteristics were drawn from archival medical records. Primary impairments were measured according to neurological level and completeness of injury, based on the American Spinal Injury Association (ASIA) classification system. Functionally complete injuries were those classified as ASIA A, B or C. Functionally incomplete injuries were those with neurological sparing (ASIA D) such that ambulation is typically possible.
Quality of life was measured using the World Health Organisation’s Quality of Life Instrument (WHOQOL)-Bref [21]. This self-report measure assesses perceived quality of life over the preceding 2 weeks on 26 items and has been previously used in SCI populations. For the current study, the scale was used in two ways; (a) using the two global items ‘how would you rate your quality of life’ and ‘how satisfied are you with your health’ and (b) across the four domain subscales (Physical, Psychological, Social and Environment).
The ICF outlines three components of human function––body structure/function, activity, and participation. Measures were chosen to reveal changes across these three components. Body structure/function was measured using a subset of the self-report Secondary Conditions Surveillance Instrument (SCSI) [22]. The full SCSI (range, 0–120) measures the severity of secondary conditions or problems experienced over the past year across 40 items on a 4-point scale from 0 (no problem) to 3 (significant problem). The 15-item subset (range, 0–45) selected for this study included those items that were identified as prevalent and relevant to people with SCI. This included items related to pressure sores, posture, bladder and bowel function, dysreflexia and fatigue as well as cardiovascular, circulatory and respiratory problems. The SCSI pain item was not included as a question as a pain item exists within the WHOQOL-Bref. Higher scores on the SCSI indicate more significant problems associated with secondary conditions.
The motor subscale of the Functional Independence Measure (mFIM) was used to measure activity [23]. The mFIM (range 7–91) rates functional independence on a scale of one to seven across 13 items and has proved valid and reliable when administered by telephone to people with SCI [24]. Higher scores indicate higher functional independence.
Participation was measured with the Community Integration Measure (CIM) [25], a psychometrically sound measure of community integration when used in the SCI population [26]. The CIM (range 10–50) assesses perception of connection with community on a 5-point scale from 1 (always disagree) to 5 (always agree) across 10 items. Higher scores indicate greater community integration.
Analysis
All analyses were performed in R (version 4.0.3). Our primary interest was to investigate the effects of time since injury and age at injury on outcomes of quality of life, secondary conditions, physical functioning, and participation. All models included year, injury level, completeness, time since injury, age at injury, and whether individuals lived alone (living status) as fixed effects. Because year and time since injury were correlated, within-between estimation was used to model time since injury, separating inter-individual variation (i.e. between-subject effects) and intra-individual change (i.e. within-subject effects) across the six measurement points (i.e. 2004–2008, and 2018)—with the intra-individual change the effect of interest [27]. See Appendix 2.2 in Reinhardt et al. [28] for an explanation of between-within estimation. All models included inverse probability-of-censoring weights as a fixed effect, to correct for potential bias induced by loss to follow-up [29]. Inverse probability-of-censoring weights are based on an estimate of how loss to follow-up depends on observed baseline and time-updated participant characteristics. Weights were calculated using the R package mets [30], with injury level, completeness, gender, age at injury, and time since injury (separated for within-subject and between-subject effect) included in the model. All models included a random intercept and slope (year) for each participant in the study.
Ordinal regression was used to model ratings of WHOQOL-Bref QOL and Health Satisfaction. Stan [31] with the brms interface [32] was used to fit a cumulative model and an adjacent category model [33] with the best fitting model selected based on the smallest Leave-One-Out Information Criterion. Weakly informative prior distributions were set for the regression coefficients and variance parameters [34]. A Gaussian (mean 0, standard deviation 1) prior distribution was used for the regression coefficients, and a t-distribution (df 3, mean 0, scale 2.5) prior for the standard deviation of the random effects. In this setting, the prior distribution on the fixed effects has a 95% interval of −1.95 and 1.95—equivalent to an odds ratio of 0.14 and 7.03, respectively. Posterior estimates were generated using Markov chain Monte Carlo methods (16,000 iterations, with a 50% burn-in) and are reported as the mean and 95% credible interval.
WHOQOL-Bref Physical, Psychological, Social and Environment data were modelled with a Gaussian response distribution, and SCSI with a Poisson response distribution. These models were fit using the R package panelr [35]. mFIM and CIM data were modelled with a beta response distribution, which assumes a continuous, interval-level response variable, with known bounds [36]. The beta distribution is highly flexible and can accommodate heteroscedasticity and skewed errors [36]. mFIM and CIM scores were rescaled to lie within the (0, 1) interval using the equation: y’ = (y − a)/(b − a), where ‘a’ is the minimum possible questionnaire score, ‘b’ the maximum possible score, and ‘y’ the observed score. Because the beta distribution cannot take responses that are exactly one, ones were shifted off the boundary by or subtracting 0.00001 [36]. This has no impact on scores when back transformed to the original scale. Beta regression models were fit using the mgcv package [37].
Data are reported as the mean and 95% confidence interval (CI), unless otherwise stated. The α level for all tests was set at 5%. The R code used to generate the study findings can be found at https://github.com/SciBorgo/longterm-function-sci-qld.
Results
The main finding of the study was that a longer time since injury was associated with more secondary conditions, with a 1-year change associated with 9% higher odds of having worse SCSI scores. We did not find any evidence that time since injury or age at injury had an effect on any of the other studied outcome variables. The study results are described in further detail below.
WHOQOL-Bref global QOL ratings are shown in Fig. 1; and Health Satisfaction ratings in Fig. 2. The cumulative ordinal model was a better fit compared to the adjacent category model for global QOL (Leave-One-Out Information Criterion = 2587 versus 2631) and Health Satisfaction (Leave-One-Out Information Criterion = 2906 versus 2944). There was no evidence of time since injury or age at injury effects on global QOL or Health Satisfaction (Supplementary 1).
Figure 3 shows WHOQOL-Bref scores on the Physical, Psychological, Social and Environment QOL subscales. There was no evidence of time since injury or age at injury effects on Physical, Psychological, Social and Environment QOL scores (Supplementary 2). There was, however, evidence that participants living with others had higher Social QOL scores compared to those who lived alone (β = 7.2, 95% CI = 4.4, 10.1, p < .001). It was unclear whether there was an effect of year on Psychological QOL scores (β = 1.60, 95% CI = −0.05, 3.26, p = 0.058).
Secondary Conditions Surveillance Instrument scores are shown in Fig. 4. A longer time since injury (within-subject effect) was associated with more secondary conditions (β logit = 0.09, 95% CI = 0.3, 1.5, p = 0.006), with a 1-year change associated with 9% higher odds of worse (i.e. higher) SCSI scores (odds ratio [OR] = 1.09, 95% CI = 1.02, 1.17). There was also an effect of year on SCSI scores (β logit = −0.07, 95% CI = −0.13, −0.01, p = 0.025), with each year after 2004 associated with a 7% reduction in SCSI scores (OR = 0.93, 95% CI = 0.88, 0.99). We also found evidence that participants with an incomplete injury had fewer secondary conditions compared to those with a complete injury (mean difference = −2.0, 95% CI = −3.6, −0.4, p = 0.011). Analysis was not conducted at the item level. However, descriptively the highest aggregate impact on life (as worded in the scale itself) was noted for items related to fatigue, physical fitness, spasm, bladder and bowel problems. Therefore, these were the items that scored highest.
Figure 4 shows mFIM scores. There was no evidence of time since injury or age at injury effects on physical function. Participants with tetraplegia had lower physical function compared to those with paraplegia (mean difference = −15, 95% CI = −17, −13, p < 0.001). Participants with an incomplete injury had higher physical function than those with a complete injury (mean difference = 20, 95% CI = 18, 22, p < 0.001). Participants who lived with others also had higher physical function than those who lived alone (mean difference = 2.2, 95% CI = 0.1, 4.3, p = 0.041). CIM scores are displayed in Fig. 4. There was no evidence of time since injury or age at injury effects on participation as measured by the CIM (Supplementary 2).
Discussion
This study aimed to examine the effects of time since injury and age at injury on outcomes of quality of life, physical function, secondary conditions, and participation. We found evidence that a longer time since injury was associated with more problems related to secondary conditions (OR = 1.09, 95% CI = 1.02, 1.17). We did not find any evidence of a time since injury effect on quality of life, physical function or participation, and no evidence of an age at injury effect on any outcome variable. Appropriate formal and informal supports are required to minimise the impact of these emerging health problems as individuals age with their injury.
While these findings suggest greater health problems arising from a SCI over time since injury, there did not appear to be parallel changes in quality of life, physical function, and participation. Existing literature suggests that the increased experience of secondary conditions impacts other outcomes including quality of life and participation [9, 15, 16, 19]. This was not evident in our findings. While the current study supports previous work noting little change in quality of life [11, 38] and participation [18] over time since injury, changes in physical function, particularly for those with higher level injuries, which has been shown in previous studies [3, 4, 12], were not evident.
Our findings are encouraging and may reflect the Australian service context for people with SCI. In Queensland, where the study was conducted, a statewide all-of-life continuity of care service model exists for people with SCI. This is supported by a national public health system. Collectively, these service models provide a unique combination of formal supports for individuals with SCI across the lifespan. Improvements in service models and delivery between 2004 and 2018 could partly explain why we found an effect of year on secondary conditions, with each year after 2004 associated with a 7% reduction in SCSI scores. Given the recent introduction of a National Disability Insurance Scheme (NDIS) providing access to formal supports and funding, the impact of secondary health conditions experienced with aging may be further diminished [38]. Future research is needed to examine these outcomes through comparison with population norms and within the context of the NDIS. Ultimately, parity in quality of life and participation, regardless of injury, would be the most desirable goal.
We did not identify any association between age at injury onset and any of the studied outcomes. This contradicts previous research [6, 8,9,10]. It is possible that the measures used in the current study were not sufficiently sensitive to detect any changes attributed to age at injury onset. There was also a relatively narrow interquartile range for age at injury in this cohort which may be explanatory. However, we did observe expected differences, such as higher physical function among those with paraplegia and incomplete injuries, which could indicate that the included measures were appropriately sensitive.
The current study found that living with at least one other person was associated with better social QOL and higher physical function. It is unclear whether individuals were living with others because they have better social QOL or physical function, or whether these outcomes were improved because participants were living with others. Regardless of the causal mechanisms, the social support available through informal supports may be particularly important for both social and physical function, a finding consistent with existing literature [39]. When assessing individuals for formal supports, it may be necessary to consider the living situations of people with SCI as they age and adjust supports accordingly.
Limitations and future research
Our results may not be generalisable to all people with SCI. While accounted for in the data analysis, there was an attrition rate over the study duration of 42.6%. This highlights the challenges of conducting longitudinal research in this area. Study attrition, and the use of inverse probability-of-censoring weights, explains the large uncertainty on estimates in 2018 relative to the years 2004–2008. This uncertainty is reflected by much wider confidence intervals on all outcome measures presented in Figs. 3, 4. The large uncertainty on point estimates in 2018 likely explains why we did not find an effect of year on most outcomes (other than secondary conditions), despite seemingly lower or higher mean values in 2018 compared to the years 2004–2008 (e.g. community integration measure, Fig. 4). The current study was limited in the range of predictive/risk factors considered. It is feasible that other factors not taken into consideration may have influenced the findings over the 15-year-data collection period. Further research that explores the evolution of specific secondary conditions would be useful in targeting resources.
The current study provides limited insight into the individual experience of changes in quality of life, physical function, secondary conditions, and participation as it relates to time since injury and age at onset for people with SCI. Greater attention to qualitative investigations may provide greater understanding of people’s realities, their experiences, and the meanings they attribute to these issues in their lives.
Conclusion
We found evidence that secondary conditions associated with SCI increased with a longer time since injury. However, the increase in secondary conditions did not appear to affect quality of life, physical function, or participation. The formal assistance provided by an appropriate and resourced health system combined with the informal support of living with others may be particularly beneficial for people with SCI as they age. Future research exploring secondary conditions for people with SCI as they live longer with their injury is warranted.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request. The R code used to generate the study findings can be found at https://github.com/SciBorgo/longterm-function-sci-qld.
References
World Health Organization. How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF). Exposure draft for comment. Geneva, Switzerland: WHO; 2013.
Jörgensen S, Iwarsson S, Norin L, Lexell J. The Swedish aging with spinal cord injury study (SASCIS): Methodology and initial results. PMR. 2016;8:667–77.
Krause JS, Clark JMR, Saunders LL. SCI longitudinal aging study: 40 years of research. Top Spinal Cord Inj Rehabil. 2015;21:189–200.
Pershouse KJ, Barker RN, Kendall MB, Buettner PG, Kuipers P, Schuurs SB, et al. Investigating changes in quality of life and function along the lifespan for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:413–9.
Savic G, Charlifue S, Glass C, Soni B, Gerhart K, Ali J. British ageing with SCI study: changes in physical and psychosocial outcomes over time. Top Spinal Cord Inj Rehabil. 2010;15:41–53.
Pili R, Gaviano L, Pili L, Petretto DR. Ageing, disability and spinal cord injury: some issues of analysis. Curr Gerontol Geriatr Res. 2018. https://doi.org/10.1155/2018/4017858.
Kern SB, Hunter LN, Sims AC, Berzins D, Riekena H, Andrews ML, et al. Understanding the changing health care needs of individuals aging with spinal cord injury. Top Spinal Cord Inj Rehabil. 2019;25:62–73.
Rodakowski J, Skidmore ER, Anderson SJ, Begley A, Jensen MP, Buhule OD, et al. Additive effect of age on disability for individuals with spinal cord injuries. Arch Phys Med Rehabil. 2014;95:1076–82.
Molton IR, Terrill AL, Smith AE, Yorkston KM, Alschuler KN, Ehde DM, et al. Modeling secondary health conditions in adults aging with physical disability. J Aging Health. 2014;26:335–59.
Post MWM, Reinhardt JD. Participation and life satisfaction in aged people with spinal cord injury: Does age at onset make a difference? Top Spinal Cord Inj Rehabil. 2015;21:233–40.
Barker RN, Kendall MD, Amsters DI, Pershouse KJ, Haines TP, Kuipers P. The relationship between quality of life and disability across the lifespan for people with spinal cord injury. Spinal Cord. 2009;47:149–55.
Gerhart KA, Bergstrom E, Charlifue SW, Menter RR, Whiteneck GG. Long-term spinal cord injury: functional changes over time. Arch Phys Med Rehabil. 1993;74:1030–4.
Amsters DI, Pershouse KJ, Price GL, Kendall MB. Long duration spinal cord injury: perceptions of functional change over time. Disabil Rehabil. 2005;27:489–97.
Moharić M. Research on prevalence of secondary conditions in individuals with disabilities: an overview. Int J Rehabil Res. 2017;40:297–302.
Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51:882–92.
Adriaansen JJE, Ruijs LEM, van Koppenhagen CF, van Asbeck FWA, Snoek GJ, van Kuppevelt D, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med. 2016;48:853–60.
Hitzig SL, Campbell KA, McGillivray CF, Boschen KA, Craven BC. Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord. 2010;48:330–5.
de Ruijter LS, de Groot S, Adriaansen JJ, Smit CA, Post MWM. Associations between time since onset of injury and participation in Dutch people with long-term spinal cord injury. Spinal Cord. 2018;56:1134–43.
Reinhardt JD, Ballert C, Brinkhof MWG, Post MWM. Perceived impact of environmental barriers on participation among people living with spinal cord injury in Switzerland. J Rehabil Med. 2016;48:210–8.
Boschen KA, Tonack M, Gargaro J. Long-term adjustment and community reintegration following spinal cord injury. Int J Rehabil Res. 2003;26:157–64.
Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A Report from the WHOQOL Group. Qual Life Res. 2004;13:299–310.
Seekins T, Smith N, McCleary T, Clay J, Walsh J. Secondary disability prevention: Involving consumers in the development of a public health surveillance instrument. Disabil Policy Stud. 1991;1:21–38.
Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: A quantitative review. Arch Phys Med Rehabil. 1996;77:1226–32.
Masedo AI, Hanley M, Jensen MP, Ehde D, Cardenas DD. Reliability and validity of a Self-Report FIM (FIM-SR) in persons with amputation or spinal cord injury and chronic pain. Am J Phys Med Rehabil. 2005;84:167–76.
McColl MA, Davies D, Carlson P, Johnston J, Minnes P. The community integration measure: Development and preliminary validation. Arch Phys Med Rehabil. 2001;82:429–34.
De Wolf A, Lane-Brown A, Tate RL, Middleton J, Cameron ID. Measuring community integration after spinal cord injury: validation of the Sydney psychosocial reintegration scale and community integration measure. Qual Life Res. 2010;19:1185–93.
Bell A, Jones K. Explaining fixed effects: random effects modeling of time-series cross-sectional and panel data. Political Sci Res Methods. 2015;3:133–53.
Reinhardt JD, Fellinghauer CS, Post MWM. Change in environmental barriers experienced over a 5-year period by people living with spinal cord injury in Switzerland: a prospective cohort study. Spinal Cord. 2021;59:441–51.
Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJ Jr. Selection bias due to loss to follow up in cohort studies. Epidemiology. 2016;27:91–7.
Holst KK, Scheike TH, Hjelmborg JB. The liability threshold model for censored twin data. Comput Stat Data Anal. 2016;93:324–35.
Stan Development Team. RStan: the R interface to Stan. R package version 2.21.2. 2020. http://mc-stan.org.
Bürkner P. brms: an R package for bayesian multilevel models using Stan. J Stat Softw. 2017;80:1–28.
Bürkner PC, Vuorre M. Ordinal regression models in psychology: a tutorial. Adv Methods Pract Psychol Sci. 2019;2:77–101.
Gelman A, Carlin JB, Stern HS, Rubin DB. Bayesian data analysis. Chapman and Hall/CRC; Oxford, United States: 1995.
Long JA. panelr: Regression models and utilities for repeated measures and panel data. R package version 0.7.3, 2020. https://cran.r-project.org/package=panelr.
Smithson M, Verkuilen J. A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychol Methods. 2006;11:54.
Wood SN. Stable and efficient multiple smoothing parameter estimation for generalized additive models. J Am Stat Assoc. 2004;99:673–86.
Callaway L, Barclay L, McDonald R, Farnworth L, Casey J. Secondary health conditions experienced by people with spinal cord injury within community living: Implications for a National Disability Insurance Scheme. Aust Occup Ther J. 2015;62:246–54.
Müller R, Peter C, Cieza A, Geyh S. The role of social support and social skills in people with spinal cord injury—a systematic review of the literature. Spinal Cord. 2012;50:94–106.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
MK: Planning the study, interpretation of data, drafting of paper. DA: Planning the study, interpretation of data, drafting of paper. SS: Planning the study, collecting data, drafting of paper. DB: Planning of study, data analysis, interpretation of data, drafting of paper. KP: Planning the study, interpretation of data, drafting of paper. PK: Planning the study, interpretation of data, drafting of paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by Metro South Health Human Research Ethics Committee, reference number HREC/17/QPAH/819. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kendall, M.B., Amsters, D., Schuurs, S. et al. Longitudinal effects of time since injury and age at injury on outcomes of people with spinal cord injury in Queensland, Australia. Spinal Cord 60, 1087–1093 (2022). https://doi.org/10.1038/s41393-022-00824-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00824-8